Sepsis is a life threatening organ dysfunction caused by exaggerated response of our immune system to an infection and septic shock is a situation where there is profound circulatory failure in the form of decrease in vascular tone with some degree of hypovolemia and is associated with a greater risk of mortality [1]. The organ dysfunction due to sepsis is manifested as acute rise in 2 points in qSOFA score from baseline and is assessed by: 1) SBP ≤100 mmHg; 2) RR ≥ 22/min; 3) altered mentation [1]. In sepsis, complex chain of events occur involving inflammatory and anti-inflammatory processes, humoral and cellular reactions, and circulatory abnormalities [2,3]. Sepsis is the leading cause of death worldwide in critically ill patients in spite of modern antibiotics and resuscitation measures [4,5]. To predict the outcome, an early diagnosis and stratification of severity of the sepsis is important [6,7]. The magnitude of mortality in sepsis is high in low income countries due to lack of essential drugs, understaffed and underfunded health care systems [8]. Hence, it becomes important in identifying sepsis and predicting the likely outcome at the earliest to prioritise available resources. Predictive mortality scores permit the identification of patients requiring special attention on admission [9,10]. For predicting the outcome of sepsis at the earliest many scoring systems like SOFA, APACHE II, REMS, MPM have been developed [10]. However, the use of certain scores like SOFA and APACHE II requires more laboratory parameters such as Arterial Blood Gas (ABG) analysis, serum bilirubin, serum creatinine, total platelet counts repeatedly, which are not possible in resource poor hospitals [8-12]. Resource limited settings need simple and cost-effective clinical scores which can ensure rapid identification of patients requiring critical care [13]. Simple and feasible scoring system like REMS score comprises simple variables like, age in years, PR, RR, MAP, GCS and SpO2 estimation [Table/Fig-1] [14]. The higher the REMS score, poor is the prognosis. REMS scoring system has been validated on European patients in modern hospital environment [15]. In few validation studies, REMS at cut-off score of 6 or 7 was found to be better in predicting in-hospital mortality in emergency department patients with area under receiver operating curve being significant for REMS [14-16]. REMS was found to have the same predictive accuracy as APACHE II score [17].
The aim of the study was to evaluate the efficacy of REMS score and validate its utility in patients with sepsis in predicting mortality.
Materials and Methods
This was an observational, cohort study conducted in the Department of Medicine of SCB Medical College and Hospital, Cuttack, during the period of June 2019 to May 2020. Institutional Ethics Committee approved this study vide their letter number IEC/IRB. No. 103/dated 07.02.2020. Informed written consent in local odia language was taken from adult patients participating in the study. In case of minors and those unable to give consent, legal guardian’s consent was obtained. A total of 100 patients admitted to medical wards and ICU of Medicine Department were included in the study. Sample size was calculated to be 82, taking prevalence of sepsis in India to be 28.3% as per INDICAPS study and 10% as margin of error [18]. Simple random sampling was done to select the participants.
Sepsis is diagnosed when a person has at least 2 qSOFA score due to an infection and septic shock is defined as sepsis with MAP less than 65 mmHg after adequate fluid resuscitation or requiring vasopressor to maintain MAP above 65 mmHg [1].
Inclusion criteria: Patients above 15 years of age having signs and symptoms of infection with qSOFA score ≥2 were included in the study.
Exclusion criteria: Patients of acute coronary syndrome, chronic kidney disease, chronic liver disease, immune-compromised state and not willing to participate in the study were excluded.
Detailed history and thorough clinical examination including patient’s age, PR, MAP, GCS, RR were documented and SpO2 (oxygen saturation) was determined by simple fingertip pulse oximeter. qSOFA score and REMS score were calculated at the time of admission by the medicine specialist posted in medical wards or the ICU specialist posted in medicine ICU. All patients were subjected to laboratory investigations like Complete Blood Counts (CBC), blood glucose, renal and liver function tests, serum electrolytes, urine analysis, blood and urine cultures along with thick and thin smears and rapid card test for malaria parasite detection. Patients were categorised into sepsis or septic shock, and were followed-up for 10 days for primary outcome as either death or discharged. The observed data was pooled by the principal investigator and it was then statistically analysed for utility of REMS score in predicting the mortality, which is the secondary outcome of the present study.
Statistical Analysis
Data were checked for normalcy and skewness. The values of normally distributed continuous data were expressed in terms of mean and standard deviation, whereas median and Interquartile Range (IQR) was used for skewed data. The categorical data were expressed as frequency and percentage, and compared using Pearson’s Chi-square test. Student’s t-test and Mann-Whitney U test were used for comparing normally and non-normally distributed data between two groups, respectively. Univariate and multivariate logistic regression was done to calculate the odds ratio, adjusted odds ratio, and 95% confidence interval of the parameters in REMS. Sensitivity, specificity, PPV, NPV, and accuracy of REMS were calculated and the area under ROC curve was obtained. Asymptotic 2-tailed p-value of <0.05 was considered statistically significant. Data were entered using Microsoft excel and analysed using Statistical Package for the Social Sciences (SPSS) software version 18.0 (PASW statistics for Windows, Chicago: SPSS Inc).
Results
Out of 100 patients, 51 were males and 49 were female patients. The mean age of patients participating was 49 years (SD 14.5). Age of the majority of patients was in between 30 to 60 years (70%). Major sources of infection were pneumonia (24%) followed by urinary tract infections (19%) and typhoid (10%) [Table/Fig-2]. In the present study, culture positivity was minimal with three positive blood cultures and 14 positive urine cultures. Gram negative sepsis was the main cause of sepsis in this study.
Primary sources of infection leading to sepsis (N=100).
| Diagnosis | No of cases (N=100) n (%) |
|---|
| Pneumonia | 24 (24) |
| Urinary tract infection | 19 (19) |
| Typhoid | 10 (10) |
| Scrub typhus | 8 (8) |
| Meningitis | 6 (6) |
| Viral hepatitis | 6 (6) |
| Encephalitis | 5 (5) |
| Cellulitis | 4 (4) |
| Splenic abscess | 4 (4) |
| Hepatic abscess | 3 (3) |
| Septic arthritis | 3 (3) |
| Malaria | 3 (3) |
| Dengue | 2 (2) |
| Infective endocarditis | 2 (2) |
| Empyema | 1 (1) |
REMS score was calculated on the day of admission of all 100 patients. REMS score differ significantly among the survivors and non survivors, and clearly distinguishes the survivors from the non survivors (median REMS: 3.5 vs. 9) (p<0.001) [Table/Fig-3]. Logistic regression analysis of these parameters in REMS showed that although all the parameters were significantly associated with mortality prediction in univariate model, only the RR was strongest and independent predictor of mortality in multivariate model [Table/Fig-4].
Descriptive statistics of data comparing survivors and non survivors (N=100).
| Parameters | Survivors (n=76) | Non survivors (n=24) | OR (95% CI) | p-value |
|---|
| Age | 47.1±13.2 | 55.9±16.6 | 1.045 (1.01-1.082) | 0.009 |
| Male | 41 (53.9%) | 10 (41.6%) | 0.610 (0.241-1.543) | 0.294 |
| Female | 35 (46.05%) | 14 (58.3%) | | |
| PR (/min) | 108.8±7.5 | 119.1±7.1 | 1.24 (1.127-1.363) | 0.001 |
| MAP (mmHg) | 84.3±10.6 | 75.8±9.5 | 0.915 (0.866-0.968) | 0.001 |
| RR (/min) | 23.6±2.5 | 28.2±2.4 | 2.907 (1.777-4.753) | 0.001 |
| GCS | 13.9±1.3 | 12.4±1.4 | 0.477 (0.329-0.691) | 0.001 |
| SpO2 (%) | 90.5±2.7 | 86.3±2.4 | 0.461 (0.319-0.665) | 0.001 |
| TLC | 11265±1985 | 12116±2722 | - | 0.099 |
| qSOFA | 4.7±1.9 | 6.8±2.3 | - | 0.001 |
| REMS |
| Mean±Std deviation | 3.65±2.1 | 8.91±1.9 | 2.092 (1.558-2.81) | 0.001 |
| Median (IQR) | 3.5 (2-5) | 9 (7-10) |
For normally distributed continuous data like age, PR, MAP, RR, GCS, SpO2, TLC: Student’s t-test was used to compare the means For not-normally distributed continuous data like REMS score: median values were compared using Mann-Whitney U test. (For REMS score: both mean value as well as median values are mentioned) For categorical parameter like Sex: frequency and percentage was calculated and Chi-square Test was applied; OR: Odd ratio; REMS: Rapid Emergency Medicine Score; PR: Pulse rate; MAP: Mean arterial pressure; RR: Respiratory rate; GCS: Glasgow coma scale; SpO2: Peripheral oxygen saturation; IQR: Interquartile Range; TLC: Total leucocyte count; qSOFA: quick Sequential Organ Failure Assessment
Multivariate logistic regression of REMS parameters to analyse independent predictors of mortality.
| REMS parameters | OR (95% CI) | aOR (95% CI) | p-value |
|---|
| Age | 1.045 (1.01-1.082) | 0.985 (0.895-1.084) | 0.764 |
| PR (/min) | 1.24 (1.127-1.363) | 1.038 (0.855-1.261) | 0.706 |
| MAP (mmHg) | 0.915 (0.866-0.968) | 0.926 (0.825-1.039) | 0.19 |
| RR (/min) | 2.907 (1.777-4.753) | 2.843 (1.185-6.823) | 0.019 |
| GCS | 0.477 (0.329-0.691) | 0.789 (0.369-1.686) | 0.541 |
| SpO2 (%) | 0.461 (0.319-0.665) | 0.627 (0.317-1.237) | 0.178 |
OR: Odd ratio; REMS: Rapid Emergency Medicine Score; PR: Pulse rate; MAP: Mean arterial pressure; RR: Respiratory rate; GCS: Glasgow coma scale; SpO2: Peripheral oxygen saturation
Out of 100 patients, 84 patients had sepsis and death occurred in 15 (17.8%) patients. Among the 16 patients with septic shock, death occurred in nine patients (56.2%). REMS score differed significantly among the patients with sepsis and septic shock (median REMS: 4 vs. 9) (p<0.001) [Table/Fig-5].
REMS among Sepsis and Septic shock (N=100).
| REMS score | Sepsis (n=84) | Septic shock (n=16) | p-value |
|---|
| Mean±Std deviation | 4.14±2.5 | 9±2.3 | <0.001 |
| Median (IQR) | 4 (2-5.75) | 9 (7-10.5) |
REMS: Rapid Emergency Medicine Score; IQR: Interquartile Range
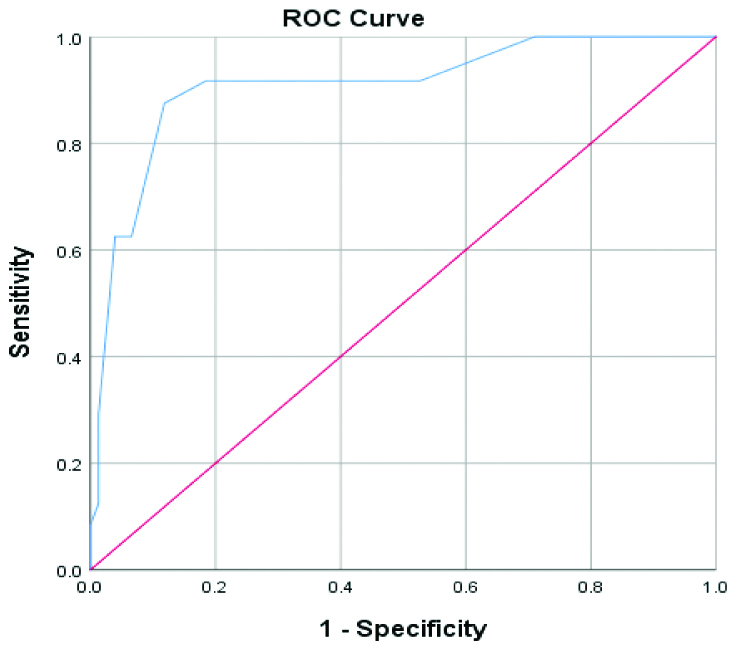
For a cut-off REMS score of 7, REMS had a sensitivity of 87.5%, specificity of 88.2%, PPV of 70%, NPV of 95.7%, and accuracy of REMS was 88%. Area under the ROC curve was 90.8 (95% CI: 83.4-98.2) which validates the use of REMS score in predicting mortality in patients with sepsis and septic shock [Table/Fig-6,7].
Validity of REMS at cut-off score of 7 among survivors and non survivors (N=100).
| REMS score | Non survivors (n=24) | Survivors (n=76) |
|---|
| ≥7 | 21 (87.5%) | 9 (11.8%) |
| <7 | 3 (12.5%) | 67 (88.2%) |
Area under ROC curve for REMS was 90.8 (95% CI: 83.4-98.2); p<0.001.
Discussion
Sepsis can be lethal, if we miss early intervention. Over the past few years, the definition of sepsis and septic shock has been changing. The current guidelines recommends organ dysfunction in sepsis is manifested as acute rise in 2 points of qSOFA score from baseline which takes SBP, RR, and altered mentation into account [1]. Mortality due to sepsis is as high as 21% in Indian scenarios [18]. In the present study, it was found that the mean age of patients was 49 years with increasing age associated with higher mortality. Males and females were almost equally distributed and gender was not significantly associated with mortality which is in accordance with the study conducted by Ghanem-Zoubi NO et al., [19]. Respiratory infection is the predominant source of infection (24%) followed by urinary tract infection (19%) [Table/Fig-2]. Culture positivity in the present study was minimal with three positive blood cultures and 14 positive urine cultures. Gram negative sepsis was the main cause of sepsis in this study and similar result was found by Sands KE et al., [20]. Few patients of malaria and viral hepatitis developed sepsis in ICU secondary to bacterial infection acquired through catheter related blood infection or thrombophlebitis. Mortality in patients with septic shock was three times higher compared to the patients with sepsis (56.2% vs. 17.8%), where mortality is closely related to severity of sepsis and number of organs involved according to Martin GS et al., [21].
Logistic regression analysis of these parameters in REMS showed that although all the parameters were significantly associated with mortality prediction in univariate model, only the RR was strongest and independent predictor of mortality in multivariate model [Table/Fig-4]. In a similar way, there is consistency in mortality prediction of all the parameters in univariate analysis, but the independent predictors of mortality vary across multiple studies [15,17,22].
REMS score was significantly high among the non survivors as compared to the survivors {median REMS: 9 (7-10) vs. 3.5 (2-5)} [Table/Fig-3]. Patients with septic shock had higher REMS score compared to the patients with sepsis {median REMS: 9 (7-10.5) vs. 4 (2-5.75)} which was also statistically significant [Table/Fig-5]. Thus, higher the REMS score of a patient, it is more likely that the patient would not survive even with the standard protocol of management. In resource limited country, this scoring system can be used to further prioritise the available resources for better outcome [8-10].
The area under the Receiver Operating Characteristic (ROC) curve was 90.8 (95% CI: 83.4-98.2) [Table/Fig-7]. This is in accordance with study conducted by SEAK CJ et al., [23]. The REMS score predicting 1-day and 10-day mortality in sepsis patients are comparable to that of the present study [19]. The sensitivity of REMS score was analysed using the ROC curve and it showed a sensitivity of 87.5% and accuracy of REMS as 88% in predicting the mortality at a cut-off score of 7. REMS cut-off score of 6 or 7 predicted mortality most accurately in emergency department [14,24,25]. REMS score is a valid scoring test to predict mortality in patients with sepsis, which is in accordance with the study conducted by SEAK CJ et al., [23]. The advantage of using REMS to predict outcome is that it is an efficient, convenient, and time-saving assessment tool that can be performed in poor infrastructural emergency departments and ICUs. REMS scoring system provides a good clinical utility to the overstretched emergency physicians to sieve, prioritise patients with sepsis, and optimise the available resources for a better outcome [26]. Adequate sample size, systematical approach towards diagnosis and data collection, and robust statistical tests used to validate the REMS scoring system were the strengths of the current study. Further studies with larger sample size are required to evaluate the reliability of REMS scoring system and analyse the independent predictors of mortality in resource poor settings, are the future recommendations of the present study.
Limitation(s)
The present study used only the REMS scoring system to predict the mortality and the future studies should include the other available scores like APACHE II, SOFA or MPM in comparison with REMS.
Conclusion(s)
REMS score calculated on the day of admission can significantly discriminate between the survivors from the non survivors. The REMS score of non survivors was significantly higher compared to the survivors. High sensitivity, specificity, and accuracy of REMS are particularly helpful in resource limited emergency departments in predicting mortality in patients with sepsis and septic shock.
PR: Pulse rate; MAP: Mean arterial pressure; RR: Respiratory rate; GCS: Glasgow coma scale; SpO2: Peripheral oxygen saturation
For normally distributed continuous data like age, PR, MAP, RR, GCS, SpO2, TLC: Student’s t-test was used to compare the means For not-normally distributed continuous data like REMS score: median values were compared using Mann-Whitney U test. (For REMS score: both mean value as well as median values are mentioned) For categorical parameter like Sex: frequency and percentage was calculated and Chi-square Test was applied; OR: Odd ratio; REMS: Rapid Emergency Medicine Score; PR: Pulse rate; MAP: Mean arterial pressure; RR: Respiratory rate; GCS: Glasgow coma scale; SpO2: Peripheral oxygen saturation; IQR: Interquartile Range; TLC: Total leucocyte count; qSOFA: quick Sequential Organ Failure Assessment
OR: Odd ratio; REMS: Rapid Emergency Medicine Score; PR: Pulse rate; MAP: Mean arterial pressure; RR: Respiratory rate; GCS: Glasgow coma scale; SpO2: Peripheral oxygen saturation
REMS: Rapid Emergency Medicine Score; IQR: Interquartile Range