ABR has emerged as a serious threat to the quality of public health care. It develops when bacteria become resistant to the antibiotics used to treat infections caused by them. Patients infected with resistant bacteria like Methicillin Resistant Staphylococcus aureus (MRSA), Vancomycin Resistant Enterococci (VRE), and Extended Spectrum Beta Lactamase (ESBL) producers take longer to treat, require more frequent doctor visits, and are likely to face prolonged hospital stays, more severe side effects, expensive treatments and increased mortality [1].
Emergence of ABR over time is a naturally occurring process, but this has been accelerated to dangerously high levels due to misuse and over-use of antibiotics in plants, animals and humans worldwide. Infections such as pneumonia, tuberculosis, gonorrhoea, malaria, and foodborne diseases have now become harder and sometimes impossible to treat. This combined with almost negligible development and availability of novel drugs has precipitated a global crisis [1-4].
It is noteworthy that though ABR is a global challenge affecting people of all ages, but nowhere is it as stark as in India [5]. Factors such as high prevalence of infection, poor infection prevention and control guidelines, lack of clinical microbiology laboratories, irrational use of antimicrobials, and easy availability of antibiotics over-the-counter have put Indian healthcare system in a very precarious position [6]. Most of hospitals lack standard treatment guidelines and knowledge on AMS is minimal. Consequently, India has a very high incidence of ABR and HAI rates. Lack of prompt and substantial action is likely to lead us to a post-antibiotic era, in which common infections and minor injuries would prove lethal [7].
It is incumbent to start implementing strategies for an effective control of further development and spread of ABR. Coordinated action from all the stakeholders in society is required wherein the frontline fighters have to be the healthcare professionals, especially future physicians. They carry the dual responsibility of rationally prescribing antibiotics and sensitising the general population [8]. It has been observed that although physicians are aware of ABR and its contributing factors, this awareness does not necessarily influence their prescribing practices. Also, there is sufficient evidence to support that newly licensed doctors are not adequately trained to prescribe medications safely [9-11]. A healthy understanding of AMS and good prescribing practices is crucial. Continuous education and training is a potent tool to achieve these targets. This training should start early, preferably during medical college, continue during undergraduate clinical training, and be reinforced throughout postgraduate training. Educational modules incorporated early in the medical curriculum may help increase the awareness of medical students on such issues.
Materials and Methods
Study Design and Study Population
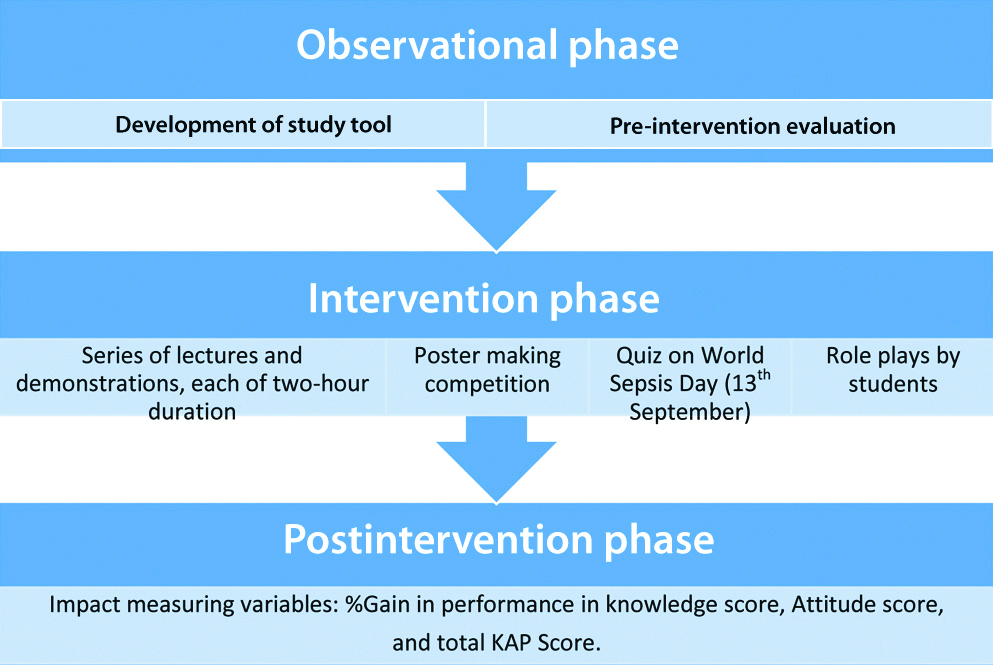
This pre-post-quasi experimental non-randomised study with prospective design “HAI and ABR Awareness Campaign” organised by Departments of Microbiology and Pharmacology of a University Medical College, Jaipur, Rajasthan, India was done from 08th to 14th September 2018. The study design is depicted in flowchart [Table/Fig-1]. Out of a batch of 100, 5th semester MBBS undergraduate students, 86 students consented and were included in the study.
Study Instrument
The instrument used was a preformed pretested 30 item self-administered questionnaire which was developed after literature review comprising questions related to demographics (seven questions), knowledge (twelve questions), attitudes (seven questions), and practices (four questions) associated with ABR and HAI. The questionnaire was validated by doing pre-test on 5% of the sample before the actual data collection period. Necessary modification of the questionnaire was carried out based on the pre-test feedback. Socio-demographic data included gender, father’s occupation, mother’s occupation and residential address of the participant. Participant’s knowledge assessment was in domains related to HAI (definition and types, common pathogens involved, mode of transmission, methods for prevention) and ABR (factors contributing to the development, spread and containment of ABR). The beliefs of the participants were assessed by questions addressing their attitude towards the importance of appropriate prescription, dispensing, and consumption of antibiotics. The practices towards prevention of transmission of HAI and correct use of antibiotics were also assessed.
Pre-intervention
The study participants were approached through personal communication. They were asked to fill the study questionnaire which was then collected by the investigator. Subsequently, the same participants were delivered a series of lectures and demonstrations on HAI, hand hygiene and ABR, over a week long study period i.e., 08th to 14th September 2018. They also participated in poster making competition where they made creative posters on either of the above mentioned topics. The participants were then asked to give a brief presentation on their poster to a panel of judges who were distinguished clinicians, microbiologists or administrators from various multispecialty hospitals of the city. Finally, on World Sepsis Day i.e., 13th September, a quiz was organised which was attended by all the study participants, either as audience or as quiz participants. There were role plays done by students.
Post-intervention
After the interactive sessions and activities, the study participants were asked to fill the same questionnaire again. The performance of individual participant before and after the interactive sessions and activities was then statistically analysed.
Ethical committee approval: Since the study had less than minimal risk and there were no linked identifiers, it was exempted from Ethical Committee Review.
Statistical Analysis
The data were collected, compiled, coded and analysed with Microsoft Excel and Software SPSS version 20. The demographic variables were compiled as count and percentages. Each correct response was given one score and each wrong response got zero score. Each student’s questionnaire was scored in this manner. The frequencies and percentages of participants with correct response before and after intervention were analysed in all three domains of KAP per item question wise and statistically supported with Chi-square test. The median scores were also calculated for each question as well as each domain. Box and Whiskar plot of impact variables was prepared. The statistical significance was set at 5%. The overall impact of intervention was expressed as improvement in median scores and percent increase in participants with correct response in all three domains separately and then summated to calculate overall impact subsequently. The impact was also categorised as poor, average and excellent according to the scores as 0-50%, 50-75%, and ≥75%.
Results
Characteristics of Study Participants
A total of 86, 5th semester MBBS undergraduates participated in the study. Responses of all these students were noted for questions on HAI and ABR. The number of responses for each question varied slightly as not all students responded to all questions. The demographics of the students has depicted in [Table/Fig-2].
Demographic characteristics of study participants (n=86).
| Category | Frequency | Percentage |
|---|
| Gender | Female | 33 | 38.4% |
| Male | 53 | 61.6% |
| Father’s occupation | Medical profession | 15 | 17.4% |
| Non-medical profession | 71 | 82.6% |
| Mother’s occupation | Medical profession | 10 | 11.7% |
| Non-medical profession | 15 | 17.4% |
| Housewife | 61 | 70.9% |
| Residence | Rural | 23 | 26.7% |
| Urban | 63 | 73.3% |
Knowledge
All the students agreed that ABR is an important and serious public health issue worldwide. Before intervention, 52.3% students were aware of resistant organisms like MRSA, VRE, and ESBL producers as compared to 97.7% students post intervention. Pre and post-intervention, 5.8% and 89.5% students, respectively correctly defined and identified various components of AMS i.e., namely choice of antibiotics, dosage, frequency and duration, time of administration, adverse effect, and route of administration. A 44.2% students pre intervention and 86% post-intervention could correctly tell the functions of Hospital Infection Control Committee (HICC) i.e., to regularly review the infection control activities of the hospital, monitor emergence of drug resistance, formulate antibiotics policy, recommend suitable sterilisation and disinfection procedures, maintain data on the incidence and type of infections and antibiotics susceptibility patterns of the common prevalent pathogens. The pre and post-intervention response of the students to questions related to Knowledge on HAI and ABR has depicted in [Table/Fig-3].
Knowledge of study participants on Hospital Acquired Infection (HAI) and Antibiotic Resistance (ABR). [HICC=Hospital Infection Control Committee]
| S. No. | Parameter | Pre-intervention correct response N (%) | Post-intervention correct response N (%) | p-value (Chi-square test) |
|---|
| 1. | Definition of HAI | 47 (54.7) | 82 (95.3) | <0.0001 |
| 2. | Gram negative organisms are the most common pathogen responsible for nosocomial pneumonia in ICU | 16 (18.6) | 86 (100) | <0.0001 |
| 3. | Direct contact is the most common mode of transmission of HAI | 10 (11.6) | 71 (82.6) | <0.0001 |
| 4. | Personal Protective Equipment (PPE) | 43 (50) | 77 (89.5) | <0.0001 |
| 5. | Principles of AMS | 5 (5.8) | 77 (89.5) | <0.0001 |
| 6. | Outbreak investigation when required. | 66 (76.7) | 54 (62.8) | 0.05 |
| 7. | Composition of HICC | 38 (44.2%) | 74 (86.0%) | <0.001 |
HAI was correctly defined by 54.7% before intervention as against 95.3% post intervention. This difference was found to be statistically significant (p<0.0001) [Table/Fig-3]. Similarly, other questions related to common pathogens responsible for nosocomial pneumonia in ICU (18.6% vs 100% students); common modes of transmission (11.6% vs 82.6%); knowledge on PPE (50% vs 89.5%); and composition of HICC (44.2% vs 86.0%) showed a statistically significant improvement [Table/Fig-3]. However, when asked about the right time for doing outbreak investigation, 76.7% student pre-intervention could answer it correctly while this percent decreased to 62.8% postintervention. This decline was statistically significant and no valid reasons were found for the same. It however indicates that in future such academic events need to stress more on outbreak management.
Attitude
The attitude of the students was assessed by asking them True and False questions related to HAI and ABR. When asked about the factors they think may help prevent or contain ABR; pre-intervention 1.2%, 3.5%, and 2.3% thought that treating infection and not contamination or colonisation, ongoing education program on appropriate antibiotic therapy, and hospital antibiotic policy or stewardship, respectively alone may help while 83.7% thought that all three factors together with development of better diagnostic tests will help. Post-intervention, 94.2% responded that all the above mentioned factors are helpful. The pre and post-intervention responses of study participants is shown in [Table/Fig-4].
Attitude of respondents towards antimicrobial resistance.
| S. No. | True-False questions | Correct answer | Respondents who answered correctly N (%) | p-value (Chi-square test) |
|---|
| Pre-test | Post-test |
|---|
| 1. | Indiscriminate and injudicious use of antibiotics lead to antibiotic resistance | Yes | 80 (93) | 86 (100) | 0.0128 |
| 2. | Patients in your hospital are at risk of infection with resistant bacteria like MRSA, VRE, and ESBL | Yes | 58 (67.4) | 72 (83.7) | 0.013 |
| 3. | Antibiotics speed up the recovery of common cold/ viral sore throat | No | 53 (61.6) | 71 (82.6) | 0.0022 |
| 4. | Culture/sensitivity report should guide antibiotic prescription pattern | Yes | 74 (86) | 82 (95.3) | 0.0367 |
| 5. | Antibiotics should not be dispensed without a valid prescription of a doctor | Yes | 77 (89.5) | 86 (100) | 0.0021 |
| 6. | Skipping one or two dose of antibiotics does not contribute to the development of antibiotic resistance | No | 46 (53.5) | 64 (74.4) | 0.0044 |
Practice
[Table/Fig-5] depicted the practices being followed by the students towards the containment of ABR, pre and post-intervention. During the campaign, practices that help contain spread of HAI and ABR were emphasised. The impact was then assessed by comparing their pre and post-intervention practices score. Results showed that pre and post-intervention, the respective percentage of students who followed five moments of hand hygiene was 93% and 100% (p-value-0.0128) and wearing PPE in the correct sequence was 31.4% and 95.3% (p-value-<0.0001).
Practice towards containing antimicrobial resistance.
| S. No. | Practice parameters | Pre-intervention | Post intervention | p-value (Chi-square test) |
|---|
| 1. | Follow five moments of hand hygiene | 80 (93.0) | 86 (100) | 0.0128 |
| 2. | Do not prefer to take an antibiotic in common cold/sore throat | 45 (52.3) | 74 (86) | <0.0001 |
| 3. | Complete full course of antibiotic treatment | 72 (83.7) | 78 (90.7) | 0.1707 |
| 4. | Use of PPE | 27 (31.4) | 82 (95.3) | <0.0001 |
Overall Impact of Intervention
The pre-intervention combined KAP score was found to be poor in 17.4% study participants, average in 61.6%, and excellent in 20.9% study participants. Post-intervention combined KAP score was found to be poor, average, and excellent in 1.1%, 8.14%, and 90.7% study participants, respectively. A statistically significant decrease in the percentage of students with poor score and a significant increase in those with excellent scores was observed after the intervention (p<0.05).
Association with Parents Occupation
Authors then studied the impact of the parents’ profession on the KAP of students towards ABR and HAI. The students were grouped into those where either of the parent was a medical professional and those whose parents were not medical professionals. Results have been compiled in [Table/Fig-6]. It was observed that overall KAP scores were significantly better in group of students where either or both parents were medical professionals.
Association of scores obtained by students with either parent’s occupation (N=86).
| Parents medico (N=15) | Parents non medico (N=71) | p-value (independent t-test) |
|---|
| Knowledge score pre-intervention (mean±SD) | 9.13±1.302 | 8.01±1.824 | 0.027 |
| Knowledge score post-intervention (mean±SD) | 7.47±1.125 | 8.01±1.824 | 0.268 |
| Attitude score pre-intervention (mean±SD) | 6.13±0.834 | 4.77±1.466 | <0.001 |
| Attitude score post intervention (mean±SD) | 6.87±0.516 | 6.03±1.095 | <0.001 |
| Practice score pre-intervention (mean±SD) | 2.87±0.834 | 2.55±0.923 | 0.222 |
| Practice score post intervention (mean±SD) | 3.80±0.561 | 3.70±0.571 | 0.555 |
| Total score pre intervention (mean±SD) | 17.00±1.604 | 14.14±3.226 | <0.001 |
| Total score post intervention (mean±SD) | 21.87±1.060 | 20.49±2.413 | 0.001 |
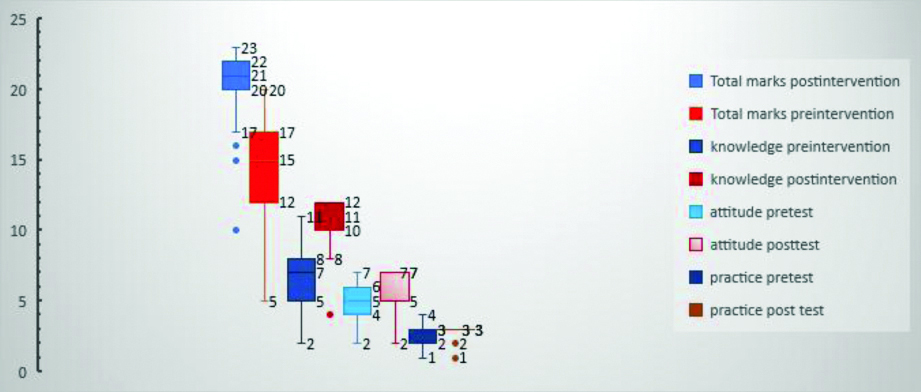
[Table/Fig-7] showed Box and Whisker plot demonstrating increase in post-intervention KAP score.
Box and Whiskar plot of impact variables.
Discussion
Growing ABR is a new world pandemic. Alongside, HAIs are causing alarming rates of morbidity and mortality [1-4]. Healthcare professionals, beyond doubt are the frontline fighters against these twin evils. They urgently need to change the way they prescribe antibiotics, failing which the world will remain in threat, even if new drugs are developed. Also, AMS practices need to be understood and implemented aggressively.
One of the most effective tools to ensure this is continuous education and training of healthcare professionals on appropriate antibiotic use and infection control practices. Medical undergraduates hold a key position in healthcare machinery. If their young minds are sensitised and trained adequately, they can bring about far reaching and sustaining results. Short and repeated educational programs incorporated early in the medical curriculum would help increase the awareness of medical students.
In the present study, the baseline awareness of students on HAI and ABR was first identified and graded by evaluating their self-filled questionnaire. In the initial survey, all the 86 students correctly identified that ABR is an important and serious public health issue. This response was much better as compared to the reports of other studies [12,13]. Further, 93% of the students in the present study believed that indiscriminate and injudicious use of antibiotics led to ABR. Similar findings have also been reported by studies done by Yashin AN et al., Manali M et al., Tarao MS et al., and Akram A et al., [14-17]. However, the study conducted by Khan A et al., reported that only 85% of total respondents believed that cause of bacterial resistance was due to its indiscriminate use [8]. A buoyant response observed in this study group may be the result of ongoing national and international efforts to raise awareness on ABR.
Previous studies done by Yashin AN et al., and Zafar SN et al., showed that 70% and 60% of participants, respectively believed that antibiotics should be prescribed for viral diseases like sore throat and cough [14,18]. A low level of awareness among students in this regard has also been reported by several other studies [8,13,19,20]. Interestingly and contrary to the above observations, 61.6% respondents in the present study believed that antibiotics do not speed up the recovery of common cold. This indirectly showcased their knowledge on the fact that diseases like influenza and common cold are not of bacterial origin and hence do not need antimicrobial drugs. Comparable findings have also been observed by Ahmad A et al., among undergraduate Pharmacy students of Trinidad and Tobago and Jorak A et al., among medical students in Iran [17,21]. However, much to our dismay, this positive attitude observed in the study participants was not similarly reflected in their practices as only 52% of them admitted that they do not prefer to take an antibiotic in common cold/ sore throat. In spite of having the right attitude these participants continue to observe the wrong practices. Variable practices in this regard have been reported by many other studies [8,22,23].
Another encouraging result observed in this study was that around 83.7% respondents admitted that they complete their full course of antibiotic treatment. Yashin AN et al., reported 92% of respondents completing the full course [14]. Mixed findings have been reported by many other authors in this regard [8,13,17,20,24]. A 89.5% of the study population believed that antibiotics should not be dispensed without a valid prescription of a doctor. Similar kind of result was also found in a study by Tarao MS et al., [16].
In the present study, the baseline KAP score was average in 61.6% and excellent in 20.9% students. These scores are lesser than a similar study done by Dutt HK et al., wherein the KAP grading came out to be moderate in 74.4% respondents who were final year students of medical, dental, and nursing courses [25]. The fact that only 5th semester MBBS undergraduates were included may explain this disagreement as these students have lesser clinical exposure in terms of patient dealing as compared to final year students. Some of the recent studies in other developing countries have showed an inadequate knowledge regarding antibiotic use and resistance, in addition to a lack of formal training about antibiotics during the undergraduate teaching [26].
Although the baseline awareness of the students in the present study was satisfactory but there existed a significant gap in their KAP which was evident from the percent of students giving correct responses [Table/Fig-3,4 and 5] to the related questions.
Interestingly, only 5.8% students recognised that the maximum consumption of antibiotics occur for non-therapeutic use in animals. This response was very poor as compared to a study which states that 54.6% of medical undergraduates know that excessive antibiotic use occurs in livestock [26]. It is noteworthy that excessive use of antibiotics in animal feedstock contributes to development of ABR [27].
The KAP grade of 17.4% students was poor before intervention which then decreased to 1.1% post-intervention. Percentage of excellent performers increased from 20.9% before intervention to 90.7% post-intervention. These differences were found to be statistically significant.
During analysis, it was speculated that better scores would be found among students who’s either of the parents was a medical professional and the overall KAP scores of study participants showed expected results. The group with doctor parents had significantly better scores both pre and post-intervention. Baseline knowledge and attitude scores were also significantly better in expected group. However, no significant difference in items pertaining to practice domain was seen in both groups pre and post-intervention. These results were very encouraging as they indicate a positive effect when the family culture has been continuously incorporating these in their discussions and habits [Table/Fig-6].
Since, the medical students are going to be future prescribers, it is important to have proper guidelines in medical curriculum related to rational use of antibiotics. An in-depth understanding of various HAIs and infection control measures need to be imparted. Education is the major and most important intervention by which students can be aware of the important concept of antimicrobial resistance. The current study signifies the amount of change that can be brought about by implementing simple educational modules and can be used as a guide by policy makers while defining medical curriculum for future generation of doctors.
Limitation(s)
Though this study concentrates on a potential target population that can play an important role in the prevention of antimicrobial resistance, small sample size was a limitation. Another limitation was related to the design of the questionnaire. Even if the questions regarding knowledge and attitude allow the respondents to state their true thoughts without any suggestion, there is a possibility that respondents gave socially acceptable answers.
Conclusion(s)
The study indicated that MBBS students were aware of Antibiotic Resistance and believes it is an extremely important global challenge. The current study also reiterates that there were few gaps in understanding and that these gaps can be cemented with the use of suitable educational programs. There is an urgent need for suitable amendments in current MBBS curriculum to include modules which comprehensively address the core principles of HAI, ABR, and AMS.