Introduction
Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) disease also known as COVID-19 was first reported in China in December, 2019 [1]. There were several cases of pneumonia noticed among the residents of Wuhan, China which later on spread to other countries and in March 11 2020, World Health Organisation (WHO) declared this novel coronavirus as a pandemic. COVID-19 has affected millions worldwide and has led to death of thousands. As on 18th July, 2020 about 14, 106, 753 confirmed cases with mortality of 602, 656 globally were recorded [2]. The novel coronavirus is an infectious disease affecting the respiratory system presenting as cough, fever, breathlessness and in severe cases as pneumonia. Other symptoms include anosmia and dysgeusia, headaches, abdominal pain, fatigue, haemoptysis, diarrhoea and chest pain [3,4]. Transmission of this virus is from human to human via droplets from coughing or sneezing.
It is obvious that COVID-19 infection affects other systems outside the respiratory system. The haematological and coagulation systems are commonly affected. The D-dimer level is often elevated and abnormalities of the coagulation system manifesting as Disseminated Intravascular Coagulopathy (DIC) or VTE are often diagnosed. COVID-19 has also been well described as causing a proinflammatory and hypercoagulable state with marked elevations in Lactate Dehydrogenase, Ferritin, C-reactive protein, D-Dimer, and Interleukin levels IL-2R, IL-6, IL-10, and Tumour Necrosis Factor alpha (TNF-α) [5,6]. With this knowledge, one is left to ask how these haematological markers could help clinicians to predict the severity and prognosis of patients who are newly diagnosed with COVID-19. An in-depth review of the haematological markers of COVID-19 severity is presented in this paper.
Epidemiology and Spread
All races are affected. The natural reservoirs of COVID-19 are the bats as seen in other epidemics of coronaviruses- SARS CoV-1 and Middle East Respiratory Syndrome (MERS). The SARS CoV-2 may have undergone mutation in order to infect man. Investigations are currently on-going to find other animal sources of corona virus. The spread of this virus is from human to human and many infected individuals have died from complications of the infection [7-9]. Those patients with severe forms of COVID-19 are known to shed the virus more than the asymptomatic or mild cases [10]. The predominant mode of transmission of the virus is via respiratory droplet, contact with a sufferer or an asymptomatic carrier.
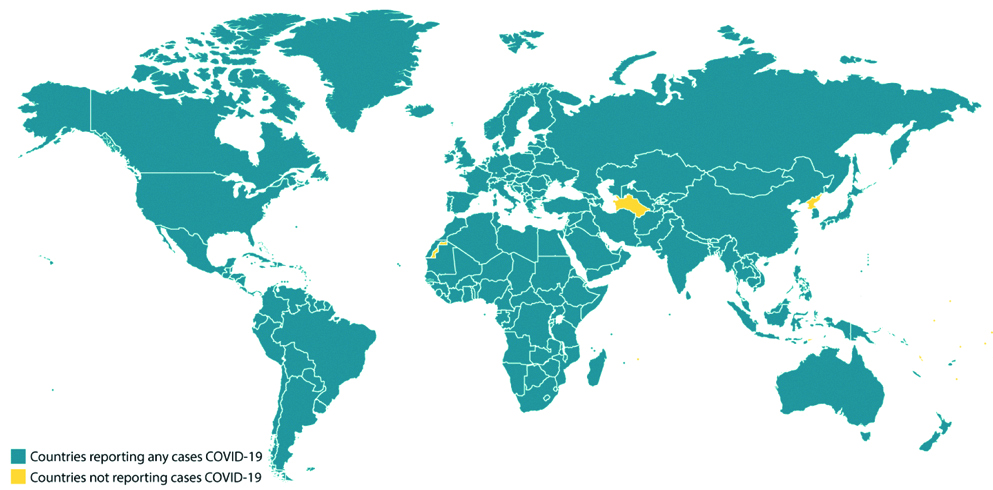
COVID-19 has an incubation period of 1 to 14 days [11]. A mean incubation period of 5.1 days was also reported by Lauer SA et al., and that 97.5% of patients developed symptoms within 11.5 days of acquiring COVID-19 infection [12]. The clinical presentation of this infectious disease has a wide spectrum: asymptomatic, mild, severe (hypoxia, dyspnea, >50% lung involvement) and critical cases (multi-organ failure, shock, respiratory failure) and death from COVID-19 infection [13]. The older populations and individuals with other co-morbidities; cancer, diabetes, asthma and cardiovascular diseases are known to succumb faster to the disease [9,14-17]. The global distribution of COVID-19 is shown in [Table/Fig-1] [18].
Global distribution of COVID 19 cases as of 10:30 am ET 28th May, 2020 [18].
International locations with confirmed COVID. Center for disease control. Available at https://www.cdc.gov/coronavirus/2019-ncov/global-covid-19/world-map.html. Accessed on 28th May, 2020
Complete Blood Count and Its Relevance
As part of the initial investigations that will help in case management, COVID-19 patients are requested to do Full Blood Count (FBC). The components of FBC include: haemoglobin level, total white cell count and differentials (neutrophil, lymphocyte, basophil, eosinophil) and platelet count. On admission most patients were found to have normal haemoglobin level, white cell count and platelet count. These findings were commonly seen in early clinical stage or mild cases of the infection [19]. In another study by Huang C et al., it was noted that 25% of patients on admission had leukopenia with a total white cell count of less than 4×109/L while 63% had lymphocytopenia (<1.0X 109/L) [20]. The disparity seen on the FBC depends on the clinical stage of the patient at the time of admission. The haematological parameters often become deranged with progressive disease. Marked cytopenias are more commonly seen in severe forms than in milder forms of the infection [21,22]. Therefore, FBC plays a key role as an independent predictor of severity of the COVID-19 symptoms.
White Cell Count
A reduced lymphocyte count has been noted by several scholars [23,24]. Early in the disease, the FBC is usually normal but a peripheral blood film shows a reduced lymphocyte count which progressively decreases as the severity of the COVID-19 infection worsens [19,25]. Data from several studies across different geographical regions from China to Singapore to Washington DC were reviewed and showed that lymphocytopenia is a marker of severity for COVID-19 infection [19,26-28]. The proposed reason for the lymphocytopenia has been attributed to factors such as: 1) increased IL production (IL-6, IL-2, TNF alpha) which promotes apoptosis of the lymphocytes; 2) direct infection and destruction of the lymphocyte by the virus through the Angiotensin Converting Enzyme (ACE) receptors; and 3) atrophy of the spleen and other lymphoid organs which occur with the cytokine storm leading to reduced lymphocyte mobilisation [29-33]. It was found that COVID-19 survivors had their lowest lymphocyte count on the 7th day of the illness, and that lymphocyte count improves as patient recovers from the infection [30].
Platelet Count
Platelets are blood cells that are involved in coagulation, haemostasis, maintenance of the integrity of the blood vessels, and in inflammatory responses. Yang M et al., in 2005 noted a consistent feature of thrombocytopenia in critically ill patients with severe acute respiratory syndrome [34]. Patients with COVID-19 infection are known to have a low platelet count which worsens as the disease progresses. Thus, lower the platelet count, the worse the severity or the prognosis of the infection. Yang X et al., in 2020, found that 20.7% of patients had thrombocytopenia [35,36]. The underlying mechanism of thrombocytopenia as proposed by Xu P et al., included inhibition of platelet synthesis by direct infection of the progenitor cell by the virus and increased platelet consumption from the cytokine storm [37]. Qu R et al., however, demonstrated that a better marker for prognosis would be a Platelet Lymphocyte Ratio (PLR). The reason is that since both parameters are involved in immunity, a more sensitive measure would be the use of PLR which depicts the extent of systemic inflammation. He also noted that a high PLR was seen among COVID-19 patients who stayed sick for a longer period of time. The platelet peak occurs as a result of platelet activation by the cytokine storm [38]. FBC could therefore help to quickly determine the clinical severity of COVID-19 infection. This will aid in prompt intervention and may save many lives.
Coagulation and Thrombosis
Critically ill patients admitted into critical care wards are known to develop coagulation disorders including Pulmonary Embolism (PE) and Deep Vein Thrombosis (DVT). PE and DVT make up VTE. Several factors such as hypertention, obesity, inherited thrombophilias (Factor V Leiden), immobilisation, critical illness, surgery and malignancies are all predisposing factors to VTE [39]. Patients with COVID-19 who are critically ill also have these risk factors and have been found to have abnormal coagulation results. According to Klok FA et al., COVID-19 patients especially those admitted into the Intensive Care Unit (ICU) are predisposed to arterial (myocardial infarction, ischemic stroke) and venous thrombosis. The reasons stem from hypoxia, chronic inflammation and immobility of these patients [40]. Furthermore, the organ dysfunction observed in several COVID-19 patients such as liver dysfunction and renal dysfunctions are common factors which can increase their bleeding risk or thrombotic risk [41].
It has been demonstrated by several studies that critically ill COVID-19 patients especially those with Acute Respiratory Distress Syndrome (ARDS) have abnormal coagulation parameters. Those who died from COVID-19 complications were found to have had DIC with prolongation of the PT/International Normalized Ratio (INR) and APTT. This could be explained by the fact that infections and inflammatory processes are notable mechanisms that could activate and accelerate the coagulation system. Excessive consumption of coagulation factors during sepsis leads to DIC in COVID-19 patients with severe clinical illness. Therefore, it is necessary to carry out routine screening for any derangements in coagulation functions in all newly diagnosed COVID-19 patients [42]. The D-dimer test is a negative predictor of thrombosis and when the levels are markedly elevated, thrombosis should be suspected and treatment commenced. There has been an increased D-dimer level above the upper limit of normal which is also seen in non-COVID-19 patients who are critically ill [43]. It has also been used as a way to assess the severity of the disease and its mortality too [44]. PE has been reported as the most frequent complication among ICU patients with COVID-19 [40]. Ranucci M et al., noticed a normalised coagulation profile when they commenced anticoagulation regimen with Low Molecular Weight Heparin (LMWH) and suggested that all COVID-19 patients be started on therapeutic anticoagulation [43]. It was noted that COVID-19 patients with elevated levels of D-dimers at high risk of VTE are far clinically better when commenced on heparin [40,45].
Blood Transfusion and COVID-19
As the coronavirus pandemic rages worldwide, social distancing and self-quarantine are measures put in practice to control the spread of the virus. These same measures also keep the donors away from the blood centers thus reducing the number of blood donors at various blood donation centers. Similar trend was also seen during the H1N1 pandemic where donors feared contracting the virus from donation facilities and hence stayed at home [46,47]. Many blood centers may be faced with the problem of blood shortages due to reduction in donation rate. The possibility of transmission of coronavirus via blood transfusion has been put forward but evidence to prove transmission is lacking currently [48-50]. Thus, the uncertainty of COVID-19 transmission though blood transfusion has necessitated a 28 day deferral for donors with history of travel to affected areas or donors that had contact with a COVID-19 patient [50].
The SARS-CoV2 virus is known to attach to the epithelium of cells via the human ACE2 receptors. These ACE2 receptors are also found in the lung, kidney, intestine and the heart. Within 2 to 3 days of showing symptoms of COVID-19, a patient may have RNA copies of SARS-CoV-2 detected in the serum or plasma [48]. This suggests there is a theoretical chance of blood donors transmitting the virus to the recipients. Previous outbreaks of SARs and MERS employed the deferral of cases for 28 days after recovery, and contacts, for 14 days. The AABB (formerly known as American Association of Blood Banks) update on 25th February, 2020 has also as a precautionary measure, stated that blood collections centers may adopt these same measures for blood safety since no infection has been reported to have occurred through blood transfusion [51,52]. Therefore, in order to ameliorate or reduce the pressure of blood shortages on the blood centers and safeguard the blood stock, clinicians must learn to apply good patient blood management [53]. Efforts should be made to prevent or treat those conditions that will cause anaemia, use of alternatives to blood transfusion and minimising excessive blood loss during surgeries by optimising the haemoglobin level preoperatively and achieving adequate haemostasis intraoperatively.
COVID-19 and Haematological Cancers
Haematological cancers are varied in their clinical and biological features. Majority of them are seen in the elderly population. These cancers are associated with immune dysregulation or immuneparesis. The treatment modalities too including radiation, immunotherapy, targeted therapy and chemotherapy also contribute to the immunosuppression and cytopenias seen in patients with haematological cancers. Thus, patients with haematological cancers are at increased risk of developing severe COVID-19 related complications. It is not surprising then to see a higher incidence of pneumonia, use of ventilators and increased mortality among patients with active cancers who contracted COVID-19 infection [54]. Although the novel coronavirus has been noted amongst patients with haematological cancers, no parameter has so far been found to be a predictor of cancer patients that will go on to develop COVID-19. It was noted that patients with haematological cancers usually develop severe forms of COVID-19 infection. This finding was attributed to the effect of the underlying cancer and to the therapy those patients are receiving [55]. This is seen because of bone marrow suppression of many anticancer regimens. Most of these anticancer regimens induce low haemoglobin, neutrophil and lymphocyte count thus worsening the disease severity.
Severs forms of COVID-19 infection are also seen among patients who have non-haematological cancers alongside COVID-19 infection [13]. The fatality rate for COVID-19 is 2.3% among the general population [13,56] but it rises to a rate of 5.6% [15] to 28.6% among cancer patients with COVID-19 infection [57,58]. This period of pandemic will create huge problems for cancer patients (both haematological and non-haematological cancers). There will be delays in diagnosis because some of these patients will present with COVID-19- like symptoms necessitating initial testing for the coronavirus and time wasting. There will be post-ponement of chemotherapy, shortage of blood products and increased risk of infection due to lack of isolation wards. This has been reported among acute leukemia patients by Gavillet M et al., [59]. Onder G et al., noted that out of 355 COVID-19 deaths in Italy, 20% of them had active cancer [60]. Patients with haematological cancers and those who received stem cell transplants are really the vulnerable group for COVID-19 infection. The burning decisions to make now include how to protect this most vulnerable group of patients from infection: whether or not to withhold chemotherapy while treating COVID-19; the need for attenuation of doses or withholding bone marrow suppressive drugs to avoid inducing cytopenias and immunosuppression; reducing number of hospital visits by use of telemedicine for their protection. All these will be taken on a case by case basis because we are dealing with patients with different cancers at different ages and with none or many co-morbidities.
Conclusion(s)
There is a strong relationship between the severity of COVID-19 infection and some haematological parameters. The parameters often become deranged with progressive disease. Marked cytopenias are more commonly seen in severe forms than in mild forms of the infection. The degree of lymphocytopenia and thrombocytopenia could predict the progression to pneumonia and subsequent need for ventilator support due to respiratory failure. The PLR is a better marker of disease severity than isolated lymphocytopenia or thrombocytopenia. There is also elevation of D-dimers and abnormalities of PT and aPTT among hospitalised patients, suggesting the need for prophylactic anticoagulation to prevent VTE. Haematological parameters are therefore important indices that could be used to predict the severity of COVID-19 infection.
[1]. Ashour HM, Elkhatib WF, Rahman MM, Elshabrawy HA, Insights into the recent 2019 Novel Coronavirus (SARS-CoV-2) in light of past human coronavirus outbreaksPathogens 2020 9(3):18610.3390/pathogens903018632143502 [Google Scholar] [CrossRef] [PubMed]
[2]. Johns Hopkins University. COVID-19 Dashboard by the center for systems Science and Engineering (CSSE). Available from: https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6. Accessed on May 15, 2020 [Google Scholar]
[3]. Abduljalil JM, Abduljalil BM, Epidemiology, genome, and clinical features of the pandemic SARS-CoV-2: A recent viewNew Microbes New Infect 2020 35:10067210.1016/j.nmni.2020.10067232322400 [Google Scholar] [CrossRef] [PubMed]
[4]. Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX, Wang QZ, Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: A scoping reviewInfect Dis Poverty 2020 9(1):2910.1186/s40249-020-00646-x32183901 [Google Scholar] [CrossRef] [PubMed]
[5]. Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, Clinical and immunological features of severe and moderate coronavirus disease 2019J Clin Invest 2020 130(5):2620-29.10.1172/JCI13724432217835 [Google Scholar] [CrossRef] [PubMed]
[6]. Han H, Yang L, Liu R, Liu F, Wu KL, Li J, Prominent changes in blood coagulation of patients with SARS-CoV-2 infectionClin Chem Lab Med 2020 58(7):1116-20.10.1515/cclm-2020-018832172226 [Google Scholar] [CrossRef] [PubMed]
[7]. Phan LT, Nguyen TV, Luong QC, Nguyen TV, Nguyen HT, Le HQ, Importation and Human-to-Human Transmission of a Novel Coronavirus in VietnamNew England Journal of Medicine 2020 382(9):872-74.10.1056/NEJMc200127231991079 [Google Scholar] [CrossRef] [PubMed]
[8]. Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family clusterLancet 2020 395(10223):514-23.10.1016/S0140-6736(20)30154-9 [Google Scholar] [CrossRef]
[9]. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Clinical characteristics of 138 hospitalised patients with 2019 novel coronavirus-infected pneumonia in Wuhan, ChinaJAMA 2020 323(11):106110.1001/jama.2020.158532031570 [Google Scholar] [CrossRef] [PubMed]
[10]. Hoehl S, Rabenau H, Berger A, Kortenbusch M, Cinatl J, Bojkova D, Evidence of SARS-CoV-2 infection in returning travelers from Wuhan, ChinaN Engl J Med 2020 382(13):1278-80.10.1056/NEJMc200189932069388 [Google Scholar] [CrossRef] [PubMed]
[11]. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumoniaN Engl J Med 2020 382(13):1199-207.10.1056/NEJMoa200131631995857 [Google Scholar] [CrossRef] [PubMed]
[12]. Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, The incubation period of Coronavirus Disease 2019 (COVID-19) from publicly reported confirmed cases: Estimation and applicationAnn Intern Med 2020 172(9):57710.7326/M20-050432150748 [Google Scholar] [CrossRef] [PubMed]
[13]. Wu Z, McGoogan JM, Characteristics of and important lessons from the coronavirus Disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese center for disease control and preventionJAMA 2020 323(13):1239-42.10.1001/jama.2020.264832091533 [Google Scholar] [CrossRef] [PubMed]
[14]. Sanyaolu A, Okorie C, Marinkovic A, Patidar R, Younis K, Desai P, Comorbidity and its impact on patients with COVID-19SN Compr Clin Med 2020 :01-08.10.1007/s42399-020-00363-432838147 [Google Scholar] [CrossRef] [PubMed]
[15]. Liang W, Guan W, Chen R, Wang W, Li J, Xu K, Cancer patients in SARS-CoV-2 infection: A nationwide analysis in ChinaLancet Oncol 2020 21(3):335-37.10.1016/S1470-2045(20)30096-6 [Google Scholar] [CrossRef]
[16]. Chen T, Wu D, Chen H, Chen T, Wu D, Chen H, Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective studyBMJ 2020 368:m109110.1136/bmj.m109132217556 [Google Scholar] [CrossRef] [PubMed]
[17]. Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, Jin HJ, The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak- An update on the statusMil Med Res 2020 7(1):1110.1186/s40779-020-00240-032169119 [Google Scholar] [CrossRef] [PubMed]
[18]. Center for Disease Control and Prevention. International locations with Coronavirus disease 2019 (COVID-19. Available at https://www.cdc.gov/coronavirus/2019-ncov/global-covid-19/world-map.html. Accessed 28th May, 2020 [Google Scholar]
[19]. Fan BE, Chong VCL, Chan SSW, Lim GH, Lim KGE, Tan GB, Hematologic parameters in patients with COVID-19 infectionAm J Hematol 2020 95(6):E131-34.10.1002/ajh.25774 [Google Scholar] [CrossRef]
[20]. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, ChinaLancet 2020 395(10223):497-506.10.1016/S0140-6736(20)30183-5 [Google Scholar] [CrossRef]
[21]. Wang F, Nie J, Wang H, Zhao Q, Xiong Y, Deng L, Characteristics of peripheral lymphocytes subset alteration in COVID-19 pneumoniaJ Infec Dis 2020 221(11):1762-69.10.1093/infdis/jiaa15032227123 [Google Scholar] [CrossRef] [PubMed]
[22]. Ahnach M, Bouanani N, Nejjari S, Bendari M, Doghmi K, El kettani C, The critical role of complete blood count in the management of patients with COVID-19Pan African Medical Journal 2020 35(2):6310.11604/pamj.supp.2020.35.2.2376433623587 [Google Scholar] [CrossRef] [PubMed]
[23]. WHO. “Solidarity” clinical trial for COVID-19 treatments. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov/solidarity-clinical-trial-for-covid-19-treatments. Accessed on May 29, 2020 [Google Scholar]
[24]. Shen C, Wang Z, Zhao F, Yang Y, Li J, Yuan J, Treatment of 5 critically ill patients with COVID-19 with convalescent plasmaJAMA 2020 323(16):1582-89.10.1001/jama.2020.478332219428 [Google Scholar] [CrossRef] [PubMed]
[25]. Han R, Huang L, Jiang H, Dong J, Peng H, Zhang D, Early clinical and CT manifestations of coronavirus Disease 2019 (COVID-19) pneumoniaAJR Am J Roentgenol 2020 :01-06.10.2214/AJR.20.2296132181672 [Google Scholar] [CrossRef] [PubMed]
[26]. Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington StateJAMA 2020 323(16):161210.1001/jama.2020.432632191259 [Google Scholar] [CrossRef] [PubMed]
[27]. Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational studyLancet Respir Med 2020 8(5):475-81.10.1016/S2213-2600(20)30079-5 [Google Scholar] [CrossRef]
[28]. Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, Nalla AK, Covid-19 in critically Ill patients in the seattle region- Case seriesN Engl J Med 2020 382(21):2012-22.10.1056/NEJMoa200450032227758 [Google Scholar] [CrossRef] [PubMed]
[29]. Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, ItalyJAMA 2020 323(16):157410.1001/jama.2020.539432250385 [Google Scholar] [CrossRef] [PubMed]
[30]. Terpos E, Ntanasis-Stathopoulos I, Elalamy I, Kastritis E, Sergentanis TN, Politou M, Hematological findings and complications of COVID-19Am J Hematol 2020 95(7):834-47.10.1002/ajh.2582932282949 [Google Scholar] [CrossRef] [PubMed]
[31]. Singh S, Sharma A, Arora SK, High producer haplotype (CAG) of -863C/A, -308G/A and -238G/A polymorphisms in the promoter region of TNF-α gene associate with enhanced apoptosis of lymphocytes in HIV-1 subtype C infected individuals from North IndiaPLoS ONE 2014 9(5):e9802010.1371/journal.pone.009802024837009 [Google Scholar] [CrossRef] [PubMed]
[32]. Chan JF, Zhang AJ, Yuan S, Poon VKM, Chan CCS, Lee ACY, Simulation of the clinical and pathological manifestations of Coronavirus Disease 2019 (COVID-19) in golden Syrian hamster model: Implications for disease pathogenesis and transmissibilityClin Infect Dis 2020 :ciaa32510.1093/cid/ciaa32532215622 [Google Scholar] [CrossRef] [PubMed]
[33]. Fu L, Wang B, Yuan T, Chen X, Ao Y, Fitzpatrick T, Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysisJ Infect 2020 80(6):656-65.10.1016/j.jinf.2020.03.04132283155 [Google Scholar] [CrossRef] [PubMed]
[34]. Yang M, Ng MH, Li CK, Thrombocytopenia in patients with severe acute respiratory syndrome (review)Hematology 2005 10(2):101-05.10.1080/1024533040002617016019455 [Google Scholar] [CrossRef] [PubMed]
[35]. Yang X, Yang Q, Wang Y, Wu Y, Xu J, Yu Y, Thrombocytopenia and its association with mortality in patients with COVID-19J Thromb Haemost 2020 18(6):1469-72.10.1111/jth.1484832302435 [Google Scholar] [CrossRef] [PubMed]
[36]. Lippi G, Plebani M, Henry BM, Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: A meta-analysisClin Chim Acta 2020 506:145-48.10.1016/j.cca.2020.03.02232178975 [Google Scholar] [CrossRef] [PubMed]
[37]. Xu P, Zhou Q, Xu J, Mechanism of thrombocytopenia in COVID-19 patientsAnn Hematol 2020 15:01-04.10.1007/s00277-020-04019-032296910 [Google Scholar] [CrossRef] [PubMed]
[38]. Qu R, Ling Y, Zhang Y, Wei L, Chen X, Li X, Platelet-to-lymphocyte ratio is associated with prognosis in patients with Corona Virus Disease-19J Med Virol 2020 10.1002/jmv.2576732181903 [Google Scholar] [CrossRef] [PubMed]
[39]. Rosendaal FR, Causes of venous thrombosisThromb J 2016 14(suppl 1):2410.1186/s12959-016-0108-y27766050 [Google Scholar] [CrossRef] [PubMed]
[40]. Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, Incidence of thrombotic complications in critically ill ICU patients with COVID-19Thromb Res 2020 191:145-47.10.1016/j.thromres.2020.04.01332291094 [Google Scholar] [CrossRef] [PubMed]
[41]. Wang T, Chen R, Liu C, Liang W, Guan W, Tang R, Attention should be paid to venous thromboembolism prophylaxis in the management of COVID-19The Lancet Haematology 2020 7(5):e362-63.10.1016/S2352-3026(20)30109-5 [Google Scholar] [CrossRef]
[42]. Iba T, Levy JH, Levi M, Connors JM, Thachil J, Coagulopathy of Coronavirus Disease 2019Crit Care Med 2020 Available from: https://doi.org/10.1097/ccm. 0000000000004458. Accessed May June 30, 202010.1097/CCM.000000000000445832467443 [Google Scholar] [CrossRef] [PubMed]
[43]. Ranucci M, Ballotta A, Di Dedda U, Bayshnikova E, Dei Poli M, Resta M, The procoagulant pattern of patients with COVID-19 acute respiratory distress syndromeJ Thromb Haemost 2020 18(7):1747-51.10.1111/jth.1485432302448 [Google Scholar] [CrossRef] [PubMed]
[44]. Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, Clinical characteristics of coronavirus disease 2019 in ChinaN Engl J Med [Internet] 2020 382(18):1708-20.10.1056/NEJMoa200203232109013 [Google Scholar] [CrossRef] [PubMed]
[45]. Tang N, Bai H, Chen X, Gong J, Li D, Sun Z, Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathyJ Thromb Haemost 2020 18(5):1094-99.10.1111/jth.1481732220112 [Google Scholar] [CrossRef] [PubMed]
[46]. World Health Organization. Maintaining a Safe and Adequate Blood Supply during Pandemic Influenza Guidelines for Blood Transfusion Services. 2011. Available from: https://www.who.int/bloodsafety/publications/WHO_Guidelines_on_Pandemic_Influenza_an d_Blood_Supply.pdf. Accessed on May 5, 2020 [Google Scholar]
[47]. Masser BM, White KM, Hamilton K, McKimmie BM, Beliefs underlying blood donors’ intentions to donate during two phases of an avian influenza outbreakTransfus Apher Sci 2012 46(1):47-52.10.1016/j.transci.2011.11.00122142514 [Google Scholar] [CrossRef] [PubMed]
[48]. Chang L, Yan Y, Wang L, Coronavirus Disease 2019: Coronaviruses and blood safetyTransfus Med Rev 2020 34(2):75-80.10.1016/j.tmrv.2020.02.00332107119 [Google Scholar] [CrossRef] [PubMed]
[49]. Franchini M, Farrugia A, Velati C, Zanetti A, Romanò L, Grazzini G, The impact of the SARS-CoV-2 outbreak on the safety and availability of blood transfusions in ItalyVox Sang 2020 10.1111/vox.1292832240543 [Google Scholar] [CrossRef] [PubMed]
[50]. AABB. Statement on Coronavirus and Blood Donation. 2020. Available from: http://www.aabb.org/advocacy/regulatorygovernment/Pages/Statement-on-Coronavirus-and-Blood-Donation.aspx. Accessed May 9, 2020 [Google Scholar]
[51]. AABB. Update: Impact of 2019 Novel Coronavirus and Blood Safety. 2020. Available from: http://www.aabb.org/advocacy/regulatorygovernment/Documents/Impact-of-2019-Novel-Coronavirus-on-Blood-Donation.pdf. Accessed May 15th, 2020 [Google Scholar]
[52]. World Health Organization. Maintaining a safe and adequate blood supply during the pandemic outbreak of coronavirus disease (COVID-19). Available from: https://www.who.int/publications-detail/maintaining-a-safe-and-adequate-blood-supply-during-the-pandemic-outbreak-of-coronavirus-disease-(covid-19). Accessed on May 16, 2020 [Google Scholar]
[53]. Shander A, Goobie SM, Warner MA, Aapro M, Bisbe E, Perez-Calatayud AA, The essential role of patient blood management in a pandemic: A call for actionAnesth Analg 2020 131(1):74-85.10.1213/ANE.000000000000484432243296 [Google Scholar] [CrossRef] [PubMed]
[54]. Rassy E, Khoury-Abboud RM, Ibrahim N, Kattan C, Assi T, Kattan J, What the oncologist needs to know about COVID-19 infection in cancer patientsFuture Oncol 2020 16(17):1153-56.10.2217/fon-2020-031232323577 [Google Scholar] [CrossRef] [PubMed]
[55]. He W, Chen L, Chen L, Yuan G, Fang Y, Chen W, COVID-19 in persons with haematological cancersLeukemia 2020 34:1637-45.10.1038/s41375-020-0836-732332856 [Google Scholar] [CrossRef] [PubMed]
[56]. Wu JT, Leung K, Leung GM, Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: A modelling studyThe Lancet 2020 395(10225):689-97.10.1016/S0140-6736(20)30260-9 [Google Scholar] [CrossRef]
[57]. World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19).2020. Available from: www.who.int/docs/def ault-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf. Accessed on May 5, 2020 [Google Scholar]
[58]. Zhang L, Zhu F, Xie L, Wang C, Wang J, Chen R, Clinical characteristics of COVID-19-infected cancer patients: A retrospective case study in three hospitals within Wuhan, ChinaAnn Oncol 2020 31(7):894-901.10.1016/j.annonc.2020.03.29632224151 [Google Scholar] [CrossRef] [PubMed]
[59]. Gavillet M, Carr Klappert J, Spertini O, Blum S, Acute leukemia in the time of COVID-19Leuk Res 2020 92:10635310.1016/j.leukres.2020.10635332251934 [Google Scholar] [CrossRef] [PubMed]
[60]. Onder G, Rezza G, Brusaferro S, Case-fatality rate and characteristics of patients dying in relation to COVID-19 in ItalyJAMA 2020 10.1001/jama.2020.468332203977 [Google Scholar] [CrossRef] [PubMed]