Diagnosis, Multi Drug Resistance, Pulmonary Tuberculosis
Introduction
India has the highest TB burden in the world, accounting for one-fifth of global TB cases. Around 280,000 people die every year from TB in India. The country has the world’s second largest MDR-TB burden after China, with an estimated 99,000 new cases each year [1]. The Schedule Tribes (STs) are the weakest section of the Indian population from the economic and educational perspectives. They constitute about 8.6% of Indian population and the state of Madhya Pradesh has their largest population as per 2011 population census [2]. They are an underprivileged group of society having poor access to the good health care delivery systems. The geographical isolation, unique cultural, social practices, lack of formal education and treatment seeking behaviour, poverty, etc., makes them vulnerable to several health problems including TB and co-associated morbidities like TB-AIDS. The estimated prevalence of TB is observed to be high in the tribes (29.9%) as compared to the non tribal population (21.4%) in India [3]. The STs of Madhya Pradesh are particularly vulnerable to the combined threat of TB, MDR-TB and HIV. The ‘Saharia’ tribe in Madhya Pradesh is having a high prevalence of TB with 1518 reported cases per lac population against the national average of 216 per lac [4].
Diagnosis and treatment of TB in rural and remote location settings is a major challenge. The present day conventional methods of diagnosis requires sophisticated laboratory and repeated visits to hospitals. Social stigma associated with TB, poverty and work pressure for earning livelihood often leads to discontinuation of Antitubercular therapy by patients in developing and low income countries including India. The situation is further complicated in tribal populations practising social isolation, difficult terrains, varied ecological niches, poverty, illiteracy and superstitions. Development of MDR-TB and XDR-TB with higher mortality rates have emerged due to patient non compliance. The MDR-TB is defined as resistance against the two most potent anti-TB drugs, namely, Isoniazid (INH) and RIF. RIF is the most important drug in the treatment of TB. Infection by RR-MTB requires long therapeutic regimens with relatively more toxic second-line drugs [5]. Due to the high risk of transmission from person to person and the increase in prevalence of MDR-TB and XDR-TB, rapid diagnosis and antitubercular drug sensitivity is of paramount importance [6].
Although smear microscopy is a rapid and inexpensive technique for the detection of Acid-Fast Bacilli, it has poor sensitivity and low positive prognostic value. Culture is the “gold standard” for final determination and antitubercular sensitivity, but it is a slow process and can take up to 4-6 weeks to complete. Also, it requires sophisticated biosafety laboratory infrastructures with skilled human resource, which is largely not available in rural settings [7]. Thus rapid diagnosis coupled with drug sensitivity profiling is essentially required to check the progression and resistance development in TB. The GeneXpert MTB/RIF assay is a new integrated diagnostic tool that performs rapid diagnosis of TB as well as detection of RR in unprocessed sputum samples [8,9]. The test can be performed in ordinary laboratory conditions without isolation of MTB and is currently a suitable technique for rural settings.
Anuppur district is having high population of STs. The tribes live in isolated societies where TB is considered as a stigma. The TB patients do not visit hospitals easily and trust on alternative medicine, local healers or witchcraft. Poverty, illiteracy, lack of awareness and non availability of transport facilities further discourage them to seek treatment. The conventional methods of diagnosis using microscopy and culture delay the treatment initiation. The present study was aimed at GeneXpert MTB/RIF assay based rapid diagnosis of TB and RR detection in tribal population in District Anuppur, Madhya Pradesh.
Materials and Methods
Study Design
This was a retrospective study examining routinely collected patient data between April 2017-April 2018 at outpatient department of TB and Chest, District Hospital, Anuppur. Individuals of both sexes, aged between 0-90 years, with symptoms of PTB having chest pain, breathing difficulty, cough (usually with mucus), excessive sweating, particularly at night, fatigue, weight loss and low-grade fever were included in the study. Subjects without symptoms of TB were excluded from the study.
Sample Size
According to Census-2011, the total population of district Anuppur is 7,49,237, out of which 3,09,624 are tribes [10] The sample size was calculated using open EPI software (95% confidence level, power 50%, control to exposed ratio 1%).
IEC Approval
The sputum samples were considered to be medical waste material and non invasive methods of collection were used. The patient data was analysed anonymously; hence consent from the patients was not obtained. Approval of Institutional Ethical Committee was not required for this study.
Sample Collection
The sputum samples (413) were collected from males (267) and females (146) aged between 0-90 years, symptomatic for TB. The samples were processed for GeneXpert MTB/RIF assay.
GeneXpert MTB/RIF Assay
The analysis of sputum samples was performed as per manufacturer’s instructions. Briefly, the sputum was diluted with lysis buffer in a ration of 1:2 (v/v) and mixed vigorously. The mixture was incubated at room temperature for 10 minutes with intermittent manual shaking. Two (2.0) ml of the inactivated sputum sample was transferred to the GeneXpert test cartridge and loaded into the test platform. The machine was run as per given protocol and the electronic results were used for analysis [11].
Statistical Analysis
The data was analysed and expressed in percentage.
Results
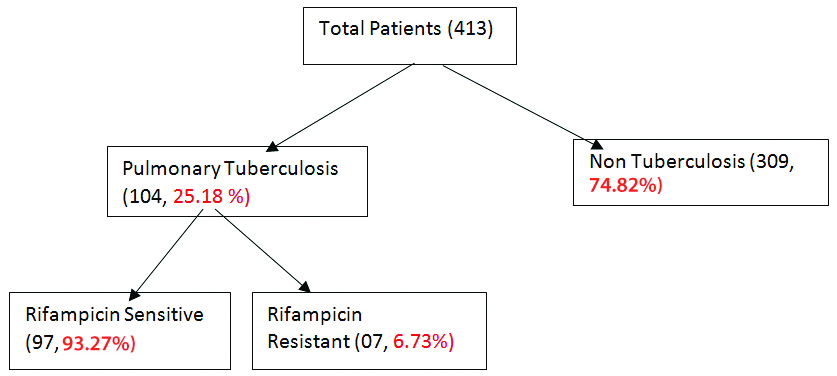
Of the 413 samples analysed by GeneXpert, TB was detected in 104 (25.18%) samples and 309 (74.82%) samples were negative for TB. The prevalence of TB among different age group is given in [Table/Fig-1]. Out of 104 TB positive samples, 66 (63.46%) were males and 38 (36.54%) females. RR was detected in 07 (6.73%) out of the 104 TB positive samples [Table/Fig-2].
Age wise distribution of TB patients.
| S. No. | Age group (in years) | Number of TB patients | Percentage (%) |
|---|
| 1. | 0-25 | 17 | 16.35 |
| 2. | 26-50 | 54 | 51.92 |
| 3. | 51-75 | 29 | 27.88 |
| 4. | 76+ | 4 | 3.85 |
Flow chart of analysis of sputum sample by GeneXpert.
The GeneXpert results indicated that the most prevalent mutation (five patients) responsible for RR was present at locus B. Mutation at locus C and E was reported in one patient each. There was no mutation at locus A and D [Table/Fig-3].
Probe wise pattern of Rifampicin Resistance (RR) In Tuberculosis (TB) Samples.
| Total RIF resistant | Prob-A | Prob-B | Prob-C | Prob-D | Prob-E |
|---|
| 07 | 00 | 05 (71.42%) | 01 (14.28%) | 00 | 01 (14.28%) |
Discussion
Anuppur district is one of the least developed districts of Madhya Pradesh and located around 600 Km from the state capital. All blocks of the district are having significant number of ST population. The main ST population in Anuppur district are Baiga, Gond, Panika, Kamars, Birhor, Bharias and Hill Korbas. There is no report on the prevalence of TB/MDR-TB in this region. Some of the earlier reports on Sahariya tribes in the Gwalior and Shivpuri districts of Madhya Pradesh have shown high prevalence of TB compared to the national rate [3]. In our study, among 413 subjects with symptoms, TB was detected in 104 (25.18%). In a similar study from six tribal dominated villages of four districts, namely Balangir, Dhenkanal, Kandhamal and Mayurbhanj of Odisha, out of 126 chest symptomatic, TB was detected in 35 (27.77%) subjects [12].
Although smear microscopy to detect presence of Acid-Fast Bacilli in clinical specimens is a rapid and inexpensive test, but it has low sensitivity for respiratory (54%) as well as non respiratory (50%) samples [13]. Earlier reports have shown that diagnosis of TB by smear microscopy is having low sensitivity as compared to culture methods because large bacillary load (105/ml) is required for a smear to become positive [14]. The conventional culture methods are used as ‘gold standards’ in TB diagnosis. However, these methods are time consuming and require high biosafety setup and trained laboratory personnel, which may only be available at large hospitals [15]. The culture-based methods for drug sensitivity analysis take 4-6 weeks. These conventional methods often result in compromised diagnosis and delay in treatment. TB being a ‘Poor Man’s’ Disease’, infect a large section of the population residing in rural and densely populated slums. It is very difficult for the poor patients to have frequent visits to hospitals for seeking treatment. The GeneXpert assay is a rapid, gene-based assay that can be used close to the point of care by operators with minimal technical expertise. Due to the advantage of its usage in rural settings with minimum laboratory set up, the assay is being used increasingly among developing countries having high burden of TB [16]. Apart from high diagnostic sensitivity, the technique also assess RR within 2-3 hours. The limits of detection of Xpert MTB/RIF lie in the range of 100-100 CFU/ml, compared with an estimated 10,000 CFU/ml for smear microscopy [14]. A recent literature review from 27 studies which included 9,557 participants showed that Xpert MTB/RIF assay had sensitivity of 89% (95% CI 85-92%) and specificity of 99% (95% CI 98-99%) in the diagnosis of pulmonary tuberculosis [17].
Our results indicated that the most common mutations conferring RR are located in the region of Probe B (71.42%), followed by Probe C (14.28%) and Probe E (14.28%), while no mutations were found in the region of Probe A and Probe D. Previous studies from India have shown that the most common mutation conferring RR is located in the Probe E region, codon 531 of the rpoB gene (TCG-TTG), in which serine is substituted with lysine [18]. RR by predominant mutation in probe E and B region has also been reported from Punjab, India [19]. Mutation in rpoB in the codon 516, which is in the Probe B region, and codon 526, which is in the Probe D region has also been reported [20]. Although, more studies are required for assessment of the high frequency (71.42%) of mutation at probe B, in District Anuppur, Madhya Pradesh, these mutations may be attributed to the use of a combination of antitubercular drugs, patients compliance profiles as well as local climatic and nutritional factors.
Limitation(s)
The high cost of consumable cartridge for Xpert MTB/RIF assay is a major limitation in India. Due to scarcity of funds, Xpert MTB/RIF assay could not be performed for all the patients visiting the TB centres/hospitals.
Conclusion(s)
Xpert MTB/RIF is a rapid, highly sensitive and specific assay for TB diagnosis and estimation of RR. The technique enables initiation of treatment after first visit to hospital and prescription of appropriate antitubercular therapy to rural and remote location population settings. In the present study, high rate of mutation was observed at probe B. However, other studies have reported high rate of mutation at probe E and B. For further confirmation of rate of mutation at different loci, the sample size and duration of study may be enhanced. Gene sequencing can be carried out in order to explain the higher rates of mutations at specific locus.
Author Declaration:
Financial or Other Competing Interests: As declared above
Was Ethics Committee Approval obtained for this study? NA
Was informed consent obtained from the subjects involved in the study? NA
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 08, 2020
Manual Googling: Jul 25, 2020
iThenticate Software: Aug 29, 2020 (22%)
[1]. World Health Organization. Global Tuberculosis Control: WHO Report 2010. 2010. (September 18, 2011). http://www.who.int/tb/publications/global_report/2010/en/index.html [Google Scholar]
[2]. Sharma RK, Roy J, Socio-economic and demographic characteristics of three most backward tribes of Madhya PradeshTribal Health 2016 23(1):63-68. [Google Scholar]
[3]. Raj P, Prakash R, Mishra G, Singh TD, Poojary S, Mehra NK, Prevalence of smear-positive pulmonary tuberculosis in different ethnic groups in India: Evaluation of public healthPub Health 2012 126:295-99.10.1016/j.puhe.2011.12.01622284444 [Google Scholar] [CrossRef] [PubMed]
[4]. Rao VG, Gopi PG, Bhat J, Selvakumar N, Yadav R, Tiwari B, Pulmonary tuberculosis: A public health problem amongst the Saharia: A primitive tribe of Madhya Pradesh, Central IndiaInt J Infect Dis 2010 14:e713-16.10.1016/j.ijid.2010.02.224320605504 [Google Scholar] [CrossRef] [PubMed]
[5]. World Health Organization. Companion Handbook to The WHO Guidelines for the Programmatic Management of Drug Resistant Tuberculosis, 2014, http://www.ncbi.nlm.nih.gov/books/NBK247420/ [Google Scholar]
[6]. World Health Organization. Global tuberculosis report 2016, http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf [Google Scholar]
[7]. Mark DP, Giorgio R, Alimuddin Z, Progress towards improved tuberculosis diagnostics for developing countriesLancet 2006 367:942-43.10.1016/S0140-6736(06)68386-4 [Google Scholar] [CrossRef]
[8]. Blakemore R, Story E, Helb D, Kop J, Banada P, Owens MR, Evaluation of the analytical performance of the Xpert MTB/RIF assayJ Clin Microbiol 2010 48:2495-501.10.1128/JCM.00128-1020504986 [Google Scholar] [CrossRef] [PubMed]
[9]. Helb D, Jones M, Story E, Boehme C, Wallace E, Ho K, Rapid detection of Mycobacterium tuberculosis and rifampicin resistance by use of on-demand, near-patient technologyJ Clin Microbiol 2010 48:229-37.10.1128/JCM.01463-0919864480 [Google Scholar] [CrossRef] [PubMed]
[10]. District- population Census 2011. https://www.census2011.co.in/district.php [Google Scholar]
[11]. Myneedu VP, Behera D, Verma AK, Bhalla M, Singh N, Arora J, Xpert W MTB/RIF assay for tuberculosis diagnosis: Evaluation in an Indian settingInt J Tuberc Lung Dis 2014 18(8):958-60.10.5588/ijtld.13.032825199011 [Google Scholar] [CrossRef] [PubMed]
[12]. Hussain T, Tripathy S, Das S, Satapathy P, Das D, Thomas B, Prevalence, risk factors and health seeking behaviour of pulmonary tuberculosis in four tribal dominated districts of Odisha: Comparison with studies in other regions of IndiaPlos One 2020 10.1371/journal.pone.022708332251467 [Google Scholar] [CrossRef] [PubMed]
[13]. Afsar I, Gunes M, Er H, Sener AG, Comparison of culture, microscopic smear and molecular methods in diagnosis of tuberculosisRev Esp Quimioter 2018 31(5):435-38. [Google Scholar]
[14]. Lawn SD, Nicol MP, Xpert® MTB/RIF assay: Development, evaluation and implementation of a new rapid molecular diagnostic for tuberculosis and rifampicin resistanceFut Microbiol 2011 6(9):1067-82.10.2217/fmb.11.8421958145 [Google Scholar] [CrossRef] [PubMed]
[15]. Hillemann D, Rüsch-Gerdes S, Boehme C, Richter E, Rapid molecular detection of extra pulmonary tuberculosis by the automated GeneXpert MTB/RIF systemJ Clin Microbiol 2011 49(4):1202-05.10.1128/JCM.02268-1021270230 [Google Scholar] [CrossRef] [PubMed]
[16]. Ullah I, Shah AA, Basit A, Ali M, Khan A, Ullah U, Rifampicin resistance mutations in the 81 bp RRDR of rpoB gene in Mycobacterium tuberculosis clinical isolates using Xpert MTB/RIF in Khyber Pakhtunkhwa, Pakistan: A retrospective studyBMC Infectious Diseases 2016 16:413-18.10.1186/s12879-016-1745-227519406 [Google Scholar] [CrossRef] [PubMed]
[17]. Steingart KR, Schiller I, Horne DJ, Pai M, Boehme CC, Dendukuri N, Xpert MTB/RIF assay for pulmonary tuberculosis and rifampicin resistance in adultsCochrane Database Syst Rev 2014 (1):CD00959310.1002/14651858 [Google Scholar] [CrossRef]
[18]. Singh UB, Pandey P, Mehta G, Bhatnagar AK, Mohan A, Goyal V, Genotypic, phenotypic and clinical validation of GeneXpert in extra-pulmonary and pulmonary tuberculosis in IndiaPLoS One 2016 11:e014925810.1371/journal.pone.014925826894283 [Google Scholar] [CrossRef] [PubMed]
[19]. Kaur R, Jindal N, Arora S, Kataria S, Epidemiology of rifampicin resistant tuberculosis and common mutations in rpoB gene of Mycobacterium tuberculosis: Aretrospective study from six districts of Punjab (India) using XpertMTB/RIF assayJ Lab Physicians 2016 8:96-100.10.4103/0974-2727.18078927365918 [Google Scholar] [CrossRef] [PubMed]
[20]. Reddy R, Alvarez-Uria G, Molecular Epidemiology of Rifampicin Resistance in Mycobacterium tuberculosis Using the GeneXpert MTB/RIF Assay from a Rural Setting in IndiaJournal of Pathogens. J Pathogens 2017 2017:673809510.1155/2017/673809529225973 [Google Scholar] [CrossRef] [PubMed]