Open fractures of the lower limb are common injuries presenting emergency. Road traffic accident is one of the major causes. Following damage control orthopaedic procedures, definitive management of these fractures are always a challenge. Frequently, these fractures result in amputations, infection, non-union and limb length discrepancy [1]. Infected non-union can be a difficult problem to solve. The presence of bone loss, deformity, infection or failure of previous internal fixation further complicates the problem [2].
Treatment of non-union is a challenging task and various treatment modalities have been recommended. Non-invasive and semi-invasive methods for non-union of long bones like electric stimulation, low-intensity pulsed ultrasound and extracorporeal shock wave therapy have been studied [3-7]. Internal fixation methods like interlocking nail and plate-screw fixation and external fixation with Ilizarov ring fixator and monolateral external fixator are in routine use. The skin and soft tissue are in poor condition in these cases owing to discharging sinuses, extensive scarring, presence of skin grafts and muscle flaps. This makes use of internal fixation difficult and causes frequent wound complications. To address these problems, the principle distraction osteogenesis was given by Ilizarov in 1950 [8]. The monolateral rail fixator is designed on Ilizarov’s principles of distraction osteogenesis and is also used for the treatment of non-union of long bones [9,10]. Use of Ilizarov ring fixator has been very successful and popular, but is cumbersome and has a high learning curve [11-13]. The monolateral external fixator was designed to function on Ilizarov’s principles and has gained popularity in treatment of non-union of tibia.
Various studies have been done using LRS and segment transport to treat infected non-union of long bones with predictable good results [9,10,14]. The aim of this study was to evaluate the radiological and functional outcome of infected non-union of Tibia with or without bone lose treated with LRS.
Materials and Methods
This prospective cohort study was conducted in Department of Orthopaedic Surgery of a Tertiary Care Centre, from September 2016 to August 2017.
All the patients were briefed in detail about the procedure and also regarding prolonged treatment with fixator, bone transport, persistence of infection and limitation in terms of functions, if any after the procedure. A detailed and informed written consent was obtained from each patient. This study was conducted after obtaining ethical approval from competent authority of the institute.
Inclusion and Exclusion criteria: Total of 21 patients with infected non-union of tibia were included in this study. Any patient, who refused treatment with LRS or not willing to accept the procedure and possible complications, was not included in this study. Also, patients with very bad skin condition in the transportable segment or exposed bone were not included in the study.
All the patients were operated by a senior orthopaedic surgeon who had a long experience of treating these patients with LRS. The surgical approach to the non-union site was individualised in every case based on the presence of flaps, skin grafts and discharging sinuses. The incision was deepened up to the bone so as to obtain a full thickness flap including the periosteum. Debridement of dead and necrotic tissues was performed. Freshening of the fracture ends was done and bleeding bone surfaces were obtained. Intramedullary fibular strut grafting and reduction of fracture was done if required. The fibular strut was tailored by splitting the graft along the longitudinal axis, in cases where the fibula did not fit the medullary canal. Alignment was held temporarily using K-wires when necessary. LRS was used to stabilise the fractures. Compression at fracture site was obtained using compression-distraction unit. Limb lengthening was performed in cases where limb length discrepancy was more than 2.5 cm [15]. A corticotomy was performed and limb lengthening was done at the rate of 1 mm per day by rotating the CD unit at six hourly intervals [16]. Weight bearing as tolerated was allowed in the postoperative period and compensatory shoe-raise was given. Knee and ankle mobilisation exercises were encouraged.
The clinical and radiological outcome of these patients was recorded at regular follow-up. The outcome was assessed according to Association for the Study and Application of the Methods of Ilizarov (ASAMI) scoring system as described by Paley D et al., [Table/Fig-1] [8].
ASAMI scoring system [8].
| Result | Bone results | Functional results |
|---|
| Excellent | UnionNo infectionDeformity <7 degreeLimb length inequality <2.5 cm | Active, no limp, minimum stiffness (loss of <15 degree knee extension/<15 degree dorsiflexion of ankle), no RSD, insignificant pain |
| Good | Union with any two of the following:Absence of infection, <7 degree deformity and limb length inequality of <2.5 cm | Active with one or two of the following:limp, stiffness, RSD, significant pain |
| Fair | Union with only one of the following:Absence of infection, deformity <7 degree,limb length inequality of <2.5 cm | Active with three or all of the following:limp, stiffness, RSD, significant pain |
| Poor | Non-union/refracture/union+infection+deformity >7 degree+limb length inequality >2.5 cm | Inactive (unemployment or inability to return to daily activities because of injury) |
| Failure | | Amputation |
RSD: Reflex sympathetic dystrophy
Statistical Analysis
Data was collected on a Microsoft Excel sheet, SPSS (IBM SPSS statistics 24.0) used for analysis. Mean, median and mode were used to describe continuous variables. Frequency tables were used to describe categorical variables.
Results
Out of 21 patients, 19 were males and two were females. The mean age of patients was 29.43±14.07 years. The mean limb length discrepancy was 23.3 mm (range, 15-40 mm). The mean duration from injury to LRS application was 7.9 months (range, 6-12 months). Mean duration of follow-up was 29.5 months (range, 16-50 months) [Table/Fig-2].
| S. No. | Age (years) | Sex | Postoperative infection | Corticotomy | Limb length discrepancy (mm) | ASAMI bone result | ASAMI functional result | External fixation time (months) | Duration of follow-up (months) |
|---|
| 1 | 40 | M | Yes | No | 15 | Good | Excellent | 16 | 32 |
| 2 | 61 | M | No | Yes | 30 | Good | Good | 18 | 50 |
| 3 | 31 | M | No | No | 15 | Excellent | Excellent | 12 | 41 |
| 4 | 29 | F | Yes | Yes | 35 | Fair | Good | 8 | 36 |
| 5 | 25 | M | No | No | 25 | Good | Good | 6 | 20 |
| 6 | 7 | F | No | No | 15 | Excellent | Excellent | 8 | 18 |
| 7 | 35 | M | Yes | Yes | 30 | Fair | Fair | 9 | 32 |
| 8 | 23 | M | No | No | 15 | Excellent | Excellent | 11 | 28 |
| 9 | 17 | M | No | Yes | 30 | Good | Good | 12 | 36 |
| 10 | 35 | M | No | No | 15 | Excellent | Excellent | 16 | 26 |
| 11 | 13 | M | No | No | 20 | Excellent | Excellent | 14 | 28 |
| 12 | 25 | M | No | Yes | 35 | Good | Good | 9 | 19 |
| 13 | 40 | M | Yes | No | 20 | Good | Good | 8 | 16 |
| 14 | 23 | M | No | No | 20 | Excellent | Excellent | 9 | 17 |
| 15 | 17 | M | No | Yes | 35 | Good | Good | 12 | 36 |
| 16 | 35 | M | No | No | 15 | Excellent | Excellent | 10 | 26 |
| 17 | 13 | M | No | No | 20 | Excellent | Excellent | 14 | 28 |
| 18 | 25 | M | No | Yes | 40 | Good | Good | 12 | 19 |
| 19 | 40 | M | Yes | No | 15 | Good | Excellent | 8 | 32 |
| 20 | 61 | M | No | Yes | 30 | Good | Good | 13 | 50 |
| 21 | 23 | M | No | No | 15 | Excellent | Excellent | 10 | 30 |
| Mean | 29.43 yrs | | 23.33 mm | | 11.19 months | 29.52 months |
Corticotomy and bone lengthening were performed in eight cases. The mean external fixation time was 11.2 months (range, 6-18 months). The mean follow-up time was 29.52 months (minimun 16 months to maximum 50 months).
All the patients were allowed walking with support as soon as they tolerated fixator and were allowed to do full weight walking once the fixator was removed after bony union and consolidation of the regenerate.
According to ASAMI classification of outcomes, bone results were excellent in nine cases, good in 10 cases, and fair in two cases. There was fair bone result in one patient who sustained a re-fracture six weeks after fixator removal. Infection was the only complication listed. The procedure was repeated and union was achieved subsequently. The ASAMI functional results were excellent in 11 cases, good in nine cases and fair in one case.
Infection persisted after bone union in five cases in the form of sinus. All these sinuses were repeatedly curetted and healed in due course. No further active procedure was required. Pin tract infection was seen in four cases after fixator removal which subsided after curettage of the tract [Table/Fig-3,4].
Preoperative (a), postoperative (b) and final X-ray images (c) of infected non-union tibia with bone loss treated with LRS and bone transport.
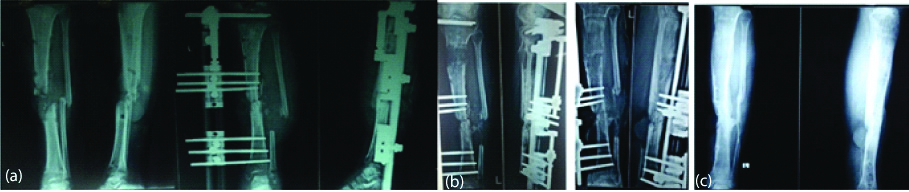
a) Preoperative and intra-operative, b) postoperative c) final functional results of segmental bone loss of tibia with infection treated with LRS.

Discussion
A prospective cohort study was done in Department of Orthopaedic Surgery of a tertiary care centre to evaluate the clinical and functional results of the patients on infected non-union of tibia with or without gap treated with LRS application and segment transport, if required. The study achieved excellent and good results in 90% of cases as per ASAMI functional and bony score.
The results are similar to the studies from literature. In a study of 25 patients of non-union of tibia by Paley D et al., bone results were excellent in 18 cases, good in five cases and fair in two cases. The functional results were excellent in 16 cases, good in seven cases, fair in one case and poor in one case [8]. In a study of 66 patients of infected tibial non-union by Yin P et al., the bone results were excellent in 44, good in 15, fair in five and poor in two cases [17]. The functional results were excellent in 24, good in 26, fair in 10 and poor in none. In a study of 37 patients with non-union of lower extremity long bones managed by monolateral external fixation; Harshwal RK et al., reported that bone results were excellent in 24 cases, good in nine cases, fair in one and poor in three cases. The functional results were excellent in 27 cases, good in six cases, fair in one case and poor in three cases [18].
Mudiganty S et al., in his study about infected non-union of femur and tibia treared with RAIL fixator showed that bone results were excellent in 57.5%, good in 40%, fair in 0% and poor in 2.5% cases, while functional result was excellent in 32.5%, good in 65%, fair in 0% and poor in 2.5% cases. Rail fixation system was thus recommended as an excellent alternative method to treat infected gap non-union of femur and tibia [10].
There was persistence of infection following bone union in five of the index cases. The use of intramedullary fibula as a strut graft additionally aided in the application of the fixator by maintaining the reduction and alignment intraoperatively. Gopisanker G et al., demonstrated good results in seven cases where intramedullary fibular strut was used in cases of infected non-union of Humerus [19]. Fracture union was achieved in all patients in the present study. Pin tract infection was found in four patients after fixator removal and they required curettage of the pin tracts. Preoperatively stiffness of ankle joint and knee joint was present in two and one case, respectively. None of the patients developed stiffness of knee or ankle joints after surgery.
Limitation(s)
The study is limited by a small sample size and the results may not reflect the true efficacy and complications associated with the procedure.
Conclusion(s)
The use of monolateral rail external fixator (LRS) is an effective method for the treatment of infected non-union of tibia augmented with a fibular strut graft. This provides good results in terms of bony union, subsidence of infection and functional results.
RSD: Reflex sympathetic dystrophy