The advent of Computed Tomography (CT) and its universal availability has paved way for new dimensions in medical world, in appropriate diagnosis and treatment of the diseases. Multi detector Computed Tomographic (MDCT) examination of the chest is routinely performed for various clinical indications. The detailed evaluation of the scans reveals additional unsuspected findings which may not be relevant to the clinical indication. Assessment of the mediastinal vasculature and its measurements should be part of the routine thoracic CT analysis [1]. The measurement of the PA vascular diameter indirectly reflects the pressures within. Several studies have been performed to measure the PA diameter, and have shown that the increase in the MPAD is associated with an increase in pulmonary pressure. Thus, it reflects the presence of PA Hypertension (PAH) [2-5]. PAH is caused by variety of disorders and could be occult before its clinical presentation. Hence, presence of dilated arteries incidentally detected at CT could help in early diagnosis and institution of therapy which can reduce the associated morbidity and mortality [1].
The gold standard test for measuring Pulmonary Artery Pressure (PAP) is right cardiac catheterisation. However, this is an invasive procedure and carries inherent risks and complications [6,7]. Therefore, researchers have carried out several studies, such as those by Edwards PD et al., Wittram C, Bozlar U et al etc., seeking a reliable and reproducible non invasive imaging method to predict the PAH [8-10]. These include echocardiography and PA diameter measurements at chest X-ray. Some investigators have found reasonable correlations with right descending PA size and PAP in studies with chest radiography. However, this measurement at chest radiography is not a reliable method. Numerous factors contribute to the problem, such as superposition of the mediastinal and hilar structures, concurrent parenchymal diseases, architectural distortion and magnification differences [11,12]. With the helical CT, measurement of PA diameter is nearly accurate and reproducible. It is also well known that, there exists a relationship between diameter of MPA and AA diameter in an individual [4,13,14]. The MPA to AA diameter ratio of less than 1 is generally accepted as normal and this ratio has shown to be independent of physiological variables like sex and body surface area [15]. Novelty of this study is to establish normal range of MPAD and its relation to AA in Indian population, as sizes of anatomical organs do depend on race and built of the population which would be specific to a particular region. To the best of our knowledge, no single large study has been published demonstrating the range of normal diameter of MPA in Indian population. Hence, this study was undertaken to know the normal reference values of the pulmonary arteries with age and sex-specific distribution.
Materials and Methods
This was a prospective cross-sectional study conducted between October 2018 and September 2019 among patients who had clinical indication for Contrast Enhanced CT (CECT) scan of thorax such as cough for evaluation, suspected lung nodule, chest wall lesions, primary or secondaries in the lung at chest X-ray etc. All subjects underwent echocardiography after the CT scan and patients with elevated PAP were also this should be included. Subsequently, 500 subjects (380 males, 120 females) between the age of 30-65 years were included in the study. Those individuals with chronic illness like those having hypertension, current and past smokers, chronic obstructive pulmonary disease, history of pulmonary embolism, diabetics, obesity, cardiovascular disease and heart valvular surgery were excluded from the study.
Sample size calculation:
Formula: n=4pq/d2
where, n-sample size, p-prevalence (according to PLOS study) [16]. q-(1-p), d-absolute error, CI-confidence interval, p=31.9%, q=68.1 (1-p), d=4.5%, CI=95%, Substituting the values, n=4×31.9×68.1/(4.5)2=429~500, The sample size chosen for the current study was 500.
The CT examination of thorax was performed in Philips 128-slice CT scanning system with breath holding from the level of thoracic inlet to the upper pole of the right kidney. Non ionic iodinated (300 mg I/100 mL) contrast material with volume depending on patient body weight was given intravenously (1-2 mL/kg body weight). Scanning was acquired about 20 seconds after the start of contrast material injection. CT Imaging parameters were 120 kV and 200 mAs, 0.5 seconds rotation time, 128×0.625 mm collimation, 2 mm slice thickness, 52 cm Field Of View (FOV) and 512×512 matrix were used.
Data were transferred to a dedicated Philips workstation and diameters were measured in mediastinal window using a window level of 350 HU, with the centre at 50 HU. The maximum diameter of MPA was measured at the level of its bifurcation, perpendicular to its long axis. At the same level, diameter of AA was also measured [Table/Fig-1]. The outer limits of the contrast column were considered to determine the vessel diameter. Measurements were done by two general radiologists on a PACS work station. Each observer performed three measurements for each subject. The average of six measurements was accepted as the mean artery diameter.
Axial CECT image of Ascending Aorta (AA) and Main Pulmonary Artery (MPA) measured at its bifurcation.
Statistical Analysis
SPSS version 20. {IBM SPASS statistics (IBM corp. Armonk, NY, USA released 2011)} was used to perform the statistical analysis. Quantitative variables were described in terms of descriptive statistics like mean and standard deviation. Inferential statistics like Unpaired t-test was used to test the significant difference for quantitative variables between the two groups. The level of significance was set at 5%.
Results
The present study group consisted of 500 subjects comprising of 380 male and 120 female population. Mean age of overall population was 46.22±15.64 years. The MPA diameters of whole population ranged between 15.6-31.6 mm, with mean diameter of 23.08±2.81 mm [Table/Fig-2,3]. The mean MPA diameter of female subjects was 23.17±2.57 mm and ranged between 17.4-31.6 mm whereas in male subjects, mean MPA diameter was 23.0±3.0 mm and ranged between 15.6-31.4 mm [Table/Fig-4]. It was noted that the mean MPA diameter in females was slightly higher than in males, but the difference was not statistically significant (p=0.207). Eliminating the extreme values on both side of curves i.e., (lower 2.5% and upper 2.5%), the remaining 95% values were considered as normal range. Thus, we found the normal range of upper and lower limits of the MPA diameters to be 28.7 mm and 17.5 mm. AA diameters showed a homogeneous distribution; the CT-determined mean AA diameter was 27.15±2.6 mm. The mean AA diameter in males was 27.76±3.2 mm, and 26.67±2.0 mm in females with statistical significance (p-value 0.001) between the groups [Table/Fig-4]. The mean ratio of MPA to AA in whole population, males and females was found to be 0.85, 0.83 and 0.87, respectively.
Tabular representation showing positive correlation (weak) between age and diameter of Main Pulmonary Artery (MPA).
| Parameters | Mean | SD | Correlation | p-value |
|---|
| Age (in years) | 46.22 | 15.64 | 0.191 | 0.001 |
| MPA (mm) | 23.08 | 2.81 |
*Unpaired t-test
Scatter graph showing positive correlation between age and diameter of Main Pulmonary Artery (MPA).
(p-value <0.001)
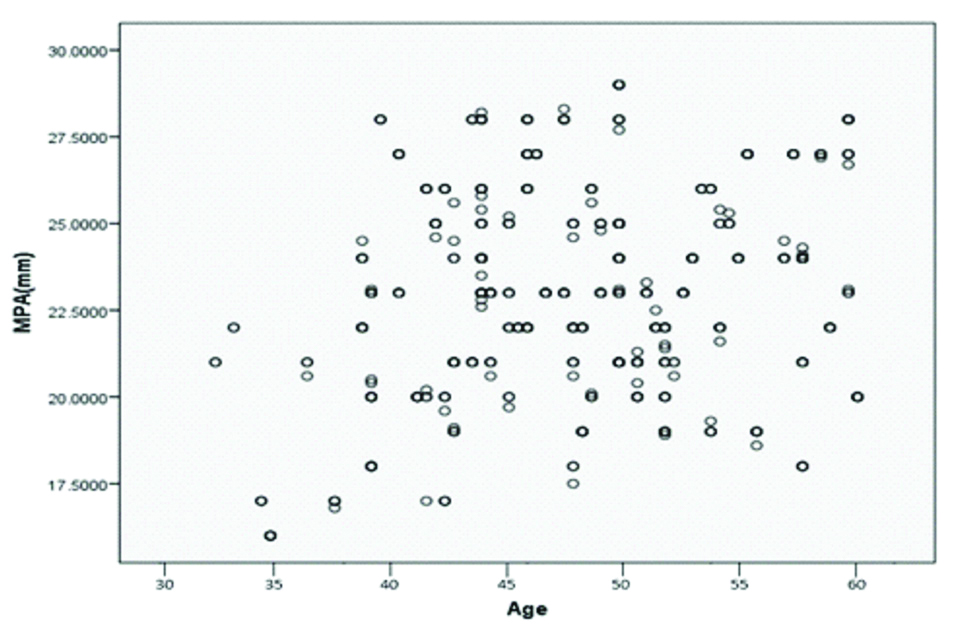
Table depicting the sex specific mean values of the age, MPA and AA including p-value.
| Variable | Gender | n | Mean | SD | Mean diff | t-ratio* | p-value |
|---|
| Age (years) | Male | 380 | 43.37 | 17.049 | -5.715 | -3.322 | 0.001 |
| Female | 120 | 49.08 | 14.275 |
| MPA (mm) | Male | 380 | 23.0 | 3.063 | -0.390 | -1.262 | 0.207 |
| Female | 120 | 23.17 | 2.571 |
| AA (mm) | Male | 380 | 27.76 | 3.252 | 1.096 | 3.478 | 0.001 |
| Female | 120 | 26.67 | 2.063 |
MPA: Main pulmonary artery; AA: Ascending aorta; *Unpaired t test
Discussion
Right atrial catheterisation is the standard method of choice to measure pulmonary arterial pressures [6,7]. CT is one among the common non invasive technique used to measure the PA and aortic diameters, which indirectly reflects the pulmonary pressures and therefore, predicts the presence of pulmonary hypertension. The measurements obtained by this technique are nearly accurate and reproducible [8]. The current study was conducted to establish the normal range of PA diameter and MPA to AA diameter ratio among Indian population.
Various parameters such as age, sex, height, body surface area, body mass index and associated comorbidities like, cardiovascular and pulmonary diseases affects the size of pulmonary arteries [9,10]. According to Wittram C, the normal values of MPA should be correlated with variables like age, sex, height and body surface area [9]. However, in a study by Bozlar U et al., the PA diameters showed weak/medium correlation with many of these variables [10]. A direct relationship was found betweenMPAD and age i.e., increase in age was associated with increase in MPAD [Table/Fig-2,3], in agreement with Bozlar U et al., [10]. This was statistically significant (p=0.001). The mean MPAD in female population (23.17 mm) were slightly higher than in male population (23.0 mm). However, this difference is not significant (p=0.207). This is contrary with the study by Edwards PD et al., [8]. This insignificant difference could be explained owing to the overall higher age of the females represented in the current study. The correlation between the MPAD and the other physiological variables such as BMI, were not evaluated in the present study.
The mean MPAD of the entire subject population, range of MPA diameters and the range of upper and lower limits of the MPAD in the present study population were consistent with Bozlar U et al., and Wani AH et al., [10,12].
Generally, in normal individuals, the diameter of the AA is more than the MPA measured at its bifurcation. Hence, the ratio of MPA and AA diameter is less than 1 [4,13,15]. In a study by Lee SH et al., the 90th percentile sex-specific MPA, AA, and MPA/AA ratio values determined in healthy reference group were, 31.3 mm, 36.8 mm, and 1.05 in males, and 29.6 mm, 34.5 mm, and 1.03 in females, respectively [16]. In this study, the Mean MPA/AA ratio in whole study population was 23.08/27.1 i.e., 0.85. The mean ratio of MPA to AA in males was found to be 23.0/27.7 i.e., 0.83 and in females was 23.17/26.6 i.e., 0.87. Interestingly, the ratio remained within 0.85 even in subjects with MPAD above 30 mm. Hence, it becomes inappropriate to categorise individuals as having PAH based on PA values alone. Thus, the ratio of MPA to AA diameter appears to be very important to categorise patients with or without pulmonary hypertension.
Limitation(s)
In the present study, the influence of physiological parameters such as weight, height and body surface area of individuals was not taken into consideration. Hence, influence of these parameters on diameters of PA could not be established. It is of importance to state here that, it is difficult to establish an absolute cut-off point of MPAD to define the presence or absence of pulmonary hypertension in this study. Since, the study population did not include patients with pulmonary hypertension and hence, the comparison of the MPAD in patients with PAH and without PAH could not be made, to arrive at a conclusion.
Conclusion(s)
The MDCT assessment of MPA diameter and its ratio with AA is simple, easily obtained and reproducible. In the present study, the upper limit of normal MPA diameter was found to be 28.7 mm and the mean MPA to AA diameter ratio was 0.85. The correlation between age and MPAD was statistically significant, while sex-specific MPAD was insignificant. Further studies are needed to establish the effects of other physiological variables on the size of MPA.
*Unpaired t-test
MPA: Main pulmonary artery; AA: Ascending aorta; *Unpaired t test