Thrombocytopenia (TCP) is a common medical condition associated with a wide variety of diseases. By definition, TCP is defined as a subnormal number of platelets in circulating blood. Platelet counts below 1,50,000 per microliter define TCP, but they do not reveal the underlying pathophysiology [1]. During evaluation of thrombocytopenic patients, it is essential to know whether it is due to hypoproduction, hyperdestruction or abnormal platelet pooling as this will aid in targeted management of the patient, thereby avoiding unnecessary investigations and narrowing the differentials [2]. Automated haematology analysers have now largely replaced labour intensive and time consuming methods in laboratories and health care centres worldwide. These analysers other than platelet count also provide outputs of platelet indices like MPV, PDW, and PCT routinely in minutes without any extra cost [3-5]. But these parameters are at times overlooked in patient management, with the main emphasis being only on the platelet count [6]. A good basic knowledge on their interpretation can be a useful adjunct tool along with supporting clinical data to bottom down the aetiology of TCP, thereby aiding in better patient care. This study was undertaken with the aim to determine if studying the variation in platelet indices helps to identify the aetiology of TCP. The objectives of the study were to categorise the platelet indices in adult patients with respect to the underlying mechanism of TCP and to study the significance of variation in platelet indices with underlying mechanism and also according to the severity of TCP.
The novelty of present study is that in addition to the aetiology, variation of platelet indices in each group depending on the severity of fall in platelet counts were studied.
Materials and Methods
This prospective study was conducted in the Haematology Department of Sapthagiri Institute of Medical Sciences and Research Centre located in Bangalore, Karnataka, India over a period of three months from June 2019 to August 2019. Institutional Ethical Committee clearance was taken. (Ref no.- IEC NO: SIMS and RC/IECC/5/2019). Purposive sampling was done for calculating the sample size. The adult thrombocytopenic cases were those referred from various clinical departments for blood investigations. Ethylene-diamine-tetraacetic acid (EDTA) anti-coagulated venous samples were run within four hours of sample collection in the autoanalyser Sysmex XN-550. Platelet parameters obtained included- PCT, PDW and MPV. A peripheral blood smear stained with Leishman stain was also reviewed wherever necessary with Olympus CX21i microscope, which also helped to rule out pseudo-thrombocytopenic cases. These parameters were standardised by routine external and internal quality control checks. Relevant clinical data, demographic details, working diagnosis and supportive investigations along with serological test results of the cases were collected using the laboratory information system, maintaining the patient’s anonymity. The cases were categorised into three groups based on the mechanism of TCP. Group 1- Hyperdestructive TCPs, Group 2 Hypoproductive TCPs and Group 3 includes- TCPs due to Abnormal pooling.
Inclusion criteria: Adult patients aged ≥18 years of both sexes with a platelet count of less than 1,50,000 and with sufficient clinical details and informed consent.
Exclusion criteria: Patients on medications causing TCP and those on anti-platelet drugs were excluded. Patients with insufficient clinical details and working diagnosis.
Statistical Analysis
The data collected was entered in excel sheet and was analysed using the Software SPSS version 20. Platelet parameters of patients with TCP in the three aetiological categories (Hyperdestructive, Hypoproductive and Abnormal pooling groups) were statistically tested by one-way ANOVA test. A p-value of <0.05 was considered as statistically significant.
Results
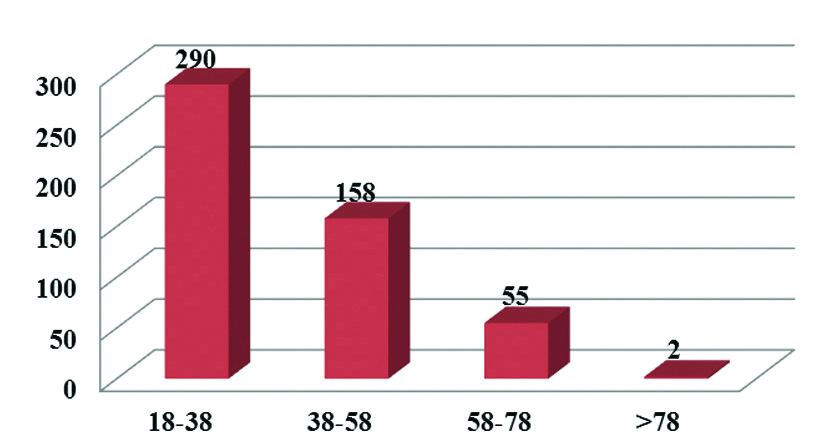
The present study was done over a period of three months and included a total of 598 cases of adult TCP. A total of 93 cases were excluded as they did not meet the inclusion criteria as mentioned. Among the 505 cases taken for the study, majority fell into the age group of 18-38 years [Table/Fig-1].
Figure showing age distribution of cases.
X axis: Age range in years; Y axis: Number of cases
Of the total cases, 295 were males and 210 were females with male: female ratio being 1.4:1. These cases were categorised into three groups based on the mechanisms of TCP. Group 1- Hyperdestructive TCPs, Group 2- Hypoproductive TCPs and Group 3- TCPs due to abnormal pooling [Table/Fig-2]. Under the hyperdestructive group (Group 1) were the cases of viral fevers (dengue included), sepsis, malaria, liver and renal diseases, Immune Thrombocytopenic Purpura (ITP) and cardiac diseases. Hypoproductive group included cases presenting with anaemia, leukaemias/Myelodysplastic Syndromes (MDS) and pancytopenias. Group 3 had Splenomegaly [Table/Fig-2]. Simultaneous study of peripheral smears helped to rule out the EDTA induced TCPs.
Distribution of thrombocytopenic cases in each group.
| Aetiologies | Causes | No. of cases (%) |
|---|
| Group 1(Hyperdestructive)420 cases (83%) | Viral fevers (Dengue included) | 292 (69.5%) |
| Sepsis | 55 (13.1%) |
| Malaria | 11 (2.6%) |
| Liver diseases | 26 (6.2%) |
| Renal diseases | 12 (2.9%) |
| Cardiac diseases | 10 (2.4%) |
| ITP | 14 (3.3%) |
| Group 2(Hypoproductive)72 cases (14%) | Anaemia | 53 (73.6%) |
| Leukaemias/MDS | 13 (18.1%) |
| Pancytopenia | 6 (8.3%) |
| Group 3(Abnormal pooling)13 cases (3%) | Splenomegaly | 13 (100%) |
For the next part of the study three categories of TCPs were made according to the severity as follows: Group A- <50,000/cmm, Group B- 50001-1,00,000/cmm and Group C- 1,00001-1,50,000/cmm [Table/Fig-3].
Distribution of cases according to the severity of thrombocytopenia (TCP).
| Severity of Thrombocytopenia* | No. of cases (%) |
|---|
| Group A | 166 (32.87%) |
| Group B | 219 (43.37%) |
| Group C | 120 (23.76%) |
| TOTAL | 505 |
*Group A: Platelet count- <50000/cumm, Group B: Platelet count-50001-100000/cumm, Group C: Platelet count-100001-150000/cumm.
The statistical analysis showed that there was significant variation among the platelet indices (Platelet count, MPV, PDW) in the three groups of TCPs in terms of aetiologies. PCT though showed significant variation was of a lesser degree than the other indices [Table/Fig-4]. The statistical analysis showed that the platelet indices (PCT, MPV, PDW) varied significantly with the severity of thrombocytopenia [Table/Fig-5].
Table showing mean, standard deviation and p-values of platelet parameters in different aetiologies of Thrombocytopenia (TCP).
| Platelet parameter | Aetiologies of Thrombocytopenia (TCP) | N | Mean | Std. deviation | p-value |
|---|
| Platelet Count | Group 1 | 420 | 74309.76 | 34662.468 | 0.008** |
| Group 2 | 72 | 60472.22 | 35745.569 |
| Group 3 | 13 | 76384.62 | 37382.122 |
| Total | 505 | 72390.30 | 35155.372 |
| PCT (%) | Group 1 | 420 | 0.084 | 0.047 | 0.02* |
| Group 2 | 72 | 0.066 | 0.040 |
| Group 3 | 13 | 0.097 | 0.050 |
| Total | 505 | 0.080 | 0.047 |
| MPV (fl) | Group 1 | 420 | 11.870 | 1.304 | 0.001** |
| Group 2 | 72 | 10.509 | 1.328 |
| Group 3 | 13 | 12.538 | 1.441 |
| Total | 505 | 11.694 | 1.399 |
| PDW (%) | Group 1 | 420 | 15.637 | 3.417 | 0.001** |
| Group 2 | 72 | 11.719 | 3.085 |
| Group 3 | 13 | 16.531 | 4.138 |
| Total | 505 | 15.101 | 3.658 |
Group 1: Hyperdestructive, Group 2: Hypoproductive, Group 3: Abnormal pooling
**Significant p-value <0.05 MPV: Mean platelet volume; PCT: Plateletcrit; PDW: Platelet distribution width
Table showing mean, standard deviation and p-values of platelet parameters. According to the severity of Thrombocytopenia (TCP).
| Platelet parameters | Severity of Thrombocytopenia (TCP) | N | Mean | Std. deviation | p-value |
|---|
| PCT (%) | Group A | 166 | 0.037 | 0.016 | 0.001** |
| Group B | 219 | 0.082 | 0.028 |
| Group C | 120 | 0.138 | 0.042 |
| Total | 505 | 0.080 | 0.047 |
| MPV (fL) | Group A | 166 | 11.380 | 1.218 | 0.002** |
| Group B | 219 | 11.837 | 1.453 |
| Group C | 120 | 11.867 | 1.470 |
| Total | 505 | 11.694 | 1.399 |
| PDW (%) | Group A | 166 | 14.190 | 3.486 | 0.001** |
| Group B | 219 | 15.613 | 3.634 |
| Group C | 120 | 15.428 | 3.725 |
| Total | 505 | 15.101 | 3.6583 |
Group A: Platelet count- <50000/cumm, Group B: Platelet count-50001-100000/cumm, Group C: Platelet count-100001-150000/cumm; **Significant p-value <0.05
MPV: Mean platelet volume; PCT: Plateletcrit; PDW: Platelet distribution width
Discussion
Platelets being one among the blood elements, play a vital role in the clotting cascade and help in preventing bleeding. The platelets are produced from the megakaryocytes, with their mother cells in the bone marrow. A platelet count below 1,50,000 per microliter is the standard definition of TCP as accepted worldwide [7,8]. TCP is a commonly encountered condition in clinical practice that leads to the clinicians ordering many other investigations to narrow down the cause of the same [9]. The underlying mechanisms of TCP can be broadly be categorised as hyper destructive causes, hypo- productive causes and those due to abnormal splenic pooling [8]. With the beginning of automation in haematology and the advent of auto analysers, automated cell counters are now used all over the world to measure the various blood indices. The analysers have the advantage of not only being quick but also are able to throw light on a wide variety of indices and also minimise the inter-observer bias to a certain extent [2,10]. A manual smear can give an idea about the morphology and platelet count; however, it is time consuming and does not contribute to the other parameter details [4]. Also, the platelet count, when interpreted in conjunction with other platelet indices gives a complete picture of platelet maturity and function [4]. Other than the routine platelet counts, which is the most commonly asked parameter, the other platelet indices like MPV, PCT and PDW are also available in the analyser readings [9,10]. Assessing these parameters by correlating them with the mechanism of TCP can give an insight into the probable aetiology of the same and help in narrowing down the diagnosis.
Majority of the thrombocytopenic cases in present study fell into the third decade of life, with the male to female ratio being 1.4:1 in the thrombocytopenic patients, similar to the study done by Borkataky S et al., [11]. TCP can be due to either peripheral destruction (destructive TCP) or due to inadequate production (hypoproliferative TCP). A third less common cause is abnormal splenic sequestration of the platelets causing splenomegaly [12]. Hyperdestructive TCP category includes idiopathic TCP, malaria, Kala-azar, dengue fever, renal diseases, cardiac diseases, sepsis and viral fevers [11,12]. In present study, cases of hyperdestructive TCP predominated (83%), followed by hypoproductive cases (14%) and abnormal pooling (3%) causes similar to other studies by Parveen S and Vimal M, Reddy RS et al., Katti T et al. and Numbenjapon T et al. [2,13-15]. Dengue cases predominated the hyperdestructive group as the study was done during the early monsoon which is the peak season for this entity. Hypoproliferative group, included anaemias, acute leukaemias and chronic lymphocytic leukaemias (with marrow infiltration), post chemotherapy cases and myelodysplatic syndromes [16]. As most of the patients were from rural background, it was no surprise that a higher percentage of cases fell into the anaemic aetiology in the hypoproductive group.
MPV is a platelet parameter which reflects change in either platelet stimulation or rate of platelet production and gives an average size of the platelet, normal range being from 7.5 to 11.5 fl [16]. Increase in MPV reflects the attempt of the bone marrow to compensate the platelet loss by releasing young platelets that are seen on smear as giant platelets. Previous studies have reported the mean MPV value in the hyperdestructive group to be significantly higher than in the hypoproductive and abnormal pooling groups [2,8]. The mean cut-off of MPV in present study in the hyperdestructive group was found to be significantly higher (11.8fl). The MPV in hypoproductive group in our study was 10.5 fl which is close to the study done by Negash M et al., [6]. In contrast, Nakadate H et al., and Baynes RD et al., found no significant difference in MPV between the groups [17,18]. PCT is a value depicting the volume percentage of the platelets and is not altered by the severity of TCP in either of the three mechanisms, with the same being concluded in present study too. The PCT does not appear to provide any information of clinical value [2,19]. The present study revealed that mean PDW was significantly higher in hyperdestructive group as compared to the hypoproductive and abnormal pooling group. Other authors like Katti T et al., Kaito K et al., Khaleel KJ et al., Ntaios G et al., and Shah AR et al., also reported that PDW was higher in the hyperdestructive group as compared to the hypoproductive thrombocytopenic patients, which reflected an increase in the production rate of platelets [14,20-23]. Platelets with an increased number and size of pseudopodia differ in size, possibly affecting the PDW supported by the fact that the newly produced platelets are larger than circulating platelets contributing to the increased PDW. They also tend to decrease in size with ageing in the circulation akine to the reticulocytes with increased mean volume [24]. As a result, in patients with TCP secondary to peripheral destruction the PDW is increased, reflecting active bone marrow compensation with release of young platelets [4].
Studies regarding the variation of platelet indices with the severity of TCP are sparse in literature. In the present study when platelet indices were correlated (MPV, PDW and PCT), there was statistically significant variation among the three groups. This reaffirms the concept stating that- The more severe the TCP, the more is the functioning of the compensatory mechanism of the body trying to increase the platelet content in the peripheral blood.
Limitation(s)
In most of the laboratories worldwide, platelet indices are measured in blood samples collected in EDTA. Factors affecting platelet count such as interference from cells or cell fragments, inadequate detection of large platelets or platelet clumps also influence platelet indices. Misinterpretation of the red blood cells as platelets results in an overestimation of MPV, PDW and increased large cell fraction. There is concern about anticoagulant for platelet counting, K2 or K3 EDTA, because it affects MPV. EDTA causes an increase in MPV from 7.9% within 30 minutes to 13.4% over 24 hours when measured by impedance and decreases by 10% when determined by an optical method. Type of analyser technology used, EDTA induced pseudo TCP, time from venipuncture to running the samples in analyser are also a few factors to be considered [12,25,26]. A good number of cases with severely low platelet count had to be excluded from present study as the analyser could not provide the indices.
Conclusion(s)
In the present era of automation, study of platelet indices can give a fair idea about the underlying mechanisms of TCP, thereby narrowing down the clinical differentials and avoiding the unnecessary ordering of further investigations. However, standardised measurement of the indices, a thorough knowledge of the indices interpretation and large scale studies may significantly increase the predictive power of platelet indices in confirming the aetiology of TCPs.
*Group A: Platelet count- <50000/cumm, Group B: Platelet count-50001-100000/cumm, Group C: Platelet count-100001-150000/cumm.
Group 1: Hyperdestructive, Group 2: Hypoproductive, Group 3: Abnormal pooling
**Significant p-value <0.05 MPV: Mean platelet volume; PCT: Plateletcrit; PDW: Platelet distribution width
Group A: Platelet count- <50000/cumm, Group B: Platelet count-50001-100000/cumm, Group C: Platelet count-100001-150000/cumm; **Significant p-value <0.05
MPV: Mean platelet volume; PCT: Plateletcrit; PDW: Platelet distribution width