Hysterectomy is one of the most commonly performed surgical procedure in women worldwide [1,2]. Minimally, invasive approach to hysterectomy has the advantage of shortened postoperative recovery time and hospitalisation time compared to open hysterectomy and the American Congress of Obstetricians and Gynaecologists recommend this approach whenever feasible [3]. In many developed countries, laparoscopic and robotic hysterectomy has replaced abdominal hysterectomy as the most common mode of hysterectomy [3,4].
Laparoscopic vaginal cuff suturing during TLH can be a challenging step and can contribute to increased operative time. Further, the Vaginal Cuff Dehiscence (VCD) rate may be higher after TLH compared to other modalities of hysterectomy [5]. Barbed sutures are now increasingly being used for vaginal cuff suturing during TLH. Several studies have reported that barbed sutures reduce the vaginal cuff closure time and the incidence of VCD when compared to traditional sutures [6,7]. Most of these studies have compared either unidirectional or bidirectional barbed sutures with traditional sutures. The aim of this study was to compare unidirectional and bidirectional sutures in vaginal cuff closure during TLH.
Materials and Methods
This was a Randomised Controlled Trial (RCT) done in the Department of Obstetrics and Gynaecology, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry and included women with benign uterine conditions scheduled to undergo TLH. The study enrollment was from November 2017 to March 2019. The study was approved (2017/0253) by the Institute Ethics Committee and was registered under Clinical Trials registry India (CTRI/2017/10/009976).
Patients with acute pelvic inflammatory disease, chronic cough or with any other condition that could increase the risk of infection or bleeding were excluded. Patients who agreed to be part of the study and gave informed consent were randomised into two groups for vaginal cuff closure: unidirectional barbed suture group or bidirectional barbed suture group. Block randomisation with varying block size; generated using computer was used to randomise the patients in the study arms, in the ratio of 1:1. Sealed, opaque envelopes were used for concealment and they were opened in the operation theatre by a resident. Patients were blinded to the suture type. All the surgeries were done by a single surgeon trained in advanced laparoscopic surgery.
Vaginal cuff closure was done using either unidirectional barbed suture (20 cm, No 0 polydioxanone, Quill VLP 1001, Angiotech Pharmaceuticals, Vancouver) or bidirectional barbed suture (7×7 cm, No 0 polydioxanone, Quill RX- 1068Q, Angiotech Pharmaceuticals, Vancouver) according to randomisation.
TLH was performed using four trocars: 1 umbilical (10 mm) and 3 lateral (5 mm) and with patients in the lithotomy position. Uterine manipulator was used for assistance. Laparoscopic bipolar forcep was used to coagulate vascular pedicles, and harmonic scalpel was used to perform the colpotomy. The uterus was retrieved through the vagina and vaginal cuff closure was done laparoscopically in a single layer without locking.
In unidirectional barbed suture group, the first suture was passed through a loop at one end of the vaginal cuff incorporating the utero-sacral ligaments. A continuous suture to the other end of vaginal cuff was performed and then the suture was cut. In case of bidirectional barbed suture group, the closure was started in the middle of the vaginal cuff and each needle was taken to the opposite end of vaginal cuff incorporating utero-sacral ligaments and the suture was cut.
Patients were followed-up in immediate postoperative period, after 2 weeks and 4 weeks postoperatively to assess vaginal cuff healing. Any infection, vaginal bleeding/spotting, pain were also noted. Per speculum examination was done to assess the vaginal cuff healing at 2 weeks and 4 weeks postoperatively. They were advised to refrain from intercourse for 6 weeks after surgery. Patients were contacted by telephone 6 months after surgery to inquire about any complications like vaginal bleeding, infection, readmission and dyspareunia.
Statistical Analysis
Based on the hospital data, the time difference for vaginal cuff closure was estimated between unidirectional barbed suture and bidirectional barbed suture to be 5 minute with SD at 6 minutes, α error of 0.05, with 95% CI and power of 80% with 1:1 ratio between the two study groups. The minimum sample size required to calculate difference in time in two groups was 23 patients in each group. The sample size was calculated using open Epi, Version3.
The distribution of data on categorical variables was expressed as frequency and percentage and their comparison between the groups were carried out by using Chi-square or fisher-exact test. The distribution of data on continuous variables was expressed as mean with SD or as median with range depending upon the normality of distribution. The normality of distribution of continuous data was assessed using Kolmogorov-Smirnov test. The comparison between the continuous variables was done with independent Students t-test or Mann-Whitney U Test. A p-value of <0.05 was considered as statistically significant. Statistical analysis was performed using IBM SPSS software version 21.0.
Results
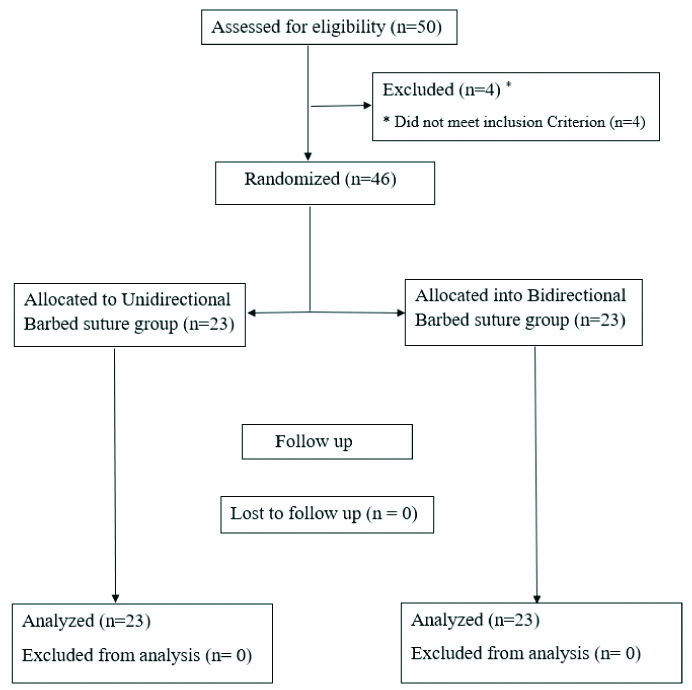
A total of 50 patients were assessed for eligibility, and 46 patients were included. All patients completed the trial. Twenty-three patients were randomised for vaginal cuff closure with unidirectional barbed suture and 23 patients for closure with bidirectional barbed sutures [Table/Fig-1].
Baseline demographics of patients are shown in [Table/Fig-2]. Uterine leiomyoma was the most common indication for surgery. [Table/Fig-3] shows the intraoperative variables and postoperative outcomes in both groups. There were no intraoperative complications noted in both groups. There was no significant difference in total operative time, blood loss and postoperative complications in between the two groups at 2 and 4 weeks’ follow-up. However, vault closure time in unidirectional group was found to be significantly less than in the bidirectional group. There were no cases of VCD in either groups.
Baseline patient characteristics.
| Parametres | Unidirectional barbed suture (n=23) | Bidirectional barbed suture (n=23) | p-value |
|---|
| Patient characteristics |
| Mean age, (years) (SD) | 43.39 (7.5) | 46.74 (5.9) | 0.1 |
| Mean body mass index, (kg/m2) (SD) | 25.6 (5.3) | 25.7 (5.4) | 0.98 |
| Post-menopausal | 3 (13) | 6 (26) | 0.46 |
| Prior laparotomy | 3 (13) | 4 (17.4) | 1 |
| Diabetes mellitus | 2 (8.7) | 4 (17.4) | 0.67 |
| Dyspareunia before hysterectomy | 6 (26) | 8 (34.8) | 0.75 |
| Presurgical diagnosis |
| Leiomyomas | 9 (39.1) | 11(47.8) | 0.55 |
| Abnormal uterine bleeding(P0 A0L0M0- C0O1E0I0N0)* | 2 (8.7) | 2 (8.7) | 1 |
| Adenomyosis | 9 (39.1) | 5 (21.7) | 0.2 |
| Endometriosis | 1 (4.3) | 4 (17.4) | 0.29 |
| Complex endometrial hyperplasia | 1 (4.3) | 1 (4.3) | 0.55 |
| Chronic pelvic pain | 1 (4.3) | 0 | 0.31 |
*Anovulatory dysfunctional uterine bleeding
Intraoperative and postoperative outcome.
| Surgical parametres | Unidirectional barbed suture (n=23) | Bidirectional barbed suture (n=23) | p-value |
|---|
| Mean Weight of the uterus (grams), mean (SD) | 372 (336.9) | 487 (381.8) | 0.29 |
| Length of surgery (min), mean (SD) | 139 (48.3) | 150.6 (42.7) | 0.39 |
| Time to close vaginal cuff (min), mean (SD) | 6.8 (1.6) | 11.3 (1.46) | <0.001 |
| Blood loss (mL), mean (SD) | 156.9 (101.6) | 139.78 (61.8) | 0.49 |
| 4-week postoperative findings |
| Vaginal bleeding n(%) | - | 2 (8.7) | 0.48 |
| Vault infection n(%) | 1 (4.3) | - | 0.31 |
At 6 months’ follow-up, none of patients reported vaginal bleeding, infection or re-admission in either groups. Only 19 (82.6%) patients in unidirectional group and 17 (73.9%) patients in bidirectional group had resumed sexual activity 6 months after surgery. Three patients (15.7%) in unidirectional group and 2 (11.7%) patients in bidirectional group reported dyspareunia. There was no significant difference in incidence of female dyspareunia in between the two groups (p=0.89). All these patients had reported dyspareunia preoperatively and there was no new onset dyspareunia reported by any patient. No case of male dyspareunia was reported in either groups.
Discussion
The mean time taken for vaginal cuff closure by unidirectional barbed suture group was 6.8±1.6 minutes and bidirectional barbed suture was 11.3±1.46 minutes (p <0.001). However, there was no significant difference in total operative time, blood loss and postoperative complications in between the two groups at 2- and 4-weeks’ follow-up. At 6 months follow-up, none of the patients had VCD or new onset dyspareunia.
Barbed sutures are a special type of monofilament absorbable sutures. They have cutting barbs on their surface and the orientation of these barbs is opposite to that of the needle. Unidirectional barbed sutures have a needle in one end and a loop in the other end whereas bidirectional barbed sutures has needles at both ends with barbs changing direction at the center of the suture [8]. There are several barbed sutures which are commercially available varying in length, suture material and size [9]. There are very few studies where these barbed sutures have been compared with each other [10,11].
In a retrospective analysis of vaginal cuff closure in 86 patients using unidirectional barbed suture, length of the suture was correlated with time for cuff closure [10]. They also reported 2 cases of VCD, both in patients where V-Loc 90 was used. A meta-analysis compared unidirectional and bidirectional barbed sutures with conventional sutures in different surgeries across all specialties [11]. They found that unidirectional barbed sutures decreased operative time when compared to conventional sutures but were associated with higher postoperative complications. On the other hand, bidirectional barbed sutures did not differ significantly from the conventional sutures both in terms of operative time and complications. But this meta-analysis of 17 RCTs had only 2 RCTs on TLH. This study is the first RCT directly comparing unidirectional and bidirectional barbed sutures during TLH.
Some retrospective studies on TLH have reported shorter total operative duration with barbed sutures compared to conventional sutures [12,13]. However, two recent RCTs comparing barbed suture and conventional sutures did not find any significant difference in total operative time [14,15]. In this study, there was no statistically significant difference in total operative time between unidirectional and bidirectional barbed sutures.
In a prospective comparative study comparing unidirectional barbed suture with conventional suture (polyglactin 910), vaginal cuff closure time in barbed suture group was reported to be significantly less than with conventional suture group (12.7±3.1 min vs. 20.4±7.1 min) [16]. A RCT comparing bidirectional barbed suture with conventional suture also reported significantly less vaginal cuff closure time with barbed suture [15]. However, another RCT comparing bidirectional barbed suture with conventional suture did not find any significant difference in vaginal cuff closure time between the two groups [14]. A meta-analysis on vaginal cuff suturing time reported that vaginal cuff closure time is reduced with the use of barbed suture compared to conventional suture [6]. In the index study, it was found that the vaginal cuff closure time was significantly more in bidirectional barbed suture group compared to unidirectional suture group. This could be because of the need to handle two needles instead of one in the bidirectional barbed suture group.
Usage of barbed sutures results in uniform tensile strength that is maintained evenly along the total length of vaginal cuff. Further, usage of barbed sutures results in better hemostasis and may reduce the usage of energy sources for hemostasis at vaginal cuff [17]. These factors may be responsible for reduced incidence of VCD with the usage of barbed sutures. In the present study, there were no cases of VCD.
Barbed sutures have cutting barbs on their surface and when used for vault closure may result in dyspareunia in patient or her partner [18]. In a RCT comparing bidirectional barbed suture with traditional suture during TLH, postoperative dyspareunia and sexual function were found to be similar in both groups [14]. However, they reported one case of male dyspareunia in the barbed suture group and were due to a loop of redundant barbed suture at vaginal apex.
Limitation(s)
There was no significant difference in dyspareunia between the two barbed suture groups, at 6 months postoperatively. However, this study was not powered to detect the differences in dyspareunia or VCD. Decreasing vault closure time by around 5 minutes in unidirectional barbed suture may not carry much significance if there are no postoperative complications in both groups. Longer follow-up period of at least 1 year would have been more appropriate to compare any vaginal dehiscence and degree of dyspareunia. Moreover, it was a single center study with a limited sample size.
Conclusion(s)
The vaginal cuff closure time during TLH using unidirectional barbed suture is significantly less when compared to bidirectional barbed suture. Larger prospective multicentric trials with longer follow-up period are needed to confirm the findings of the present study especially with respect to VCD and dyspareunia.
*Anovulatory dysfunctional uterine bleeding