Actinomycosis, once fairly common and often catastrophic, has now become an occasional infection in the era of antibiotics. The infection is caused by a branching Gram-positive, facultative anaerobic microorganism Actinomycetes. Various forms of the diseases in decreasing order of their frequency include cervico-facial form, abdomino-pelvic form and thoracic form. The thoracic involvement occurs in approximately 15% of all cases of actinomycosis. The disease presents with nonspecific signs and symptoms and therefore establishment of a definitive diagnosis with clinical and radiological investigations is difficult. The clinical and radiological picture mimics a number of other pulmonary conditions like cancer, tuberculosis, lung abscess and pneumonia. To reach at a definitive diagnosis one needs to have a high degree of suspicion and carry out histopathological studies in order to look for colonies of Actinomycetes as well as sulphur granules which are pathognomic for the infection. Here is a case of a 48-year-old diabetic male presenting with complaints of pain and swelling of neck, fever, dysphagia, dyspnea and cough with a mediastinal tumour like appearance on chest radiography. The patient underwent various noninvasive and invasive diagnostic modalities that included Contrast Enhanced Computed Tomography (CECT), Ultrasonography (USG) of thorax and histopathological examination of the cervical lymph nodes (level 2 and 3). The disease process was initially thought to be tubercular or malignant in origin which later turned out to be an actinomycotic lesion which was confirmed on the histopathological study of the lymph node specimen, that responded to antibiotics over a period of few months.
Antibiotics, Mediastinal malignancy, Tuberculosis
Case Report
A 48-year-old male presented to our Out Patient Department with chief complaints of pain and swelling on right side of neck, high grade fever, difficulty in swallowing, difficulty in breathing, cough with sputum and loss of appetite for 15 days. He was a known diabetic and hypertensive for three years on regular medication despite which he had poor glycaemic control. Patient also gave a history of left cervical lymph node abscess for which incision and drainage was performed two months back. He was a chronic tobacco chewer with poor dental hygiene but without any associated mucosal lesions and had history of dental caries for which he underwent dental extraction one and half months back.
General examination which included the vital signs, pallor, icterus, clubbing, cyanosis, oedema and jugular venous pressure were normal. The local examination revealed an ovoid, soft-to-firm, nonfluctuant, tender swelling with raised local temperature, measuring around 10×6 cm on the right side of the neck (cervical lymph node level 2 and 3). Respiratory system examination revealed a dull percussion note and decreased breath sounds in right parasternal, infraclavicular and mammary areas. After history taking and preliminary examination the differential diagnosis were lymphoma, tuberculosis, and cervical lymphadenopathy due to an unknown primary infection.
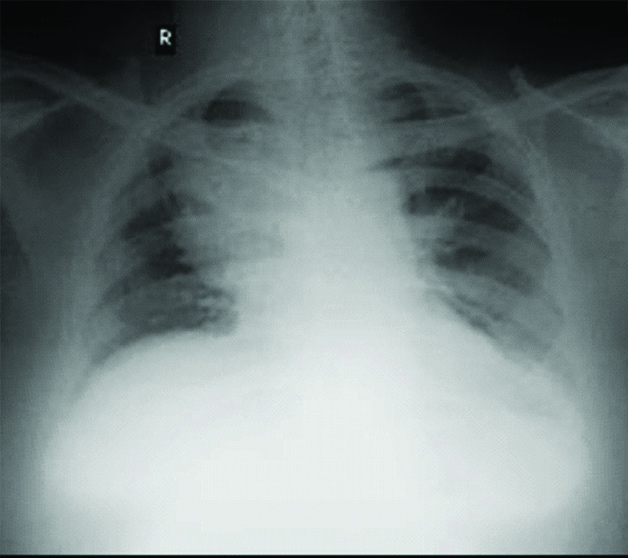
His chest X-ray obtained on admission revealed a well-defined, homogenous radiopacity in the right para-hilar region silhouetting the right heart border [Table/Fig-1].
Chest radiograph at the time of admission revealed a well-defined, homogenous radiopacity in the right para-hilar region silhouetting the right heart border indicating an anterior mediastinal mass lesion.
Routine blood tests revealed increase in leucocytes (WBC count=15600 cells/cumm) and Erythrocyte Sedimentation Rate (ESR=35 mm/hr) indicative of infective process. USG neck was done which was suggestive of neck abscess with reactive lymphadenopathy.
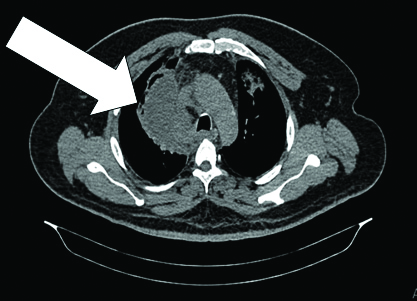
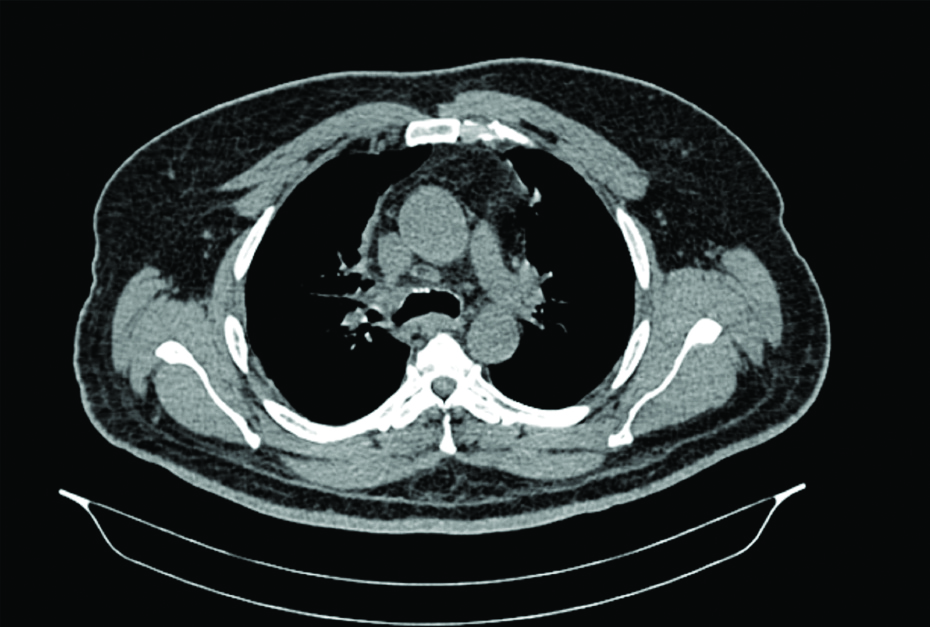
The CECT thorax revealed a well-defined multiloculated collection along the mediastinal pleura extending into the mediastinum with sub carinal, right paratracheal, right supraclavicular and right upper jugulodigastric lymphadenopathy possibly of infective aetiology [Table/Fig-2].
CT scan thorax at the time of admission revealed a well-defined multiloculated collection along the right mediastinal pleura extending into the mediastinum.
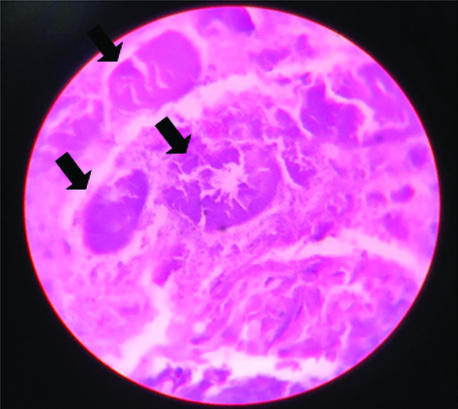
After completion of clinical and radiological examination the possibility of lymphoma or infective lymphadenopathy with suppuration was the differentials that were in the mind. Since the final diagnosis cannot be made without pathological or microbiological evidence, the differential still lay within the spectrum of malignancy and infection. The patient underwent incision and drainage of the neck abscess along with excisional biopsy of the cervical lymph nodes (level 2 and 3). The pus drained showed acute inflammatory pyogenic exudate with sulphur granules with no granuloma or malignant cells. Histopathology of cervical lymph node (level 2 and 3) revealed acute inflammatory exudates with colonies of Actinomycetes with peripheral staining and central clearing (rosette like configuration of the colonies) [Table/Fig-3].
Microscopic image of histopatholgical specimen of cervical lymph node stained with haematoxylin and eosin stain showing round to oval rosette like configuration of the colonies of actinomycetes (arrow) (H&E X100).
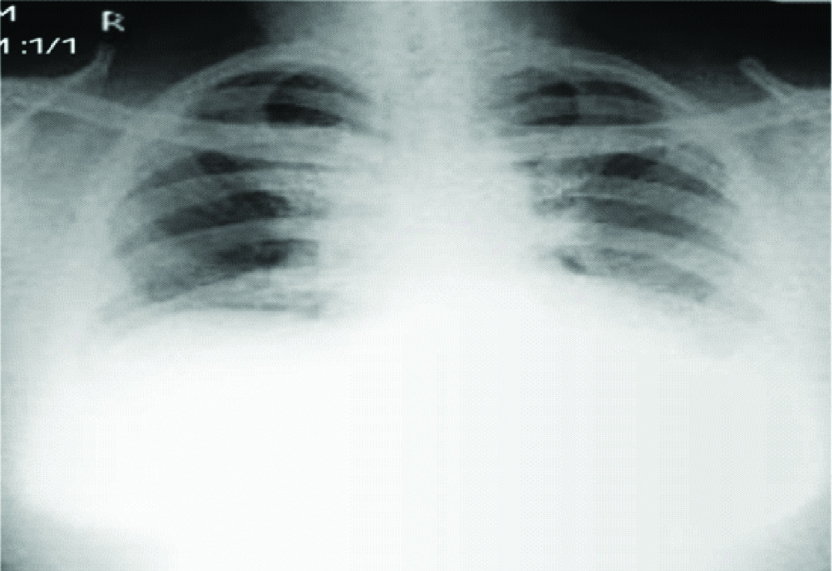
The patient was started on Injection Benzyl Penicillin which was given intravenously for 15 days and was discharged on oral penicillin preparation while ensuring strict glycaemic control. In response to this, there was significant symptomatic improvement along with radiological evidence of regression of the mediastinal shadow on X-ray as well as CT scan. Patient was advised for monthly follow up follow-up monthly and follow-up chest X-ray and CT scan thorax was done after the third month [Table/Fig-4,5].
Chest X-ray done after three months of treatment showing regression of the mediastinal lesion.
CT scan thorax done after three months of treatment showing complete resolution of the mediastinal lesion.
Discussion
Actinomycosis is a gradually progressive suppurative infection caused by Actinomyces spp., which are branching Gram-positive, facultative anaerobic, acid-fast negative bacilli, belonging to the normal flora of the oropharynx and gastrointestinal and urogenital tract [1]. The species that is mostly found in the pulmonary form of the disease is Actinomycetes israelii [2]. It is a rare infection occurring in one in 300,000 people per year [3]. Actinomyces israelii. mainly belongs to the human commensal flora of the urogenital tract, oropharynx and GIT. Actinomycosis, in any site imitates tuberculosis, nocardiosis because of its tendency to form cold abscess.
Pulmonary form of the disease is the third most common form after cervico-facial and abdomino-pelvic forms and constitutes one in seven patients of all cases of actinomycosis, however mediastinal involvement is far less described in literature. It is mainly due to trickling of upper gastrointestinal secretions into the airways or due to spread of cervicofacial infection/haematogenous spread [4]. Infection involving the mediastinum is extremely rare and literature regarding the same is scarce. The symptoms are nonspecific and this can occur due to the direct extension of cervico-facial lesion into the superior mediastinum, as it was seen in this case. Mediastinitis can also result from either perforation of the oesophagus (spontaneous or after instrumentation), penetrating chest trauma, complications of thoracic surgery, tracheobronchial perforation, or contiguous spread of pulmonary infection.
Risk factors for development of mediastinal actinomycosis include alcoholism, poor dental hygiene, pre-existing dental disease and underlying pulmonary diseases such as tuberculosis, COPD, bronchiectasis and aspergilloma [1]. Onset of this disease is insidious with nonspecific presenting complaints like cough with expectoration, chest pain, haemoptysis, anorexia and pyrexia. Involvement of mediastinal structures rarely results in Superior Vena Cava (SVC) syndrome, tracheoesophageal fistula, or pericarditis/myocarditis. Blood borne dissemination is a relatively common complication of the disease. Other less common complications include empyema thoracis, chronic sinusitis and haemoptysis. Low level of clinical suspicion can delay the diagnosis and worsen the prognosis and treatment outcomes [5].
The clinical and radiological picture mimics a number of other pulmonary conditions like cancer, tuberculosis, lung abscess and pneumonia. The radiologic manifestations of acute pulmonary actinomycosis have been described as air-space pneumonia without segmental distribution, located peripherally and with a predilection for lower lobes, whereas the radiologic signs of chronic thoracic actinomycosis include mass lesion, cavitation, chronic alveolar opacities, pleural involvement (empyema or pleural thickening), and chest wall involvement manifested by wavy periostitis of the ribs and/or mottled destruction of vertebral bodies.
The diagnosis of thoracic actinomycosis is based on histopathological testing of lung tissue specimens obtained by radiographically guided transthoracic needle biopsy, bronchoscopy guided, or resection by surgery. Sulphur granules are pathognomonic of actinomycosis [4,6-8]. The newer molecular methods, such as Polymerase Chain Reaction (PCR) with 16S rRNA gene sequencing and mass spectrometry, provide rapid microbiological confirmation of the disease with fair amount of accuracy [9].
The prognosis of the disease is excellent and an antibiotic treatment is generally curative. Intravenous penicillin at a dose of 18-24 million units daily for two to six weeks, followed by oral penicillin for 6-12 months, is the drug of choice. Surgical management should be considered when complications like massive haemoptysis and pleural empyema are present.
Conclusion(s)
Actinomycosis is a rare bacterial infection not frequently seen in routine practice and therefore the physicians have to be aware of typical clinical presentation and should also be able to distinguish it from processes like tuberculosis or neoplasm. Anaerobic bacterial culture and histopathology are cornerstone to arrive at a diagnosis following which prolonged penicillin therapy is the mainstay of treatment and surgery is considered in selected patients.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 06, 2019
Manual Googling: Jul 25, 2020
iThenticate Software: Aug 25, 2020 (15%)
[1]. Katsenos S, Galinos I, Styliara P, Galanopoulou N, Psathakis K, Primary bronchopulmonary actinomycosis masquerading as lung cancer: Apropos of two cases and literature reviewCase Rep Infect Dis 2015 2015:60963710.1155/2015/60963726146575 [Google Scholar] [CrossRef] [PubMed]
[2]. Endo S, Murayama F, Yamaguchi T, Yamamoto S, Otani S, Saito N, Surgical considerations for pulmonary actinomycosisAnn Thorac Surg 2002 74(1):185-90.10.1016/S0003-4975(02)03616-0 [Google Scholar] [CrossRef]
[3]. Han J, Lee K, Lee J, Kim Y, Choi S, Jeong Y, An overview of thoracic actinomycosis: CT featuresInsights Imaging 2012 4(2):245-52.10.1007/s13244-012-0205-923242581 [Google Scholar] [CrossRef] [PubMed]
[4]. Mabeza G, Macfarlane J, Pulmonary actinomycosisEur Respir J 2003 21(3):54510.1183/09031936.03.0008910312662015 [Google Scholar] [CrossRef] [PubMed]
[5]. Ferreira HP da C, Araújo CAA de, Cavalcanti JF, Miranda RLA de, Ramalho R de AO, Actinomicose pulmonar na forma pseudotumoral: Uma apresentaçäo raraJ Bras Pneumol 2011 37(5):689-93.10.1590/S1806-3713201100050001822042403 [Google Scholar] [CrossRef] [PubMed]
[6]. Wong VK, Turmezei TD, Weston VC, ActinomycosisBMJ 2011 343:d609910.1136/bmj.d609921990282 [Google Scholar] [CrossRef] [PubMed]
[7]. Valour F, Sénéchal A, Dupieux C, Karsenty J, Lustig S, Breton P, Actinomycosis: Etiology, clinical features, diagnosis, treatment, and managementInfect Drug Resist 2014 7:183-97.10.2147/IDR.S3960125045274 [Google Scholar] [CrossRef] [PubMed]
[8]. Ng LSY, Sim JHC, Eng LC, Menon S, Tan TY, Comparison of phenotypic methods and matrix-assisted laser desorption ionisation time-of-flight mass spectrometry for the identification of aero-tolerant Actinomyces spp. isolated from soft-tissue infectionsEur J Clin Microbiol Infect Dis 2012 31(8):1749-52.10.1007/s10096-011-1496-322143966 [Google Scholar] [CrossRef] [PubMed]
[9]. Veenakumari L, Sridevi C, Actinomycosis in histopathology- Review of literatureIAIM 2017 4(9):195-206. [Google Scholar]