Sarcoidosis is an inflammatory disease which leads to formation of noncaseating granuloma in the affected organs like lungs, lymph nodes and less commonly the skin. Cutaneous sarcoidosis occurs in about 20-35% of individuals with systemic sarcoidosis. Skin involvement serves as an early marker and may be the presenting sign of systemic sarcoidosis. Wide variety of morphological forms of cutaneous sarcoidosis is known to occur simulating several other dermatoses. Isolated skin involvement is very rare. Histopathological examination and special stains plays an important role in ruling out other granulomatous conditions like cutaneous tuberculosis, leprosy, foreign body granuloma and granuloma annulare from sarcoidosis. Corticosteroids remain the main cornerstone in the treatment of cutaneous sarcoidosis. Here, the authors reported two interesting cases of cutaneous sarcoidosis without systemic involvement, of which one presented as micropapular sarcoidosis and the other was mimicking lupus vulgaris. Both of them responded well to corticosteroid treatment and are in regular monitoring for development of systemic symptoms. Informed consent was obtained was obtained from both the patients.
Case 1
A 54-year-old female presented with asymptomatic generalised skin lesions over trunk and both upper limb for past ten days. Initially, started over upper back and spread to involve chest, abdomen and both upper limbs. There was no history suggestive of systemic involvement. General and systemic examinations were normal.
Cutaneous examination revealed multiple erythematous and skin coloured 1-2 mm papules distributed over the entire back, abdomen, both arms and forearms [Table/Fig-1].
Multiple tiny erythematous and skin coloured papules over forearm and abdomen.

Differential diagnosis of papular granuloma annulare, sarcoidosis, eruptive xanthoma, lichen nitidus, micropapular tuberculid and papular pityriasis rosea were considered.
Skin biopsy from a lesion in upper back revealed a classical noncaseating epithelioid cell granuloma (sarcoidal type) consisting of epitheloid cells, histiocytes, giant cells and sparse lymphocytes involving entire dermis. Stains for Acid Fast Bacilli and Wade fite were negative. Routine hematological and urine investigations were within normal limits. Serum Angiotensin Converting Enzyme (ACE) levels, calcium, liver function test, renal function test, fasting lipid profile, chest X-ray, pulmonary function test and ultrasound abdomen were normal. Mantoux test was negative. All these investigations pointed towards diagnosis of cutaneous sarcoidosis. Patient was started with oral and topical steroids and lesions gradually resolved. Currently, she is on hydroxychloroquine 200 mg/day.
Case 2
A 35-year-old male presented with two asymptomatic red raised skin lesions distributed over back and front of chest for past six months. There was no history suggestive of systemic involvement. General and systemic examinations were normal.
Cutaneous examination revealed a single erythematous plaque of size 0.7×0.7 cm diameter present over left upper chest in front of shoulder joint. Another erythematous plaque of size 3×2 cm with minimal scaling present over the right upper back [Table/Fig-2].
Erythematous plaque in left upper chest and right upper back.

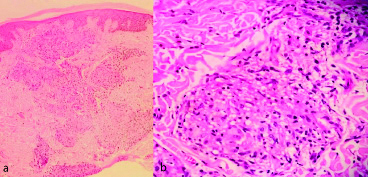
Differential diagnosis of lupus vulgaris and sarcoidosis were considered. Skin biopsy from a lesion in upper back was consistent with sarcoidosis revealing epidermis with irregular acanthosis, upper and deep dermis showed many epithelioid granulomas which were closely arranged with sparse lymphocytic cuffing [Table/Fig-3]. Stains for Acid fast bacilli and Wade fite were negative. Routine haematological and urine investigations were within normal limits. Serum ACE levels was high 225 U/L. Serum calcium, liver function test, renal function test, chest X-ray, pulmonary function test and ultrasound abdomen were normal. Mantoux test was negative. With these investigation reports, diagnosis of cutaneous sarcoidosis (plaque type) was made. Patient was treated with topical steroids and lesions gradually resolved.
a) Non-necritising epithelioid granuloma in the dermis with sparse lymphocytic cuffing (H&E-100); b) Noncaseating granuloma in dermis with focal collection of histiocytes, epitheloid cells and sparse lymphocytes (H&E-X 400). (Images from left to right)
Discussion
In 1889, first case of sarcoidosis was described by Besnier [1]. In India, the first case of cutaneous sarcoidosis was reported in 1957 by Rajam et al., Sarcoidosis is an immune mediated multisystem granulomatous disease of obscure aetiology with myriad of clinical features mainly affecting lungs, lymph nodes, eyes and skin. In the affected organs, noncaseating naked epithelioid cell granuloma occurs. It predominantly affects individuals in third and fourth decade with female predominance [2].
Sarcoidosis though a chronic inflammatory multisystem granulomatous disease, only cutaneous sarcoidosis occurs in about 10% of the patients. Cutaneous sarcoidosis can be classified as specific which reveals granuloma on biopsy and non-specific which is a reactive process without classical granuloma on histology [3].
Specific cutaneous sarcoidosis can occur in several morphological forms like papules, plaques, micropapules, lupus pernio, subcutaneous nodules (Darier-Roussy sarcoid), hypopigmented macules and alopecia (scarring and nonscarring) [4]. Other rare manifestations include erythroderma, morphea-form plaques, lichen nitidus like papules, leg ulcers, verrucous, folliculitis like, psoriasiform plaques and discoid lupus like plaques [5]. Most of them occur as asymptomatic lesions while pruritus occurs in 10-15% cases.
Among the several morphological forms papular type is the commonest, predominantly occurs on face. Micropapular cutaneous sarcoidosis is a rare variant of papular type with acute onset and favourable prognosis. It presents as tiny (1-2 mm) non-follicular shiny papules mainly distributed over trunk, limbs and periocular area. In this type, ocular and pulmonary involvement occurs frequently [6]. In the patient (case 1) by contrast face was not involved and there were no ocular or respiratory symptoms. The role of auto-immunity in sarcoidosis is a well-known fact and is characterised by increase in levels of CD4 Th1 helper cells and Th1cytokines [7]. Here in micropapular type, skin is even more compromised to allow rapid development of micropapular lesions. It has propensity for complete resolution without scarring and shows good response for a combination therapy with hydroxychloroquine and systemic steroids [6,8]. Hydroxychloroquine inhibits inflammation by blocking antigen processing and corticosteroid suppress the granuloma formation [9]. The patient also responded well to this combination treatment.
Distinction from other conditions like papular granuloma annulare, xanthoma, lichen nitidus and pityriasis rosea can be easily made based on histology. Distinction between micropapular tuberculid (lichen scrofulosorum) and micropapular cutaneous sarcoidosis is difficult both clinically and histologically. The following findings like: 1) nonfollicular papules; 2) absence of tuberculous foci; 3) negative Mantoux test; and 4) absence of caseating granuloma centered around hair follicle and or sweat ducts favour the diagnosis of sarcoidosis than lichen scrofulosorum [6,8].
More importantly in general differentiation of cutaneous sarcoidosis from lupus vulgaris is also challenging and occasionally impossible which the authors encountered in the case 2. There is no absolute criteria by which these two entities can be differentiated with certainity but following histopathological features help to distinguish: 1) infiltrate in sarcoid is scattered throughout the dermis, in lupus vulgaris its located closer to epidermis; 2) few lymphoid cells in periphery of granuloma as opposed to marked infiltrate around and between the granuloma in lupus vulgaris; 3) lack of central necrosis is common in sarcoid; 4) epidermis in sarcoidosis is mostly normal or atrophic whereas in lupus vulgaris in addition to atrophy, ulceration, acanthosis and pseudocarcinomatous hyperplasia are not uncommon [10,11].
In the patients, histopathology played a great role in arriving at a diagnosis. Presence of noncaseating epitheloid granuloma in dermis extending to subcutis with sparse lymphoctic infiltrate and absence of appendageal involvement pointed towards the diagnosis of sarcoidosis.
In about 30% of cases who initially had cutaneous sarcoidosis proceed to have systemic involvement in months to years. Hence, all cases presenting with cutaneous sarcoidosis must be screened for internal organ involvement with baseline work-up which includes history, clinical examination, CBC, RFT, LFT, serum ACE, calcium, ECG, chest radiography, PFT and ophthalmologic evaluation with regular follow-up [12]. All these investigation were done in both the patients and were normal (except for raised ACE levels in case 2). Both of them were in regular follow-up and monitored for onset of any new systemic symptoms.
Conclusion(s)
In India, sarcoidosis is uncommon and also wide spectrum of morphological forms of cutaneous sarcoidosis, causes diagnostic confusions. It is difficult to delineate it from cutaneous tuberculosis, granuloma annulare, lichen planus, leprosy, leishmaniasis, rosacea and several other dermatological disorders. Hence, sound knowledge and systematic work-up is essential for diagnosis.
[1]. Vashisht D, Sengupta P, Bansal N, Lupus pernioMed J Armed Forces India 2014 70:281-83.10.1016/j.mjafi.2012.05.00425378785 [Google Scholar] [CrossRef] [PubMed]
[2]. Reddy RR, Kumar BS, Harish MR, Cutaneous sarcoidosis-A great masquerader: A report of three interesting casesIndian Journal of Dermatology 2011 56:56810.4103/0019-5154.8715822121281 [Google Scholar] [CrossRef] [PubMed]
[3]. Ruocco E, Gambardella A, Langella GG, Lo Schiavo A, Ruocco V, Cutaneous sarcoidosis: An intriguing model of immune dysregulationInt J Dermatol 2015 54:01-12.10.1111/ijd.1256625312788 [Google Scholar] [CrossRef] [PubMed]
[4]. Mohanty R, Singh SN, Bhattamishra AB, Cutaneous sarcoidosis without systemic manifestationsIndian Journal of Dermatology 2009 54:8010.4103/0019-5154.45467 [Google Scholar] [CrossRef]
[5]. Fujii K, Okamoto H, Onuki M, Horio T, Recurrent follicular and lichenoid papules of sarcoidosisEur J Dermatol 2000 10:303-05. [Google Scholar]
[6]. Ridgway HA, Ryan TJ, Is micropapular sarcoidosis tuberculosis?JR Soc Med 1981 74:140-44.10.1177/0141076881074002107205849 [Google Scholar] [CrossRef] [PubMed]
[7]. Inaoka PT, Shono M, Kamada M, Espinoza JL, Host microbe interactions in the pathogenesis and clinical course of sarcoidosisJ Biomed Sci 2019 26:4510.1186/s12929-019-0537-631182092 [Google Scholar] [CrossRef] [PubMed]
[8]. Labadie JG, Florek AG, Vanden Boom T, Yazdan P, Krunic AL, Micropapular Cutaneous Sarcoidosis ReviewedDermatology (Basel) 2018 234:220-25.10.1159/00049312230278434 [Google Scholar] [CrossRef] [PubMed]
[9]. Jadotte YT, Hay RA, Salphale P, Mocellin S, Kumar S, Niazi A, Intervention of cutaneous sarcoidosisCochrane Database Syst Rev 2018 2018(8):CD01081710.1002/14651858.CD010817.pub2PMC6513262 [Google Scholar] [CrossRef] [PubMed]
[10]. Ko CJ, Glusac EJ, shapiro PE, Noninfectious granuloma. In: David E. Elder Elenitsas R editorsLever’s Histopathology of the skin 2009 10th editionNew DelhiLippincott Williams & Wilkins:371-372. [Google Scholar]
[11]. Sharath Kumar HK, Gayathri MN, Bharathi M, Ravikumar T, Isolated cutaneous sarcoidosis: A new insight into the old entityJ Clin Diagn Res 2013 7:1725-26. [Google Scholar]
[12]. Katta R, Cutaneous sarcoidosis: A dermatologic masqueraderAFP 2002 65:1581 [Google Scholar]