Left Planum Sphenoidale Transitional Meningioma- Simpson Grade-1
Jerrine Joseph1, C Emmanuel2, Arumugam Suresh3, Anand Parathasarthy4, Wilson Aruni5
1 Scientist D and Head, Department of Centre for Drug Discovery and Development, Sathyabama Institute of Science and Technology, Chennai, Tamil Nadu, India.
2 Director, Department of Academics and Research, Gleneagles Global Hospital and Health City, Chennai, Tamil Nadu, India.
3 Scientist cum Research Coordinator, Department of Central Research Laboratory, Meenakshi Academy of Higher Education, Kanchipuram, Tamil Nadu, India.
4 Medical Director and Chief Surgeon, Department of Ophthalmology, Centre for Vision and Eye Surgery, Chennai, Tamil Nadu, India.
5 Pro Vice Chancellor, School of Medicine, Loma Linda University, USA, Sathyabama Institute of Science and Technology, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Wilson Aruni, School of Medicine, Loma Linda University, USA, Sathyabama Institute of Science and Technology, Rajiv Gandhi Road (OMR), Chennai, Tamil Nadu, India.
E-mail: drwilsonaruni@hotmail.com
Planum sphenoidale meningiomas are rare slow growing tumours that impair cognition and lead to behavioural changes. Other common presentations of this condition include persistent headache followed by vision diminution. Dismissing cognitive impairment and behavioural changes as part of dementia, depression or aging might lead to loss of opportunity to treatment. The common symptoms manifested in sphenoid (spheno-orbital) wing meningioma is bulging of the eyes which may be painless, visual impairment and ocular paresis. Headache is also a common symptom, in addition to ptosis. Variants of the clinical syndrome include the following: Eye swelling and hearing loss, optic atropy, Kennedy syndrome and mental changes. Patient had severe headache for which he went for the eye checkup, where the loss of vision in the left eye was confirmed, through the field test. The MRI confirmed the tumour presence. Though the diagnosis was informed it took one year to convince the patient for the surgery. Hence, the author wishes to emphasise the role of tumour support systems. Physician’s serve as patients’ first point of entry into the health care system and as the continuing focal point for all necessary health care services along with their team they play a vital role in convincing patients from postdiagnosis to surgery and recovery.
Brain, Headache, Optic nerve, Routine check-up
Case Report
A 38-year-old lady reported to the Department of Ophthalmology with the chief complaint of visual disturbance. Patient gave a history of headache for more than one year. The patient had no other clinical complaints. There was no history of diabetes, hypertension or any other co-morbid conditions.
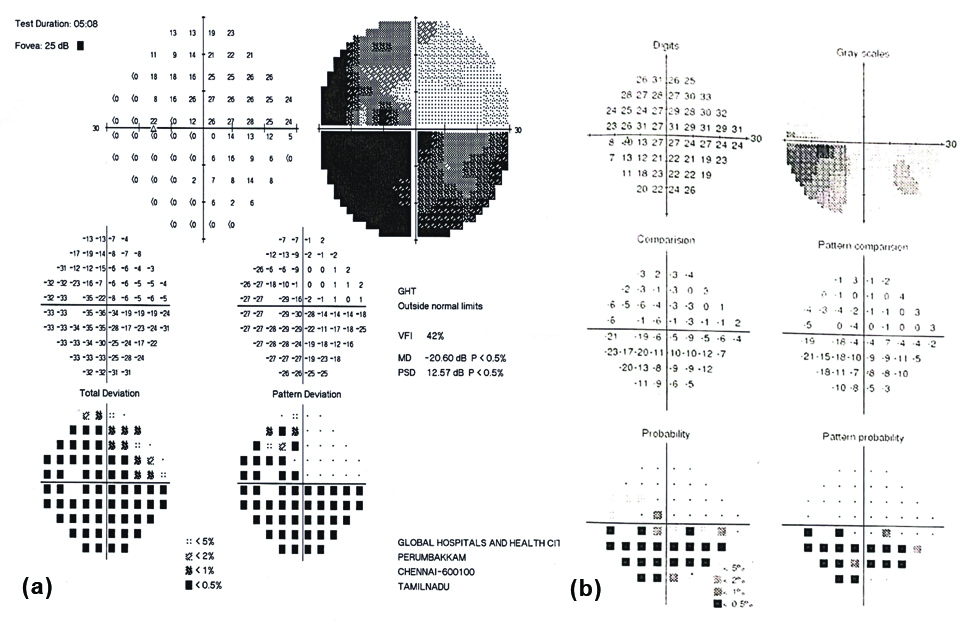
Patient experienced recurrent headaches, similar to migraine initially. Examination of the eye showed pallor of the optic nerve. Further, field tests were done revealing absence of dots in three out of four quadrants were. Hence, loss of vision was attributed in the left eye and Magnetic Resonance Imaging (MRI) was done as needed.
A contrast dye brain MRI was done which revealed a mass effect image in anterior clinoid process, the lesion encased and infero-laterally displaced the prechiasmatic portion of left optic nerve leading to its. Volume loss with T2W hyper intense signal in the intra-orbital and intra-canalicular segments of left optic nerve showed optic atrophy. The immediate plan of treatment suggested was open craniotomy. Due to complexity of the location and position of tumor along with associated risks, the patient denied the treatment.
Patient reported back after one year, since the headache and loss of vision seemed to get worse and no pain killers or alternative medicine like herbal treatment would help. At this juncture she was counselled by the Brain tumour support group and shared the experiences of previous patients’ testimonials. This gave her the needed confidence to undergo the surgery. Since it was over a year, the brain MRI had to be repeated to assess the current dimensions of the tumour before proceeding with the surgical procedure.
All laboratory results were within controlled range such as blood sugar, urea creatine, Liver Function Tests, Renal Function Tests; Thyroid Function Tests, routine blood profile etc., were in the permissible range. The repeat MRI revealed a well marginated, extra-axial lesion in left anterior clinioid process and planum sphenoidale. The mass was ISO intense to cortex on T1W and hyperintense on T2W and FLAIR images, with measurement of 3.1(AP)×2.2(T)×2.0(CC) cm [Table/Fig-1].
Axial 1 and TI of MRI images showing presence of: a) Planum Sphenoidale meningioma; b) Post- surgery.
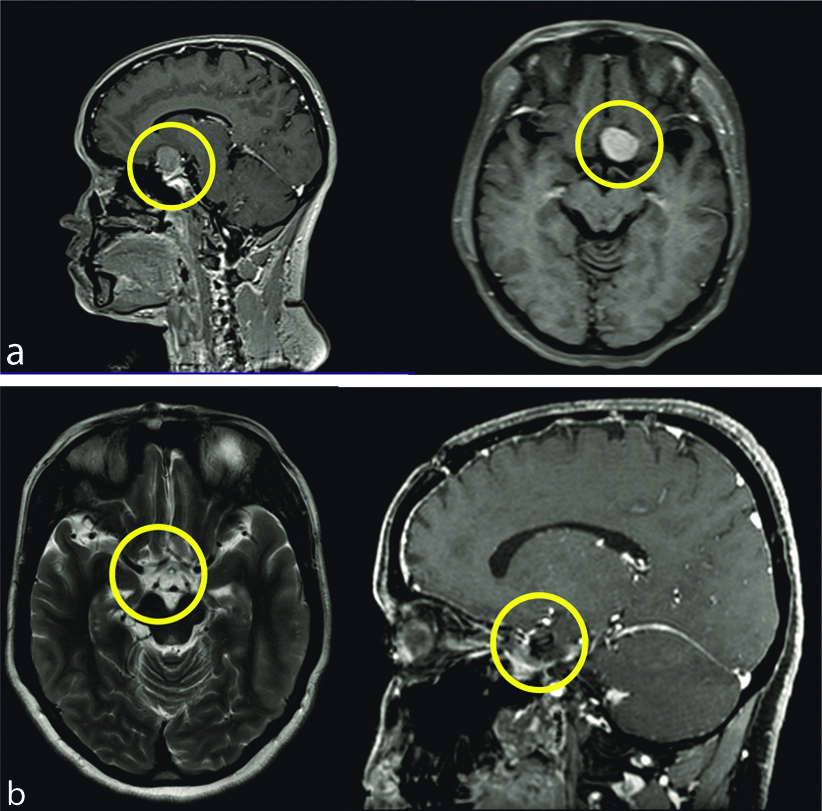
The patient underwent surgical intervention at the Neurosurgery Department. Patient consent was taken prior to the surgery and anaesthiologist consultation was also done, after explaining the procedure, such as bicoronal flap, left frontal craniotomy, sub-frontal approach and total excision of lesion with Visual Evoked Potential (VEP) monitoring. The tumour was excised in piecemeal using punch forceps after taking the specimen for histopathological examination to the pathology lab and was ascertained according to Simpson Grade-1. Post-tumour removal of both optic nerve, chiasma and pituitary stalk were well noticed.
Postsurgery, the patient recovered neurologically and improved well after two weeks of hospital stay. After one year, contrast MRI was taken and the field tests and visual test were also performed, the grey area in the lower quadrant of the left eye was found to be improved [Table/Fig-2]. The MRI taken after one year of follow-up, showed no residual mass/growth. The visual defect had been decreased as depicted in [Table/Fig-2] and the vision was also found to improve to 6/9 which was earlier 6/36 prior to surgery.
Patient’s visual field tests: a) Presurgical field test-Left eye; b) Postsurgical field test-left eye.
Discussion
Meningiomas comprise about 20% of intracranial tumours in adults, with female predominance among planum sphenoidale meningiomas is rare, constituting only 2% of all primary intracranial tumours [1-3]. Planum sphenoidale meningiomas are attributed to hormonal imbalance in female.
Supplanting of the olfactory tracts and optic chiasm takes place when the meningioma penetrates into the paranasal sinuses and nasal cavity [4]. Meningiomas extend anteriorly or posteriorly and across the midline from this primary site but the aetiology and manifestation of meningioma are ambiguous. They are slow growing and positioned in frontal lobes. Most often, at the time of diagnosis, these tumours have reached a large size even with mild presenting clinical signs. The patient usually presents with headache or visual symptoms. Difficulty with depth perception may result even though the patient may not have complete bilateral hemianopsia [5].
In the present case, fortunately, following the complete resection, the patient had visual recovery completely without any complications. The recurrence of meningiomas depends on the extent of resection and duration of follow-up. Valuation of consequences is an integral part of assessment of any form of therapy. Surgery remains the constitutional (and often only) procedure of treatment for brain tumours. With advances in imaging technology, many more tumours are being detected earlier at a stage when the patient may be neurologically well preserved and monitoring during surgery will navigate the outcomes effectively for vision perception. The conceivable benefits of surgery have to be considered against the potential risks involved. It is a unanimously accepted norm by neurosurgeons to follow the concept of ’safe maximal resection. As per previous reports the recurrence rate ranges from 5% to 41%. [6-9]. The occurrence of olfactory meningiomas is isolated cases where treatment has led to recovery. But the recovery rate of vision was not identical in the similar case studies of patients, which was monitored during and postsurgery [10].
Conclusion(s)
The index patient had completely recovered and returned to full time work. She was able carry out her daily chores efficiently and effectively. Hence, the Authors advocate for the early diagnosis and appropriate treatment of Planum sphenoidale meningiomas. The age of the patient plays a vital role in the speedy recovery of the patient postsurgery. It is important to emphasise that the family physician could always potentially provide awareness on the available options for treatment. Further, such a practice will confidently lead the patient to taking informed decisions explaining all types of interventional procedures. The brain tumour support group in hospitals will also play a vital role in enrolling the patients and their family into the treatment plan based on their success stories and live testimonies. Thus, it will all contribute to remove fear and impart confidence to cope with the life journey post meningioma diagnosis and postsurgery period. This enables the patients to handle the physical and emotional trauma better. Hence, an overall strong support system is very essential for a presurgery preparedness and postsurgery recovery.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Feb 14, 2020
Manual Googling: Jun 11, 2020
iThenticate Software: Aug 22, 2020 (11%)
[1]. Chiang GSH, Goh LG, Olfactory groove and planum sphenoidale meningiomaCan Fam Physician 2017 63(4):288-91. [Google Scholar]
[2]. Rachinger W, Grau S, Tonn JC, Different microsurgical approaches to meningiomas of the anterior cranial baseActa Neurochir (Wien) 2010 152:931-39.10.1007/s00701-010-0646-120383724 [Google Scholar] [CrossRef] [PubMed]
[3]. Tan JP, Li N, Gao J, Wang LN, Zhao YM, Yu BC, Optimal cutoff scores for dementia and mild cognitive impairment of the Montreal Cognitive Assessment among elderly and oldest-old Chinese populationJ Alzheimers Dis 2015 43(4):1403-12.10.3233/JAD-14127825147113 [Google Scholar] [CrossRef] [PubMed]
[4]. Somma A, Kaen AM, Valdepeñas CRE, Cavallo LM, Optic nerve atrophy due to long-standing compression by planum sphenoidale meningiomaWorld Neurosurg 2018 113:82-85.10.1016/j.wneu.2018.02.03229454120 [Google Scholar] [CrossRef] [PubMed]
[5]. Andrews BT, Wilson CB, Suprasellar meningiomas: The effect of tumour location on postoperative visual outcomeJ Neurosurg 1988 69(4):523-28.10.3171/jns.1988.69.4.05233418384 [Google Scholar] [CrossRef] [PubMed]
[6]. Atul G, Amresh B, Abhidha S, Amol K, Survendra R, Prahlad D, Olfactory groove meningiomas: An analysis based on surgical experience with 129 casesNeurology India 2018 66(4):1081-86.10.4103/0028-3886.23698930038098 [Google Scholar] [CrossRef] [PubMed]
[7]. Obeid F, Al-Mefty O, Recurrence of olfactory groove meningiomasNeurosurgery 2003 53(3):534-42.10.1227/01.NEU.0000079484.19821.4A12943570 [Google Scholar] [CrossRef] [PubMed]
[8]. Sanai N, Berger MS, Glioma extent of resection and its impact on patient outcomeNeurosurgery 2008 62:753-64.10.1227/01.neu.0000318159.21731.cf18496181 [Google Scholar] [CrossRef] [PubMed]
[9]. Kalkanis SN, Kondziolka D, Gaspar LE, Burri SH, Asher AL, Cobbs CS, The role of surgical resection in the management of newly diagnosed brain metastases: A systematic review and evidence-based clinical practice guidelineJ Neurooncol 2010 96:33-43.10.1007/s11060-009-0061-819960230 [Google Scholar] [CrossRef] [PubMed]
[10]. Moiyadi AV, Shetty PM, Perioperative outcomes following surgery for brain tumours: Objective assessment and risk factor evaluationJ Neurosci Rural Pract 2012 3(1):28-35.10.4103/0976-3147.9192722346187 [Google Scholar] [CrossRef] [PubMed]