Pelvic Congestion Syndrome Presenting with Massive Pulmonary Embolism
Mullusoge Mariappa Harsha1, Megha Sharma2, Ankit Kumar Sahu3
1 Assistant Professor, Department of Cardiology, Sri Jayadeva Insitute of Cardiovascular Sciences and Research, Mysore, Karnataka, India.
2 Assistant Professor, Department of Obstetrics and Gynaecology, SMS Medical College, Jaipur, Rajasthan, India.
3 Assistant Professor, Department of Cardiology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Mullusoge Mariappa Harsha, 329, 13th Main, 5th Cross, Saraswathipuram, Mysore, Karnataka, India.
E-mail: drharshamm@gmail.com
Pelvic Congestion Syndrome (PCS) causes chronic pelvic pain due to incompetent, dilated pelvic veins. Inferior Vena Cava (IVC) thrombosis can either be a cause or effect of PCS. Pulmonary embolism in such a setting is rare with only a few reported cases till date. A heightened awareness and clinical suspicion for the specific symptomatology and associated findings are necessary to prevent catastrophe. This report is about a rare case in a young multiparous female with overlooked chronic pelvic pain, due to PCS presenting with breathlessness and hypotension. On evaluation, her echocardiogram revealed dilated right sided chambers, large thrombus in IVC and right pulmonary artery. Troponin was elevated. Computed Tomography (CT) scan confirmed massive pulmonary embolism along with presence of dilated pelvic plexus and dilated right ovarian vein. Patient was successfully treated with systemic thrombolysis followed by oral anticoagulation.
Chronic pelvic pain, Dilated pelvic vein, Inferior vena cava thrombosis
Case Report
A 23-year-old female patient presented with history of non-cyclic low back/pelvic pain for last 6 months, low grade fever and intermittent vaginal discharge for last 1 month and dyspnea of New York Heart Association (NYHA) class IV for last 10 days [1]. There was no history of syncope or haemoptysis. There was no history of leg swelling suggestive of Deep Vein Thrombosis (DVT). She is G2P2L2 with last delivery 3 year back, not on oral contraceptives. She had multiple hospital visits elsewhere for last 6 months for low back/pelvic pain, with an ultrasound report done a month back revealing only an increased endometrial thickness.
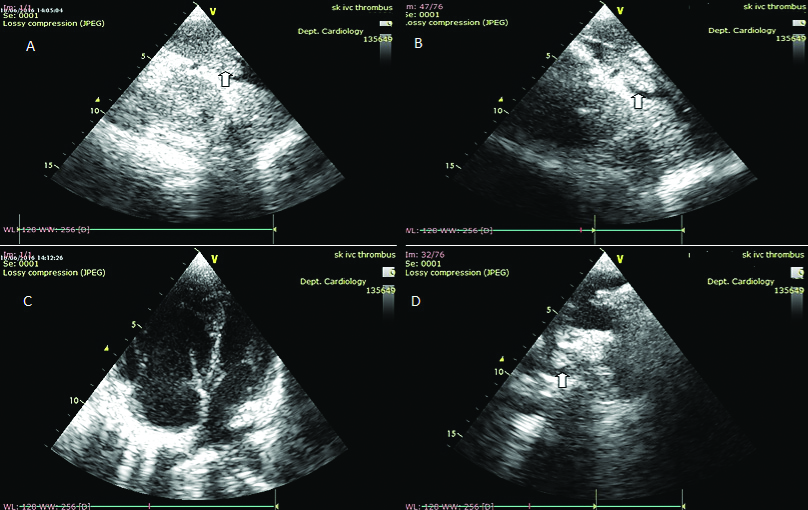
On examination, her pulse rate was 126/min, blood pressure 90/60 mmHg, tachypneic with respiratory rate of 28/min and room air oxygen saturation of 94%. There was an ejection systolic murmur in pulmonary area and loud P2; decreased breath sounds on right side and mild lower abdomen tenderness and cervical tenderness with no external varices. Echocardiography (ECG) was unremarkable except for sinus tachycardia and T inversion in V1-V4. Echocardiogram (Echo) revealed dilated right atrium and right ventricle, with right ventricular free wall hypokinesia and Right Ventricular Systolic Pressure (RVSP) of 64 mmHg. There was also a large thrombus in Inferior Vena Cava (IVC) and right pulmonary artery [Table/Fig-1A-D]. Her haemogram, Renal Function Test, Liver Function Test, thyroid profile and blood sugar were normal. Antinuclear Antibody was negative. Troponin was elevated.
Echocardiogram: A and B Free Floating Inferior Vena Cava (IVC) thrombus; C: Dilated right atrium and right ventricle suggesting massive pulmonary embolism; D: Thrombus in right pulmonary artery.
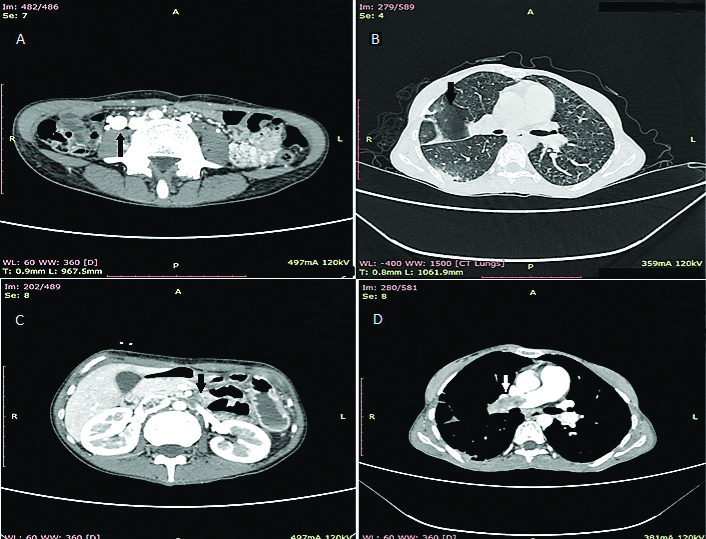
CT scan confirmed IVC thrombosis and Pulmonary Embolism occluding right pulmonary artery and peripheral thrombus in left pulmonary artery. Also, the right ovarian vein was dilated measuring 22 mm and adnexal veins were dilated, suggestive of PCS [Table/Fig 2A-D]. There was no evidence of lower extremity DVT on doppler study.
CT Scan: A-Dilated right ovarian vein and pelvic plexus; B: Pulmonary infarct; C: IVC thrombosis with left renal vein thrombosis; D: Right pulmonary artery thrombus
Patient was systemically thrombolysed with Streptokinase with 250,000 IU as a loading dose over 30 minutes, followed by 100,000 U/hr over 24 hours. Tachypnoea settled next day. Patient was anticoagulated with low molecular weight heparin with warfarin overlap to therapeutic International Normalised Ratio (INR). Follow-up ECHO on day 3 revealed no thrombus in IVC and in pulmonary artery with RVSP of 43 mmHg. A pro-coagulation assay did not reveal any abnormality.
At 3 months, patient was asymptomatic in NYHA class I [1] with INR of 2.6, echocardiogram showed normal size right atrium and right ventricle and a RVSP of 24 mmHg.
Discussion
PCS remains less diagnosed explanation for chronic pelvic pain usually in multiparous females. Symptoms include non-cyclical, lower back, pelvic and inner thigh pain, dyspareunia, and prolonged post-sexual discomfort [2]. There are only few reported cases of IVC thrombosis with pulmonary embolism in PCS. Tadlock MD et al., in post-mortem analysis of 500 deaths due to pulmonary embolism, showed pelvic plexus as source of pulmonary embolism in 4.2% [3]. Markovits MA et al., reported a case of recurrent pulmonary embolism from pelvic varices [4]. Isolated IVC thrombosis without lower limb DVT is rare, mostly attributed to IVC anomalies, malignancy or intra-abdominal pathologies [5]. Often it is difficult to distinguish PCS causing IVC thrombosis or vice-versa.
In the present case, lower abdominal symptoms were present for last 6 months with presence of hugely dilated right ovarian vein and pelvic varices with fresh mobile thrombus causing partial obstruction of IVC without affecting lower limb veins, PCS likely occurred first. Either ways, it can be fatal and an early diagnosis could prevent catastrophe of pulmonary embolism. PCS being an unusual diagnosis of exclusion in chronic pelvic pain, pelvic ultrasound and/or computed tomography scan are usually the first imaging modalities [6]. Often ultrasound being done by treating gynaecologist, it is important to look in particular venous anatomy with doppler study.
The present patient merited systemic thrombolysis in view of massive pulmonary embolism. The management dilemma was with IVC filter. In this patient with thrombus extending to right renal vein, an IVC filter if considered to be suprarenal with a Class IIb recommendation with Level of evidence C [7]. British Committee for Standards in Haematology state that vena cava filters have not been shown to reduce the incidence of fatal pulmonary embolism during thrombolysis (systemic or catheter-directed) and hence are not mandatory with such thrombolysis [8]. The present patient was administered systemic thrombolysis with streptokinase as per recommendation of ESC guidelines [9]. Patient was anti-coagulated with low molecular weight heparin, with overlap of vitamin K antagonist to attain therapeutic INR. Patient was followed up after 3 month which revealed normal pulmonary arterial pressures in NYHA Class 1 [1].
Conclusion(s)
Pelvic congestion syndrome is rare cause of pulmonary embolism and should be particularly looked for in multiparous female presenting with pulmonary embolism without extremity deep vein thrombosis.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 05, 2020
Manual Googling: Jun 23, 2020
iThenticate Software: Aug 16, 2020 (14%)
[1]. The Criteria Committee of the New York Heart AssociationNomenclature and Criteria for Diagnosis of Diseases of the Heart and Great Vessels 1994 9th edBoston, MassLittle, Brown & Co:253-56. [Google Scholar]
[2]. Janett DD, Lindsay M, Pelvic congestion syndromeSemin Intervent Radiol 2013 30(4):372-80.10.1055/s-0033-135973124436564 [Google Scholar] [CrossRef] [PubMed]
[3]. Tadlock MD, Chouliaras K, Kennedy M, Talving P, Okoye O, Aksoy H, The origin of fatal pulmonary emboli: a postmortem analysis of 500 deaths from pulmonary embolism in trauma, surgical, and medical patientsAm J Surg 2015 209(6):959-68.10.1016/j.amjsurg.2014.09.02725669120 [Google Scholar] [CrossRef] [PubMed]
[4]. Markovits MA, Wang JH, Shube SA, Recurrent pulmonary emboli from pelvic varices despite anticoagulation and infrarenal inferior vena cava filterJ Vasc Interv Radiol 2019 30(2):276-78.10.1016/j.jvir.2018.11.00430717968 [Google Scholar] [CrossRef] [PubMed]
[5]. McAree BJ, O’Donnell ME, Fitsmaurice GJ, Reid JA, Spence RA, Lee B, Inferior vena cava thrombosis: A review of current practiceVasc Med 2013 18(1):32-43.10.1177/1358863X1247196723439778 [Google Scholar] [CrossRef] [PubMed]
[6]. Elisabeth AI, Ruchika D, Shawn S, Amy SH, Douglas Y, Vivek M, Pelvic congestion syndrome: Diagnosis and treatmentSemin Intervent Radiol 2008 25(4):361-68.10.1055/s-0028-110299821326577 [Google Scholar] [CrossRef] [PubMed]
[7]. Jaff MR, McMurty MS, Archer AL, Cushman M, Goldenberg N, Goldhaber SS, Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertensionA scientific statement from the American Heart Association: Circulation 2011 123(16):1788-830.10.1161/CIR.0b013e318214914f21422387 [Google Scholar] [CrossRef] [PubMed]
[8]. British Committee for Standards in Haematology Writing groupBaglin TP, Brush J, Streif M, Guidelines on use of vena cava filtersBr J Haematol 2006 134:590-95.10.1111/j.1365-2141.2006.06226.x16869824 [Google Scholar] [CrossRef] [PubMed]
[9]. Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS)Eur Heart J 2020 41(4):543-603.10.1093/eurheartj/ehz40531504429 [Google Scholar] [CrossRef] [PubMed]