Primary Epitheloid Angiosarcoma (EA) of liver is an aggressive malignant tumour with poor prognosis irrespective of aggressive surgical resection with or without adjuvant therapy. It constitutes for 0.1-2% of primary malignant tumours of liver and is seen commonly in sixth or seventh decade of life, with male preponderance. It can be asymptomatic or may present with nonspecific symptoms. Lack of pathognomonic features on serological, biochemical and radiological tests, makes it even difficult for an early diagnosis. Despite early surgical removal, EA has very high recurrence rate. Chemotherapy agents (paclitaxel, bevacizumab) and immunomodulators (mTOR inhibitors) have shown some survival benefit and reduction in recurrence rates in recent years as adjuvant therapy. To the best of our knowledge, a hanging morphological variant of EA of liver has not been reported yet in literature. Author here by report a case of 37-years-old male incidentally diagnosed with aggressive, hanging variant of EA of liver. Despite early surgical resection and adjuvant, after chemotherapy patient had survival of less than eight months since first presentation.
Case Report
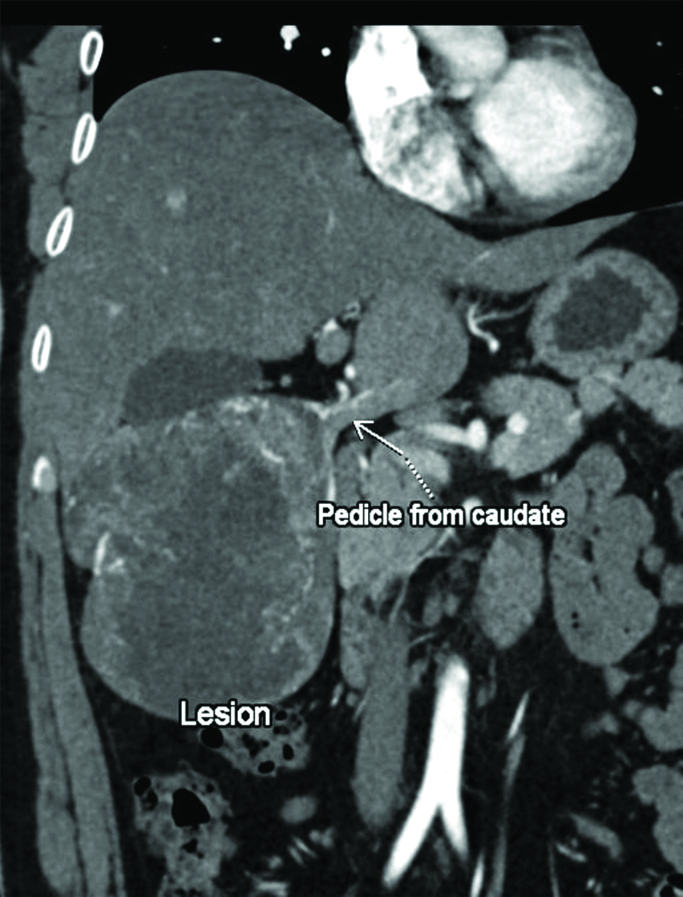
A 37-year-old male patient was referred to Hepato-billiary surgery department with chief complaints of vague abdominal pain, anorexia and weight loss since two months. There was no significant past medical or family history or any occupational exposure to chemicals. Clinical examination was unremarkable. Ultrasound report showed hepatomegaly with a single, well defined, heterogeneous, hypoechoic lesion. His clinical examination and Liver Function Tests (LFTs) were normal. Tumour markers were normal, CA19-9-9 U/mL, AFP-1.8 ng/mL, CEA-2.61 ng/mL. Computed Tomography (CT scan) showed a 10.4×9.1×11.4 cm, well defined, heterogeneously hypodense lesion in subhepatic region, free from surrounding structures except a peduncular stalk from caudate lobe [Table/Fig-1]. On contrast imaging, it showed arterial enhancement with no venous/portal washout, delayed and equilibrium phases showed progressive enhancement with central necrosis with no internal haemorrhage, calcification, and vascular invasion. It received blood supply primarily from branches of left hepatic artery. Rest of scan was unremarkable. Provisional differential diagnoses on imaging were Hepatocellular Carcinoma and Atypical Angiosarcoma. Fluorodeoxy glucose Positron emission tomography did not reveal any extra hepatic spread. Needle aspiration or biopsy was not performed to avoid risk of tumour seeding and bleeding. After discussing in multidisciplinary team, surgical excision was performed with R0 resection. A well circumscribed, capsulated, smooth, pinkish tumour was seen hanging from caudate with small pedicle [Table/Fig-2]. Cut surface was grayish white with multiple haemorrhages, gelatinous areas, and cystic spaces [Table/Fig-3].
Preoperative CT showing hanging liver mass with a caudate pedicle.
Smooth, well circumscribed surgical specimen after R0 resection.

Cut surface showing grayish white, haemorrhagic and gelatinous areas.

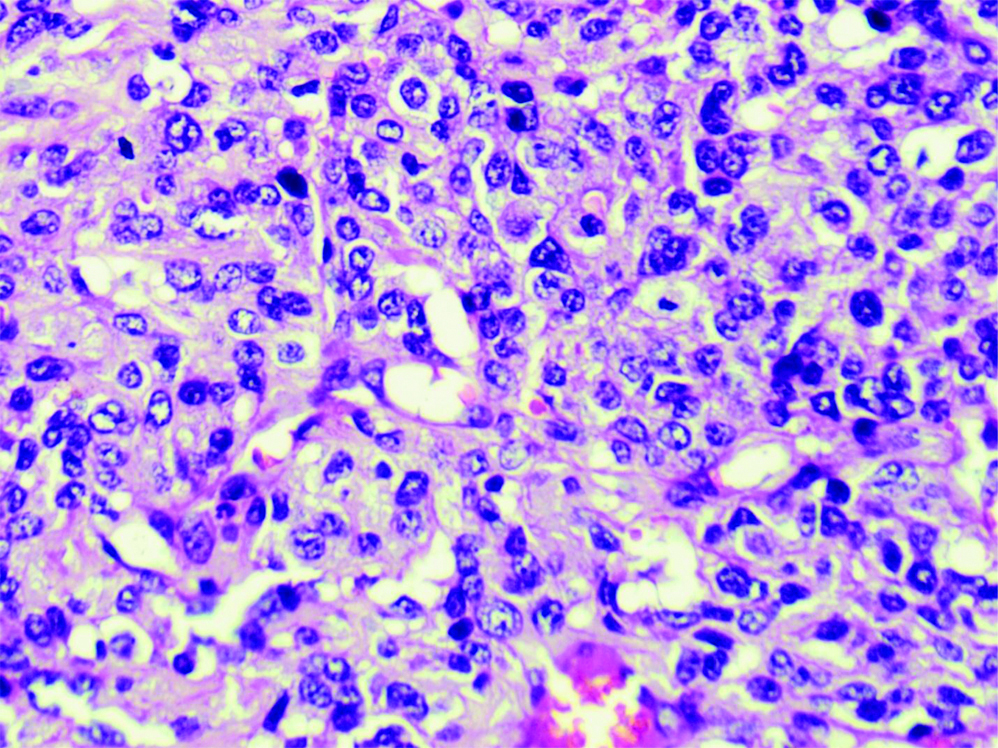
On microscopic examination, oval to spindle cells were seen arranged in sheets, fascicles with marked anisonucleosis and brisk mitosis in areas of necrosis [Table/Fig-4,5]. Intervening stroma was collagenous with no normal liver parenchyma. These features were suggestive of Hepatic Angiosarcoma. On Immunohistochemistry (IHC), Tumour expressed CD-34, Fli-1, D240 in diffuse and intense manner, typical of EA. It was negative for cytokeratin, S-100, synaptophysin, Glypican3, CD-31, DOG.1 and CD-117/c- kit.
Histopathological examination sections of surgical specimen showing oval and spindle cells arranged in sheets and fascicles with Intervening collagenous stroma is noted. (H&E, X100).
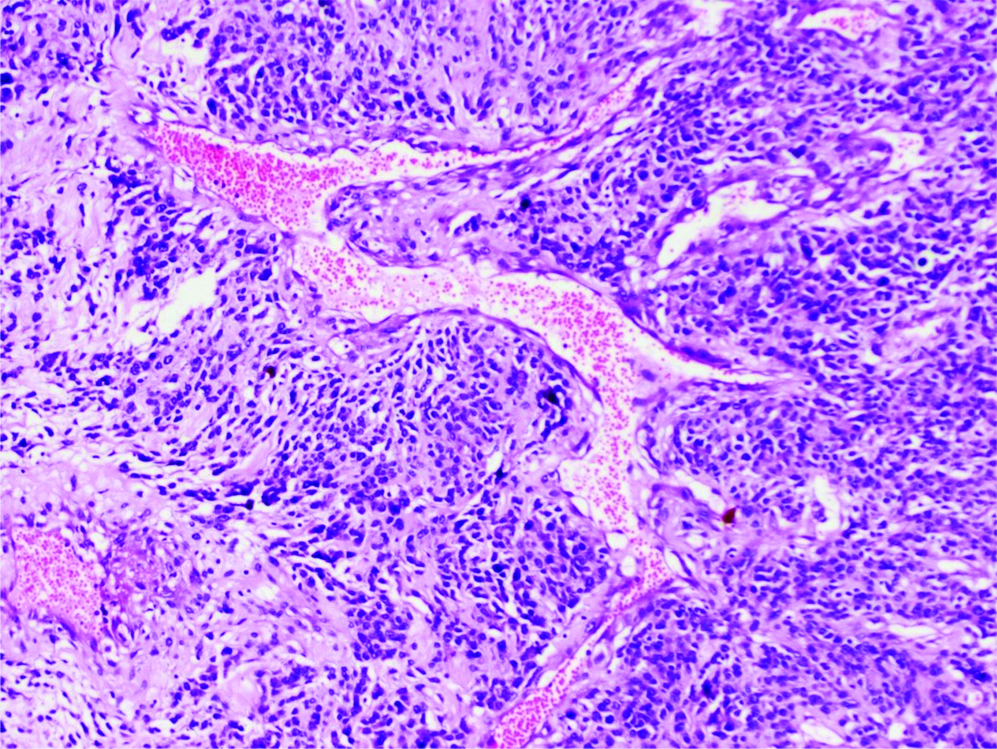
Histopathological examination sections of surgical specimen showing areas of anisonucleosis, mitosis. (H&E, X400).
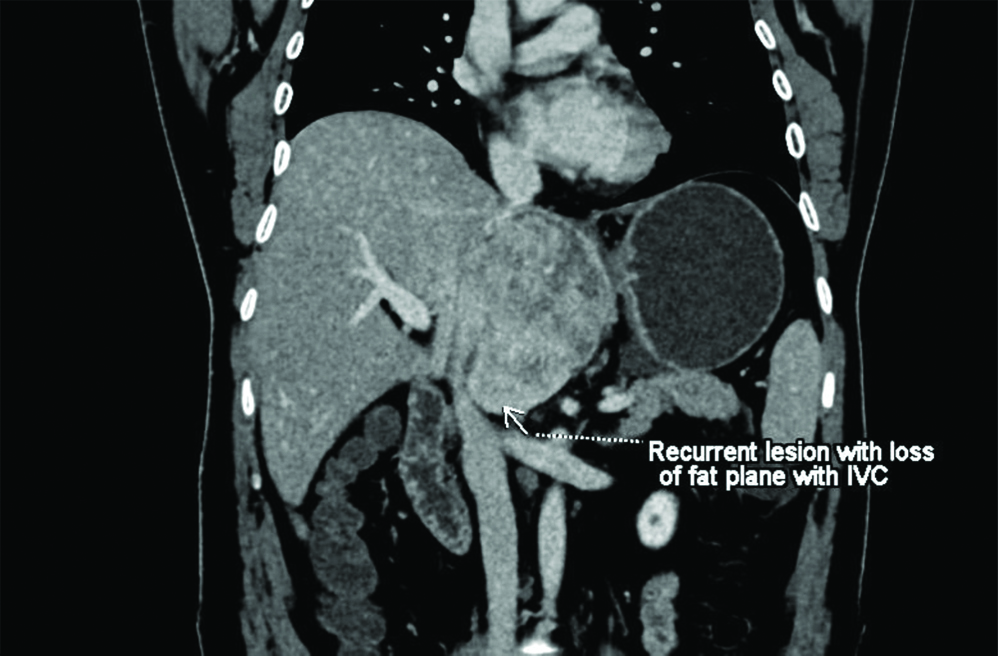
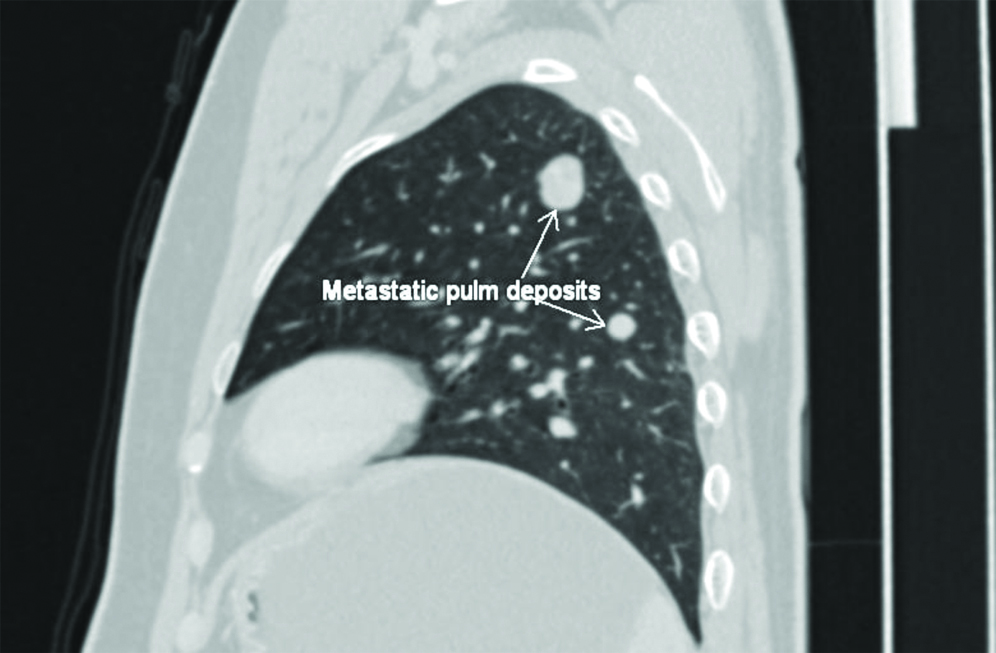
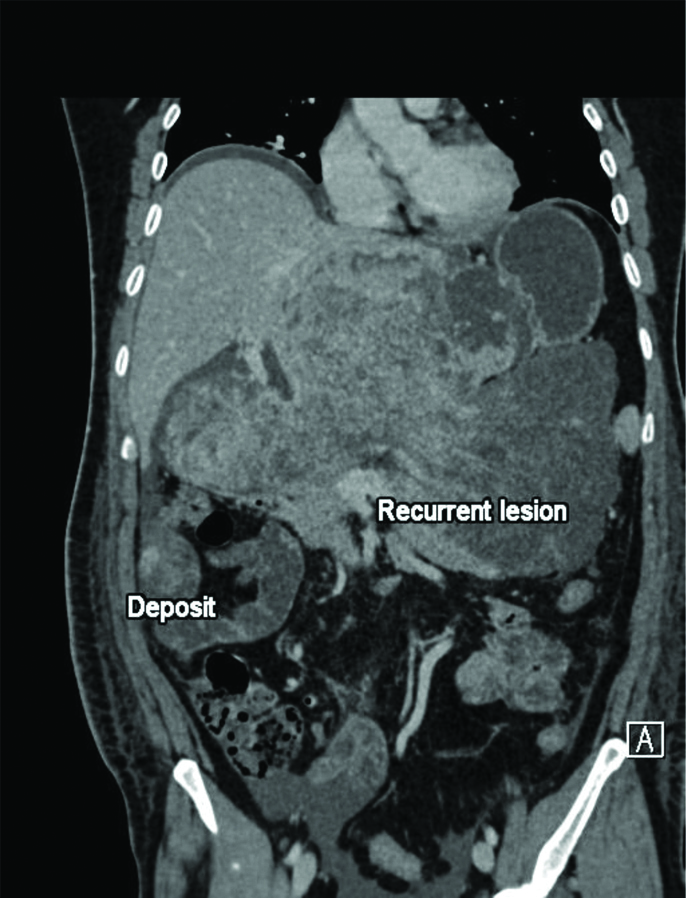
Postoperative course was uneventful. Follow-up PET done after four weeks showed no abnormal uptake. He was started on weekly Paclitaxel based chemotherapy. The CT done at four months (after eight cycles of chemotherapy), showed recurrence of abdominal mass with multiple lung deposits [Table/Fig-6,7]. Gemcitabine and Docetaxel were added in chemotherapy, but successive imaging showed progressive disease [Table/Fig-8]. Patient succumbed to disease within eight months of diagnosis.
Postoperative CT (four months) showing recurrence of abdominal lesion.
Postoperative High-Resolution Computed Tomography (HRCT) showing metastatic pulmonary lesions.
Postoperative CT (six months) disease progression after modified chemotherapy.
Discussion
Angiosarcoma is a non epithelial, malignant mesenchymal tumour with vascular endothelial differentiation and aggressive proliferation, accounting for less than 1% of all soft tissue sarcomas [1]. Angiosarcomas can be cutaneous, deep soft tissue or visceral, common sites are head, face and neck; but sites like breast, spleen and bones have also been reported [2]. Hepatic Angiosarcomas represent 0.1-2% of all primary tumours of the liver, seen in sixth and seventh decade with male preponderance [3].
The EA is a subtype of angiosarcoma, where malignant cells have predominantly epithelioid appearance, with very few cases reported in literature. EA is commonly seen in deep soft tissues of extremities, but less commonly also in thyroid and adrenals [4]. The site of origin may have a correlation with the amount of lymphovascular supply and endothelial cells in the organ [5]. Aetiology of EA is unknown in most cases (75%). Few cases are related to environmental exposure to agents like, vinyl chloride, arsenic, anabolic steroids, cyclophosphamide, and thorium dioxide; while there are reports of correlation of EA with haemochromatosis and von Recklinghausen disease [6]. However, no such association was seen in our case.
The EA may present in a variety of ways, from completely asymptomatic (~12.5%), to nonspecific symptoms (abdominal discomfort, fatigue, anorexia, weight loss) to widely disseminated disease (~9%) with rapid deterioration [3]. Acute liver failure, Kasabach-Merritt syndrome, high output cardiac failure, tumour rupture causing haemothorax, haemoperitoneum are also been reported as presentations [7,8]. Biochemical and serological tests usually are of little use for diagnosis. Liver enzymes show nonspecific rise in most cases. Hyperbilirubinemia, thrombocytopenia, leucocytosis, anaemia and hypercalcaemia also have been mentioned [9]. Tumour markers like alfa-feto protein, carcinoembryonic antigen, cancer antigen 19-9 may show mild elevation [10].
Radiologically, it is difficult to differentiate EA from other masses due to hypervascularity and lack of definitive features. There is no specific radiological diagnostic criterion mentioned in literature. Ultrasonography may show solitary or multiple mass lesions with variable echogenicity. There are few features mentioned for liver angiosarcomas of liver on CT or MRI. There is early arterial enhancement with progressive contrast filling without washout, with variable post contrast enhancement patterns within and around the lesion [11]. Angiosarcomas are Fluorodeoxyglucose Positron Emission Tomography (FDG-PET) avid, aiding in detection of metastases [12].
Lack of other definitive diagnostic tools makes role of pathology and tissue markers very crucial. Macroscopically, liver EA usually present as single parenchymal mass with satellite nodules or as diffuse infiltrative lesions, due to atypical endothelial proliferation in sinusoids [13]. But hanging morphology of liver EA has not been reported in literature yet. There is no morphological classification of liver EA described. But most cases reported till date are intra parenchymal masses, making pedunculated tumour a rare morphological variant.
Microscopic features are heterogeneous and may show overlap with features of metastatic carcinoma, cholangiocarcinoma, metastatic sarcoma with epithelioid morphology, malignant melanoma and epithelioid hemangioendothelioma. EA consists of large, mildly to moderately pleomorphic, round to polygonal epithelioid cells with abundant eosinophilic cytoplasm. Most cells are arranged in sheets, but cellular islands or cords may be seen [14,15].
The IHC provides the most accurate diagnosis. Expression of endothelial markers CD31, CD34, FLI1, ERG and factor VII-RA is characteristic of EA [16,17]. CD31 is the single best marker, particularly, if Factor VIII-RA is negative. CK (cytokeratin), Ki67, CAM5.2, Vimentin, EMA, and FOS-B may show partial positivity, while c-Myc, CAMTA-1, and TFE-3 are usually negative.
The EA has poor prognosis, high recurrence rates and survival no longer than 12 months [17,18]. The prognosis depends on the site, size (>5 cm), stage, pleomorphism, cellularity, mitotic activity, proliferative index and bleeding.
Surgical resection, radiation and chemotherapy are the treatment modalities [19]. Liver directed trans-catheter therapy is useful in unresectable tumours and as an emergency procedure in tumour rupture [20]. Paclitaxel-based chemotherapy may improve survival (five months median duration of response) with a response rate of 89% [21]. However, despite paclitaxel based chemotherapy our patient showed progression of disease. Combined use radiation and bevacizumab, followed by surgery has shown some remission response [20]. Everolimus (5-10 mg/day) has also shown some benefits in recurrent/metastatic EA [22]. Up to 2013, angiosarcomas of liver were considered an absolute containdication for Liver Transplantation (LT) due to poor survival and high recurrence. In 2014, 27 months no recurrence period was seen after a paediatric LT, where sirolimus was used [23]. A survival over two years (32-69 months) is reported in retrospective series in Taiwan (2015) with early surgery and chemotherapy [24]. However, further studies are required to define survival benefit and the role of LT and surgery with newer chemotherapeutic agents in cases of Hepatic Angiosarcomas.
Conclusion(s)
Hepatic EA have limited literature available as far as morphological classification is concerned. Larger studies are required to determine if different macroscopic morphological patterns have any correlation with disease prognosis. On other hand, liver EA are difficult to diagnose early and have poor prognosis. Despite early R0 resection and adjuvant therapy patient continue to have dismal survival rates. Recent studies have shown some good results with newer adjuvant chemotherapeutic agents. We need larger studies to determine efficacy of these agents in hepatic EA.
[1]. Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ, AngiosarcomaLancet Oncol 2010 11:983-91.10.1016/S1470-2045(10)70023-1 [Google Scholar] [CrossRef]
[2]. Deshpande V, Rosenberg AE, O’Connell JX, Nielsen GP, Epithelioid angiosarcoma of the bone: A series of 10 casesAm J Surg Pathol 2003 27:709-16.10.1097/00000478-200306000-0000112766574 [Google Scholar] [CrossRef] [PubMed]
[3]. Chaudhary P, Bhadana U, Singh RA, Ahuja A, Primary hepatic angiosarcomaEur J Surg Oncol 2015 9:1137-43.10.1016/j.ejso.2015.04.02226008857 [Google Scholar] [CrossRef] [PubMed]
[4]. VandenBussche CJ, Wakely PE Jr, Siddiqui MT, Maleki Z, Ali SZ, Cytopathologic characteristics of epithelioid vascular malignanciesActa Cytol 2014 58:356-66.10.1159/00036615125195738 [Google Scholar] [CrossRef] [PubMed]
[5]. Hart J, Mandavilli S, Epithelioid angiosarcoma: A brief diagnostic review and differential diagnosisArch Pathol Lab Med 2011 135:268-72.10.5858/135.2.26821284449 [Google Scholar] [CrossRef] [PubMed]
[6]. Huang NC, Wann SR, Chang HT, Lin SL, Wang JS, Guo HR, Arsenic, vinyl chloride, viral hepatitis, and hepatic angiosarcoma: A hospital-based study and review of literature in TaiwanBMC Gastroenterol 2011 11:14210.1186/1471-230X-11-14222200164 [Google Scholar] [CrossRef] [PubMed]
[7]. Ito Z, Kajihara M, Kobayashi Y, Kanai T, Matsumoto Y, Takakura K, Hepatic angiosarcoma associated with esophageal variceal hemorrhageCase Rep Gastroenterol 2016 10(2):440-45.10.1159/00044806727721730 [Google Scholar] [CrossRef] [PubMed]
[8]. Heo SH, Jeong YY, Shin SS, Chung TW, Kang HK, Solitary small hepatic angiosarcoma: Initial and follow-up imaging findingsKorean J Radiol 2007 8(2):180-83.10.3348/kjr.2007.8.2.18017420638 [Google Scholar] [CrossRef] [PubMed]
[9]. Locker GY, Doroshow JH, Zwelling LA, Chabner BA, The clinical features of hepatic angiosarcoma: A report of four cases and a review of the English literatureMedicine (Baltimore) 1979 58(1):48-64.10.1097/00005792-197901000-00003368508 [Google Scholar] [CrossRef] [PubMed]
[10]. Huerta-Orozco LD, Leonher-Ruezga KL, Ramírez-González LR, Hermosillo-Sandoval JM, Sandoval-Alvarado JJ, Morán-Galaviz RE, Hepatic angiosarcoma and liver transplantation: Case report and literature reviewCir Cir 2015 83(6):510-15.10.1016/j.circen.2015.11.01626144270 [Google Scholar] [CrossRef] [PubMed]
[11]. Park YS, Kim JH, Kim KW, Lee IS, Yoon HK, Ko GY, Primary hepatic angiosarcoma: Imaging findings and palliative treatment with transcatheter arterial chemoembolization or embolisationClin Radiol 2009 64(8):779-85.10.1016/j.crad.2009.02.01919589416 [Google Scholar] [CrossRef] [PubMed]
[12]. Tetsuo M, Ukihide T, Tadashi H, Hidenori O, Yasuaki A, Kazuro S, Case report: Primary hepatic angiosarcoma on coregistered FDG PET and CT imagesAJR 2007 188:1615-17.10.2214/AJR.05.083017515384 [Google Scholar] [CrossRef] [PubMed]
[13]. Washington K, Masses of the liver. In SE Mills, D Carter, JK Greenson, HA Oberman, V Reuter, MH Stoler EdsSternberg’s Diagnostic Surgical Pathology 2004 Vol 2PhiladelphiaLippincott Williams & Wilkins:1705-24. [Google Scholar]
[14]. Klijanienko J, Caillaud JM, Lagace R, Vielh P, Cytohistologic correlations in angiosarcoma including classic and epithelioid variants: Institut Curie’s experienceDiagn Cytopathol 2003 29:140-45.10.1002/dc.1033512951681 [Google Scholar] [CrossRef] [PubMed]
[15]. Jeon YK, Kim HW, Choi HJ, Park IA, Fine needle aspiration cytology of epithelioid angiosarcoma: Report of a case with nuclear grooves and indentationsActa Cytol 2004 48:223-28.10.1159/00032632115085757 [Google Scholar] [CrossRef] [PubMed]
[16]. Wu J, Li X, Liu X, Epithelioid angiosarcoma: A clinicopathological study of 16 Chinese casesInt J Clin Exp Pathol 2015 8:3901-09. [Google Scholar]
[17]. Sundaram M, Vetrichevvel TP, Subramanyam S, Subramaniam A, Primary multicentric cutaneous epithelioid angiosarcomaIndian J Dermatol Venereol Leprol 2011 77:11110.4103/0378-6323.7499021220905 [Google Scholar] [CrossRef] [PubMed]
[18]. Zheng YW, Zhang XW, Zhang JL, Hui ZZ, Du WJ, Li RM, Primary hepatic angiosarcoma and potential treatment optionsJ Gastroenterol Hepatol 2014 29:906-11.10.1111/jgh.1250624372769 [Google Scholar] [CrossRef] [PubMed]
[19]. Ravi V, Patel S, Vascular sarcomasCurr Oncol Rep 2013 15:347-55.10.1007/s11912-013-0328-223852636 [Google Scholar] [CrossRef] [PubMed]
[20]. Pierce DB, Johnson GE, Monroe E, Loggers ET, Jones RL, Pollack SM, Safety and efficacy outcomes of embolization in hepatic sarcomasAJR Am J Roentgenol 2018 210:175-82.10.2214/AJR.16.1757329090997 [Google Scholar] [CrossRef] [PubMed]
[21]. Fata F, O’Reilly E, Ilson D, Pfister D, Leffel D, Kelsen DP, Paclitaxel in the treatment of patients with angiosarcoma of the scalp or faceCancer 1999 86:2034-37.10.1002/(SICI)1097-0142(19991115)86:10<2034::AID-CNCR21>3.0.CO;2-P [Google Scholar] [CrossRef]
[22]. Zhang SL, Liang L, Ji Y, Wang ZM, Zhou YH, The benefit of everolimus in recurrent/epithelioid angiosarcoma patients: Case reports and literature reviewOncotarget 2017 8:95023-29.10.18632/oncotarget.2183229212287 [Google Scholar] [CrossRef] [PubMed]
[23]. Xue M, Masand P, Thompson P, Finegold M, Leung DH, Angiosarcoma successfully treated with liver transplantation and sirolimusPediatr Transplant 2014 18(4):114-19.10.1111/petr.1224524641525 [Google Scholar] [CrossRef] [PubMed]
[24]. Huang NC, Kuo YC, Chiang JC, Hung SY, Wang HM, Hung YM, Hepatic angiosarcoma may have fair survival nowadaysMed. J 2015 94(19):01-10.10.1097/MD.000000000000081625984668 [Google Scholar] [CrossRef] [PubMed]