Population ageing is the most significant and inevitable result of demographic transition that is associated with improvement in health and medical care. The percentage of the elderly population in India has been increasing rapidly and the share of geriatric population is projected to increase from 8 percent in 2015 to 19 percent in 2050 [1]. The rising prevalence of age-related health problems is becoming an important public health concern as proportion of older individuals in population grows [1].
Dementia is one of the major irreversible causes of disability and morbidity in aged people. It is a chronic and progressive syndrome where there is gradual deterioration in cognitive function (i.e., the ability to process thought) beyond the expected from normal ageing. It adversely affects the memory, thinking, comprehension, calculation, orientation, learning capacity, language and judgement sparing the consciousness which characteristically remains unaffected. Cognitive impairment is usually associated, and occasionally preceded, by declension in emotional control, motivation or social behaviour [2]. It is a compound syndrome characterised by global and irreversible cognitive decline that can jeopardise daily functioning with severe adverse consequences on social life, physical activities and quality of life. Dementia is precedent by Mild Cognitive Impairment (MCI). Cognitive deficit in MCI is less severe than in dementia. Usual daily activity is maintained masking its early detection in preclinical phase [3]. People with mild cognitive dysfunction showed upto 20% annual conversion rate to dementia [4].
Cognitive loss is one of the dimensions for poor quality of life especially in elderly population [5]. Early detection of dementia by screening at resource-poor settings can ensure better outcome and delay the progression of disease. Disability limitation and reversal of risk factors also have better opportunity to prevent progressive cognitive decline. At this moment, research should be focused on the development or optimisation of cost-efficient screening tools to identify people in the asymptomatic phase. There is a lack of population-based studies for cognitive screening instruments. Population based research could result in more insight as to how cognitive functions and biomarkers change with age [6].
Elderly population at risk of developing dementia is projected to increase in future in low and middle income country like India [7]. Health care services are often operated under constraints of trained human resources and equipment. So, there is a need for low-cost, quick, reliable and accurate screening tool [8].
MoCA tool was developed as a brief screening tool for detecting Cognitive dysfunction [9]. Studies undertaken in various countries revealed MoCA as accepted tool in screening for Cognitive Impairment [10]. There are several limitations of this tool. The screening with MoCA needs trained personnel and is more time-consuming [11]. So it is difficult to use it in community level in resource poor settings.
The AQ was validated as screening tool to screen cognitive dysfunction mostly in studies in western world [12]. Till date, no studies have evaluated the AQ’s performance in the Indian population. Present study aimed to find out the accuracy of AQ compared to MoCA tools in Cognitive Impairment screening among the elderly population in a slum of Kolkata. Hypothesis of the study was that the result of screening Cognitive Impairment with AQ tool is in agreement with that of MoCA.
Materials and Methods
A community based prospective cross-sectional study was conducted from June to September 2019 in urban field practice area of All India Institute of Hygiene and Public Health, Kolkata. This study was approved by Institutional Ethics Committee of AIIH & PH with IEC certificate no. PSM/IEC/2018/3. Study population was elderly people (≥60 years) in the study area. The AQ form was filled-up with the help of primary care giver of the study participant.
Inclusion criteria: Those who were residing for more than one year in that area were included.
Exclusion criteria: Those persons who did not give informed written consent, whose primary caregiver was not present during the time of data collection, who could not read or write Bengali, who was known case of dementia and unable to respond due to visual and/or auditory disability even with corrective measures were excluded.
Sample size was calculated using Buderer’s formula based on sensitivity,
Where, n=required sample size, SN=anticipated sensitivity, Z1-α=standard normal deviate corresponding to confidence interval and L=absolute precision desired on either side (half-width of the confidence interval) of sensitivity [13]. Based on the reported prevalence of MCI among elderly population (≥60 years) as 26% in a study done at urban area of Kerala, South India [14]. Taking confidence interval as 95% with Z1-α=1.96; absolute error (L)=10%, anticipated sensitivity of AQ was 90% and estimated prevalence was 26%, minimum sample size required was 133. Total 140 elderly members were selected for this study.
Urban field practice area had three units, of which one unit was chosen randomly. From the household register of that unit, a sampling frame of households having elderly member was prepared. Simple random sampling was used to select such 140 households. Elderly members of those household and their primary caregivers were interviewed. Non willing participants were replaced by randomly selected new individuals. For households having more than one elderly person, one member was selected by lottery method.
Study Tools
A predesigned, pretested, structured schedule containing sociodemographic attributes was used for interview. Cognitive impairment was measured by both MoCA Questionnaire Version 7.1 (validated Bengali version) and & AQ (Bengali version) [11]. These instruments were checked for face and content validity by the experts of AIIH & PH.
The AQ tool was translated in Bengali and back-translated to English and validation was carried out by an expert committee of AIIH & PH maintaining semantic equivalence. Final corrected Bengali version of AQ tool was used in current study. Pre-testing of this tool was conducted and internal consistency was calculated using the inter-item reliability. {Cronbach’s alpha (α) =0.757}.
MoCA was a 30-point test where score below 26 was considered as cognitive impairment.
Almost 10 to 15 minutes was given for screening using MoCA. MoCA assessed various domains of cognitive loss. Drawing a clock (three points) and copying a three-dimensional cube (one point) were used to ascertain the visuo-spatial abilities. Short-term memory (five points) was assessed by two learning trials of five nouns and delayed (nearly five minutes) recall of that. Alternation task (one point) which was adapted from the Trail Making B task, a phonemic fluency task (one point), and a two-item verbal abstraction task (two points) was carried out for assessment of executive functions. Whereas, target detection by tapping (one point), serial subtraction (three points), and digits forward and backward method (one point each) were conducted for attention, concentration and working memory. Linguistic ability was assessed using a three-item (lion, camel and rhinoceros) confrontation naming task (three points), repetition of two syntactically complex sentences with fluency (two points). Finally, Spatio-temporal orientation was evaluated (six points).
AQ consisted of 21 items with weighted yes/no options and five domains including memory, orientation, functional ability, visuo-spatial and language. Points for affirmative response were scored as one and total score was calculated. Attainable score for AQ ranged from 0 to 27. MCI was suggested by a score between 5 and 14. A score of 15 or more points indicated Alzheimer’s disease. Score five or more in AQ tool was taken for cognitive impairment [12].
Participants were interviewed with the schedule following rapport building and brief description of process. Informed written consent was obtained from all participants and their primary care-givers. MoCA was filled up by participants whereas AQ was administered by care-giver of the participants. Confidentiality was maintained throughout the process.
Statistical Analysis
Data was analysed using Microsoft Excel 2007 and Statistical Package for the Social Sciences version 16 (SPSS for Windows, version 16.0, SPSS Inc., Chicago, USA) software. Descriptive and Inferential statistics were performed. Agreement of cognitive impairment diagnosed by MoCA and AQ was assessed by Cohen’s kappa (κ) [15]. Correlation between AQ and MoCA was assessed using Spearman’s Rho Correlation coefficient as both of these variable did not have normal distribution [16]. Validity of screening test for cognitive impairment using AQ tool was calculated considering MoCA as gold standard in previously mentioned cut-off. ROC curve and Youden Index was used to find out optimum cut-off for AQ to screen cognitive impairment [17]. Confidence Interval of prevalence, Cohen’s Kappa, Likelihood Ratio was calculated using Standard error formula [18]. For confidence Interval of Sensitivity, Specificity and Predictive values, the Wilson Score confidence interval was used [19]. For confidence Interval of Spearman correlation coefficient, the Fisher z-transformation was used [20].
Results
Mean age of study population was 68.4 years (SD±7.1) with a range of 60-100. Nearly half (55.7%) of them were male. Majority (90%) of study population belonged to Hindu religion. Mean years of schooling was 4.1 (±3.9) years whereas 40.7% had no formal education. Approximately, 29.4% of the study participants belonged to Class IV socioeconomic status according to Modified BG Prasad scale 2019 [Table/Fig-1] [21].
Distributions of background characteristics of the study participants (N=140).
| Variable | Characteristics | Number (%) | Descriptive statistics |
|---|
| Gender | Female | 62 (44.3) | _ |
| Male | 78 (55.7) |
| Age (in years) | 60-69 | 84 (60.0) | Range=60 to 100Mean (SD)=68.4 (7.1)Median (IQR)=68 (63, 71) |
| 70-79 | 43 (30.7) |
| 80-89 | 10 (7.1) |
| ≥90 | 3 (2.2) |
| Educational level | Illiterate | 57 (40.7) | Years of schoolingRange=0 to 12Mean (SD)=4.1 (3.9)Median (IQR)=4 (0,8) |
| Below primary | 18 (12.9) |
| Primary | 17 (12.1) |
| Middle | 41 (29.3) |
| Secondary and above | 7 (5.0) |
| Religion | Hindu | 126 (90.0) | _ |
| Muslim | 14 (10.0) |
| Marital status | Married | 73 (52.1) | _ |
| Never married | 6 (4.3) |
| Widow/widower | 61 (43.6) |
| Modified BG Prasad Social class (2019) [21] | I | 15 (10.7) | Per Capita Income (INR)Range=400 to 11000Mean (SD)=2683.7 (31960.3)Median (IQR)=2183.3 (1407.1, 3333.3) |
| II | 23 (16.4) |
| III | 37 (26.4) |
| IV | 41 (29.4) |
| V | 24 (17.1) |
| Major occupation | Business | 15 (10.7) | _ |
| Skilled labour | 23 (16.4) |
| Unskilled labour | 37 (26.4) |
| Housemaid | 41 (29.4) |
| Homemaker | 24 (17.1) |
| Currently employed | Yes | 26 (18.6) | _ |
| No | 114 (81.4) |
The proportion of cognitive impairment using MoCA tool and AQ tool was 40% (95%CI=31.8-48.6) and 36.4% (95% CI=28.5-45.0), respectively [Table/Fig-2].
Agreement of AQ and MoCA tool for Cognitive Impairment (N=140).
| Agreement* | Montreal Cognitive Assessment (MoCA) | |
|---|
| Alzheimer Questionnaire (AQ) | Cognitive impairment | Normal | Total |
|---|
| Cognitive impairment | 48 (34.3) | 3 (2.1) | 51 (36.4) |
| Normal | 8 (5.7) | 81 (57.9) | 89 (63.6) |
| Total | 56 (40) | 84 (60) | 140 (100) |
*Cohen’s kappa; κ=0.834 (95% CI= 0.739-0.928)
The current study hypothesised that screening of Cognitive Impairment with AQ tool was in agreement with that of MoCA which was evident from the good agreement (Cohen’s kappa, κ=0.834, 95% CI=0.739-0.928) between AQ and MoCA.
The AQ and MoCA showed strong negative correlation (Spearman correlation coefficient, ρ=-0.709, 95% CI=0.764-0.884, p-value <0.001).
Sensitivity and specificity of AQ for detecting cognitive impairment were 85.7% (95% CI=74.2-92.6%) and 96.4% (95% CI=89.9-98.7%). Positive predictive value of this tool was 94.1% (95% CI=84.0-97.9%) i.e., majority of cognitive impairment cases screened by AQ tool were true positive. Negative predictive value also revealed that this tool successfully identified 91.0% (95% CI=83.2-95.4%) participants with normal cognition. Positive likelihood ratio revealed that participant with cognitive impairment had 23.8 times higher likelihood of being screened as cognitively impaired by AQ tool than persons with normal cognition. Negative likelihood ratio revealed that a participant with impaired cognition had 0.148 times higher likelihood of being screened as normal than person with normal cognition [Table/Fig-3].
Diagnostic accuracy of Alzheimer Questionnaire (AQ) for screening cognitive impairment.
| Measures | Value (95% CI) |
|---|
| Sensitivity | 85.7% (74.2-92.6) |
| Specificity | 96.4% (89.9-98.7) |
| Positive predictive value | 94.1% (84.0-97.9) |
| Negative predictive value | 91.0% (83.2-95.4) |
| Positive likelihood ratio | 23.80 (7.80-72.68) |
| Negative likelihood ratio | 0.148 (0.08-0.28) |
In ROC curve, AQ tool showed excellent performance to anticipate cognitive impairment compared to the MoCA revealed by AUC value (C-statistic) of 0.915 (95% CI=0.858-0.972) [Table/Fig-4].
ROC curve showing validity of AQ tool using MoCA tool as gold standard.
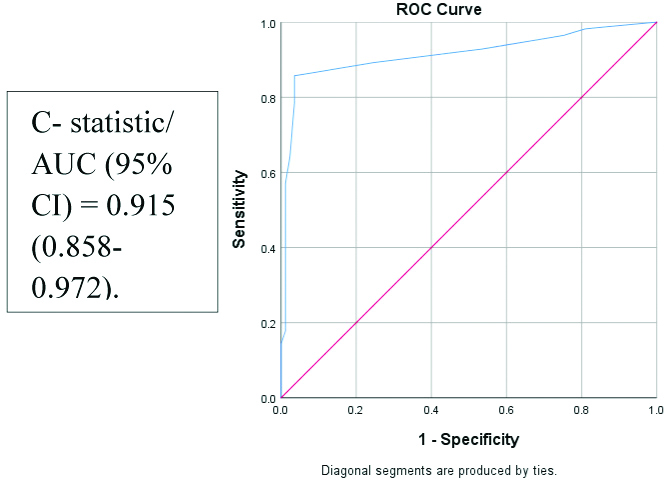
The Youden index of 0.821 showed highest sum of sensitivity and specificity of AQ tool at 4.5 score to anticipate cognitive impairment. However, AQ score had only integer values. Thus, optimal cut-off to determine cognitive impairment should be 4 or 5 in AQ scale. As Youden index at score 3.5 and 5.5 was 0.643 and 0.750, respectively, optimal cut-off lied between 4.5 and 5.5, i.e., 5.
Discussion
Current study showed cognitive impairment was found in substantial magnitude among urban elderly population. More than one-third of this population were found as cognitively impaired by MoCA (40%) and AQ (36.4%). Alkhunizan M et al., found similar prevalence (45%) among elderly in Saudi Arabia using MoCA [22].
Agreement and Correlation
AQ showed good strength of agreement (Cohen’s kappa, κ=0.834) which suggested that AQ was concurrently valid with MoCA. Thus, this tool can be used in place of MoCA especially in resource poor settings. Moreover, AQ showed strong correlation (-0.709) with MoCA for screening cognitive impairment which was inconsistent with findings by Malek-Ahmadi M et al., (r=-0.46), Budolfson K et al., (r=-0.68) showing moderate correlation between these tools [23,24]. This discordance might be attributed to differential study design as those were case-control studies unlike current study which adopted cross-sectional design.
Validity of AQ for Screening Cognitive Impairment
In this study, AQ demonstrated sensitivity and specificity for screening cognitive impairment as 85.7% and 96.4%, respectively which was comparable to previous studies by Sabbagh MN et al., (sensitivity=86.96%, specificity=94%) and Malek-Ahmadi M et al., (sensitivity=89%, specificity=91%) [23,25].
Current study showed AUC value of 0.915 in ROC curve which was comparable to study by Sabbagh MN et al., (AUC value of 0.95) both showing excellent performance to anticipate cognitive impairment compared to the MoCA [25]. In contrast, another study by Malek-Ahmadi M et al., demonstrated AUC value of AQ as 0.74 which was much lower than that of current study. It was possibly due to different criteria used for diagnosing patients with cognitive impairment [23].
In the current study, AQ showed positive and negative likelihood ratio of 23.8 and 0.148 for cognitive dysfunction screening which indicated that AQ was extremely good in those whose disease status was known. But Malek-Ahmadi M et al., found positive and negative likelihood ratio of 9.89 and 0.12 in their study which indicated that AQ was of moderate utility in those whose disease status was known [12].
There was dearth of studies regarding evaluation of AQ tool for screening cognitive impairment in existing literature. Prevalence of cognitive impairment using AQ was also rarely shown in elderly population especially in India. Thus, community-based design in current study enabled the researchers to find out prevalence of cognitive impairment among elderly using both AQ and MoCA tool and to calculate validity in terms of sensitivity, specificity as well as predictive values. This was an important strength of this study. Use of robust sampling technique and rigorous statistical methods were other strengths of this study. ROC curve was used for determination of optimum cut-off for cognitive impairment by AQ which further augmented the robustness of the current study.
Limitation(s)
However, grading of cognitive dysfunction as amnestic MCI, dementia and Alzheimer Disease was not conducted in this study. Thus, stratified analysis of validity in different degrees of cognitive loss could not be carried out. Persons with visual and auditory impairment were excluded from this study as they could not perform the tasks specified in MoCA. This exclusion disabled the researchers to find out burden of cognitive dysfunction in those persons. Moreover, this study was restricted to urban geriatric population, thus future studies should be conducted among rural counterparts to identify any geographical variations.
Conclusion(s)
Current study found that informant-based AQ was equally capable as MoCA in screening cognitive impairment. Thus, it can be used in community screening even by grass root level health workers in contrast to MoCA which was difficult to perform and need expertise to analyse. This will help in early detection of cognitive dysfunction in the community initiating early referral and management.
This study also showed high prevalence of cognitive impairment in urban elderly population. Thus, initiation of cognitive screening using AQ among elderly in primary health care level is the need of the hour. This screening can be incorporated in ongoing National Programme for Healthcare of Elderly (NPHCE). This in turn will keep the vulnerable elderly group healthy to cope-up with the age-related challenges for better survival.
*Cohen’s kappa; κ=0.834 (95% CI= 0.739-0.928)