Pleural effusions are one of the most common entities encountered by pulmonologists worldwide on a daily basis in both out-patient and emergency setting and accounts for around 4% of patients on pulmonology practice [1,2]. Evaluation of these patients begins with detailed history taking, physical examination, and chest radiography. This is followed by diagnostic thoracocentesis in which pleural fluid is aspirated and sent for biochemical, microbiological and cytological evaluation to determine the cause of the effusion. The yield of thoracocentesis varies and is usually around 60% for malignancy and 90% for tuberculosis [3,4]. If this does not lead to a definitive diagnosis, the next step usually is blind or USG-guided closed pleural biopsy. Its addition to thoracocentesis increases the diagnostic yield in malignant pleural effusion to about 70% [4,5]; thus, even after thoracocentesis and closed pleural biopsy, around 20-25% of pleural effusions remain undiagnosed [6]. Thus, it becomes challenging to find a cause for effusions in these patients.
Medical thoracoscopy, which is also referred to as pleuroscopy, has gained a lot of popularity in recent times for the evaluation of undiagnosed pleural effusions because of its high sensitivity and low risk of complications. It is a minimally invasive procedure which allows for endoscopic evaluation of pleural space in its entirety [7]. It can be performed under local anaesthesia or conscious sedation. It allows one to visualise the pleural surface, examine it and perform limited diagnostic and therapeutic procedures [7]. When compared with Video-Assisted Thoracoscopic Surgery (VATS), it is less invasive, can be performed as a day care procedure, is significantly cheaper and can be done even in frail patients who would otherwise not tolerate VATS due to their poor general conditions [8].
This study was aimed at detecting the diagnostic yield of Medical Thoracoscopy in cases of exudative, lymphocytic and pleural effusion of undiagnosed aetiology. It also aims to identify and study the complications associated with thoracoscopy.
Materials and Methods
This was a prospective observational study being carried out in the Department of Pulmonary Medicine, Jawaharlal Nehru Medical College and Hospital, from August 2016 to August 2018. The study was performed after receiving clearance from the Institutional Ethics Committee (letter no. 1918/FM). Fifty patients of pleural effusions of undiagnosed aetiology were enrolled in this study after taking prior informed consent.
Inclusion criteria:
Age >18 years for both male.
Undiagnosed pleural effusion was defined as pleural effusion having exudative pleural effusions as per Light’s criteria [9], lymphocyte-predominant, ADA levels <70 IU/L and cytology must be negative for malignancy [10].
No known underlying lung pathology causing pleural effusion like Pulmonary Tuberculosis (PTB) or malignancy.
Patients willing to give consent for thoracoscopy.
Surgically fit patients.
Exclusion criteria:
Age <18 years and Pregnant female patients.
Patients with transudative pleural effusion according to Light’s criteria.
Patients whose initial pleural fluid examination could lead to a definitive diagnosis.
Patients who did not give consent for thoracoscopy and were not fit for performing thoracoscopy were excluded as in the following cases:
Those with severe uncorrected hypoxemia despite continuous oxygen administration.
Unstable cardiovascular or haemodynamic status.
Coagulation defects.
Platelet counts <60,000/mL.
Pleural space obliterated by fibrous tissue.
Honeycomb lung, pulmonary arterio-venous aneurysms, suspected hydatid cysts, and highly vascular pulmonary lesions.
Investigations
Full history taking and detailed clinical examination.
Investigations:
Full routine laboratory investigations: Complete Blood Count (CBC), Renal Function Test (RFT), Blood Sugar (BS), Liver Function Test (LFT) and bleeding profile.
Sputum smear examinations for the presence of acid-fast bacilli.
Radiological examination: Chest X-rays, Computed Tomography (CT) scan (whenever needed).
Pleural fluid examination: Bacteriological, biochemical and cytological.
Thoracoscopic examination of the pleural space using flexi-rigid thoracoscopy.
Procedure
Patients were kept fasting for six hours before the procedure. Intravenous access was secured in the upper limb of the opposite side and patients were made to lie in lateral decubitus position with the affected side up. Continuous monitoring of pulse rate and oxygen saturation was done throughout the procedure using a finger probe. The procedure was done in conscious sedation using midazolam (0.05 mg/kg) and fentanyl (50 mcg). The lateral chest wall was cleaned with povidone-iodine and spirit. Infiltration anaesthesia was used (10 to 15 mL of 2% lignocaine).
A skin incision of about 1.5 cm was made in 5th or 6th Intercostal Space (ICS) in mid-axillary line and the subcutaneous tissue and intercostal muscles were then bluntly dissected to reach the pleural cavity. Then, a trocar with cannula was inserted into the pleural cavity. Trocar was then removed and flexi-rigid thoracoscope and was then inserted through the cannula. Pleural fluid was suctioned until the pleural surfaces were clearly visible. The pleural cavity was then thoroughly inspected to visualise the diaphragmatic, costal and visceral pleura. Adhesions, if present were gently broken using the thoracoscope itself or by biopsy forceps. Any abnormal-looking area was biopsied using biopsy forceps. Usually, 3-6 biopsies were taken. If no gross abnormalities were found on parietal pleura, multiple biopsies were taken from different areas. In the end, a chest tube with underwater seal was placed via the insertion site after removing the cannula. The drain was removed once the lung had expanded and the output from the drain was less than 50 mL a day.
Statistical Analysis
All the data were collected, tabulated and analysed using the Statistical Package for the Social Sciences (SPSS) version 25. The results were presented as mean±SD or percentage. Differences in categorical data were compared using the chi-square test or the Fisher-exact test. A p-value of <0.05 was considered statistically significant.
Results
A total of 50 patients underwent thoracoscopy for undiagnosed pleural effusion. The epidemiological and basic clinical profile of the study population is shown in [Table/Fig-1].
Epidemiological profile of patients.
| Paramter | Mean/Number (%) |
|---|
| Age (Mean±SD) | 52.74±15.4 |
| Gender |
| Male | 30 (60%) |
| Female | 20 (40%) |
| Smoking history |
| Smokers | 28 (56%) |
| Non-smokers | 22 (44%) |
| Site of effusion |
| Right | 28 (56%) |
| Left | 17 (34%) |
| Bilateral | 5 (10%) |
| Colour of effusion |
| Haemorrhagic | 27 (54%) |
| Straw coloured | 23 (46%) |
| Symptoms |
| Dyspnea | 40 (80%) |
| Chest pain | 37 (74%) |
| Cough | 36 (72%) |
| Fever | 33 (66%) |
| Weight loss | 15 (30%) |
| Haemoptysis | 4 (8%) |
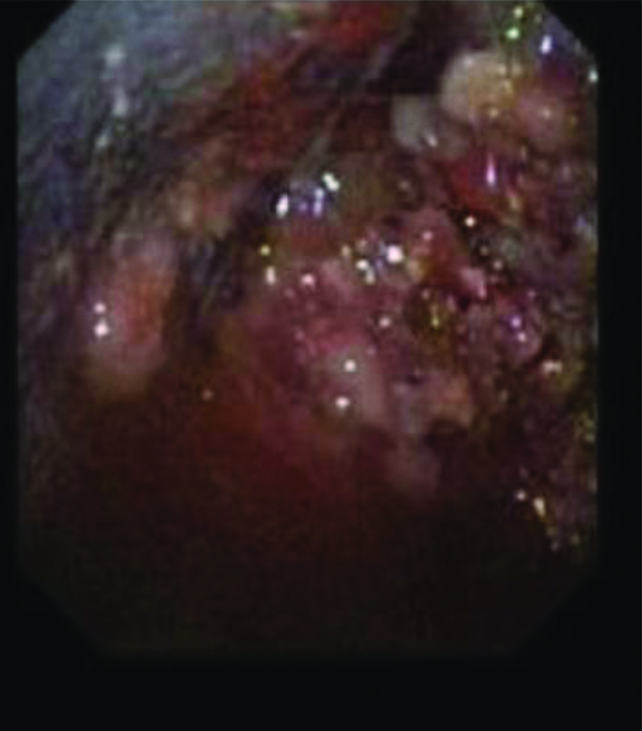
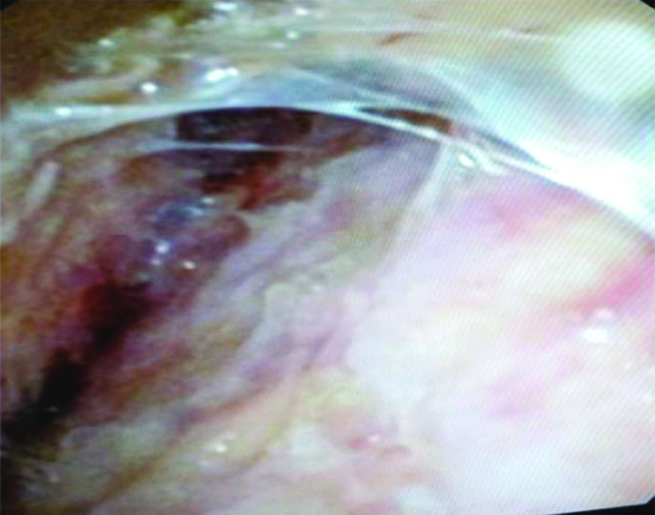
The most common gross thoracoscopic finding seen was nodules [Table/Fig-2], seen in 46% followed by pleural thickening with adhesions [Table/Fig-3] in 40%, sago grain appearance [Table/Fig-4] in 6% and normal looking pleura was seen in 8%.
Gross thoracoscopic image showing nodules.
Gross thoracoscopic image showing pleural thickening with adhesions.
Gross thoracoscopic image showing sago grain appearance.

On histopathological examination, malignancy was the most common finding, seen in 44% of the patients. The most common malignancy seen was Metastatic Adenocarcinoma, which was observed in 13 (26%) patients. The most common source of primary malignancy in those having metastatic adenocarcinoma was lungs (9/13) followed by breast (2/13) [Table/Fig-5]. In those having malignancy, 86% (19/22) patients had haemorrhagic effusion while 84% (16/19) of tubercular patients had straw coloured effusion [Table/Fig-6].
Gross thoracoscopic and histopathological findings.
| Findings | No (%) |
|---|
| Gross thoracoscopic findings |
|---|
| Nodules | 23 (46%) |
| Pleural thickening with adhesions | 20 (40%) |
| Sago grain appearance | 3 (6%) |
| Normal looking pleura | 4 (8%) |
| Histopathological findings |
| Malignancy | 22 (44%) |
| Tuberculosis | 19 (38%) |
| Non-specific inflammation | 6 (12%) |
| Fibro-collagenous tissue | 3 (6%) |
| Types of malignancy |
| Metastatic adenocarcinoma | 13 (26%) |
| Poorly differentiated carcinoma | 7 (14%) |
| Squamous cell carcinoma | 1 (2%) |
| Mesothelioma | 1 (2%) |
Shows frequency of different histopathological findings having haemorrhagic or straw coloured effusion.
| Colour of effusion | Histopathology |
|---|
| Malignancy | Tubercular | Non-specific Inflammation | Fibro-collagenous tissue |
|---|
| Haemorrhagic | 19 | 3 | 3 | 2 |
| Straw coloured | 3 | 16 | 3 | 1 |
| Total | 22 | 19 | 6 | 3 |
In patients having nodules, majority were ultimately diagnosed as having malignancy (19/23), while in those having pleural thickening only with adhesions, majority were diagnosed as tubercular (13/20). Sago grain appearance was seen exclusively in tubercular patients [Table/Fig-7]. No major complications were seen. Minor complications like bleeding, prolonged air leak and empyema were seen in 2, 2 and 1 patient, respectively. The average duration of Intercostal Tube Drainage (ICD) tube was 4.42 days. The diagnosis could be made in 41 out of the total 50 patients (82%). The data was statistically significant. (χ2=20.48, p-value <0.001).
Showing frequency of histopathological findings as various gross thoracoscopic finding.
| HPE | Gross thoracoscopic findings |
|---|
| Nodules | Pleural thickening with or without adhesions | Sago grain | Normal pleura |
|---|
| Malignancy | 19 | 3 | 0 | 0 |
| Tubercular | 2 | 13 | 3 | 1 |
| Nonspecific Inflammation | 2 | 1 | 0 | 3 |
| Fibrocollagenous tissue | 0 | 3 | 0 | 0 |
| Total | 23 | 20 | 3 | 4 |
Discussion
The present study was done with an aim to find out the diagnostic yield of medical thoracoscopy in patients with undiagnosed exudative lymphocytic pleural effusion and also to analyse the complications associated with it.
In this study, the diagnostic yield of thoracoscopy came out to be 82%. The study was able to make a diagnosis in 41 out of 50 patients. The diagnostic yield in other studies was also similar and ranged from 74.3% to 95.5% [10-18]. In some studies, the authors have also included non-specific inflammation as a separate diagnosis but the study has classified them under undiagnosed aetiology [12,17]. In present study, majority of those having haemorrhagic effusion turned to be malignant (70.37%) while in those having straw coloured effusion, majority were having benign cause (86.9%). This data came out to be statistically significant (p<0.001), which means the colour of effusion can give an initial idea as to whether we are dealing with a malignant or a benign cause. But it is not absolute, as those having haemorrhagic effusion could very well turn out to be non-malignant ultimately and vice versa. In the study done by Shah NN et al., 14 patients had malignancy of the 16 having haemorrhagic effusion, while in patients having straw-coloured effusion; none had malignancy [16]. In the study done by Agarwal A et al., [13], 90.9% patients having malignancy had a haemorrhagic effusion, while 9.1% patients of malignancy had a straw-coloured effusion. Also, in their study, 15% patients of tuberculosis had a haemorrhagic effusion.
The relatively low percentage of haemorrhagic effusion having malignancy in present study compared to other studies could possibly be due to more patients having undiagnosed aetiology even after thoracoscopy in this group who might have had a malignant aetiology.
In this study, nodules on gross thoracoscopy were seen in 23 patients (46%) of which 19 (82.6%) were malignant, two were tubercular, and two were due to non-specific inflammation. In other studies also, most of the nodules turned out to be malignant. In the study done by Prabhu VG and Narasimhan R, and Shah NN et al., 70% and 100% of the nodules turned out to be malignant, respectively [12,16]. In the study by Abd El Rehim IY et al., from Egypt, nodules were seen in 27 (75%) of the patients of which 22 were due to malignancy (81.48%) [19]. Pleural thickening/irregularity with or without adhesions was seen in 20 patients (40%), of which 13 were due to tuberculosis (65%), three due to malignancy (15%) and one case was due to non-specific inflammation.
In the study done by Prabhu VG and Narasimhan R, adhesions were seen in 26 patients (38.23%) of which >96% of patients had non-malignant aetiology [12]. In the study done by Shah NN et al., adhesions were seen in only two patients of which, one was due to malignancy and the other had non-specific inflammation [16]. In the study done by Helala LA et al., 100% of patients of adhesions had a nonmalignant disease [20]. In the index study, three patients had a sago grain appearance on gross thoracoscopy and all of them turned out to be tubercular. It was similar to the results seen in other studies [12,16,20]. Normal pleura were seen in four patients of which three were due to non-specific inflammation and one was due to tuberculosis. The results were similar to other studies. In the study done by Shah NN et al., five patients had normal pleura and all turned out to be due to chronic non-specific inflammation [16].
The data comparing the co-relation between different gross thoracoscopic findings and various histopathological results were statistically significant with a p-value of <0.001, which means this study could very well have an idea about the diagnosis just by the looks of the pleura during thoracoscopy findings. In some cases, like for sago grain appearance, the authors can say that it is 100% specific for tuberculosis. The same findings were observed in other studies as well [12,16,20]. There were no major complications seen in present study during or post-thoracoscopy. Although literature describes many complications such as subcutaneous emphysema (0.6-4.9%), prolonged air leak (0.5-8.1%), empyema (0.5-2.7%), haemorrhage (0.3-0.4%), shock (0.2%) and chest wall seeding by malignancy (0.5-4.0%) [10]. In the present study, five patients had complications, two had bleeding, two had a prolonged air leak and one patient developed empyema. The diagnostic yield of thoracoscopy depends upon several factors, which were analysed in-depth by Loddenkemper R and Boutin C, which includes, inadequate sampling (under looking of controversial gutter and diaphragm), pathological errors, the fibrinous layer covering the actual pathological area and the presence of dense adhesions [21]. Boutin C et al., in his study, concluded that the diagnostic yield of thoracoscopic pleural biopsy can be as high as 95% in malignant pleural effusion and 99% in tubercular pleural effusion which is to far superior compared to pleural fluid analysis and closed pleural biopsy [22]. Thus, thoracoscopic pleural biopsy is considered the gold standard in the diagnosis of malignant and tubercular pleural effusion [17].
Limitation(s)
In the present study, the procedure was not done by a single physician, with different skill sets and experience. Also, a bigger sample size would further validate the findings.
Conclusion(s)
The result of this study suggests that thoracoscopy is a relatively simple and safe procedure with a high diagnostic yield and a very low complication rate. Besides providing with the aetiological diagnosis, it also provides with the opportunity for some therapeutic procedures like adhesiolysis and pleurodesis. Therefore, thoracoscopy should be strongly considered in patients with undiagnosed, exudative pleural effusion especially where malignancy and tuberculosis is strongly suspected.