Bifurcation Disease: The Role of Proximal Optimisation Technique
Bhupesh Shah1, Nishit Sardava2, Nikita Chaturvedi3
1 Associate Professor, Department of Cardiology, NHL Municipal Medical College, Ahmedabad, Gujarat, India.
2 Resident, Department of Cardiology, NHL Municipal Medical College, Ahmedabad, Gujarat, India.
3 Resident, Department of Cardiology, NHL Municipal Medical College, Ahmedabad, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Bhupesh Shah, NHL Municipal Medical College, Ahmedabad, Gujarat, India.
E-mail: shahbhupesh@hotmail.com
Bifurcation lesions are both complex and challenging coronary lesion subsets in terms of lower procedural success and increased rates of long-term adverse cardiac events. Here described is a challenging case of a bifurcation lesion in a 60-year-old diabetic female with multi-vessel coronary artery disease. She presented with chest pain associated with perspiration, chest discomfort and mild breathlessness. In view of the diagnosis of acute coronary syndrome, all diseased vessels were stented and kissing balloon and Proximal Optimisation Techniques (POT) were performed yielding excellent results. This case emphasises the importance of POT, kissing balloon, and re-POT techniques in bifurcation intervention procedures that have been proven to facilitate success in such procedures. Moreover, interventional cardiologists should be familiar with all bifurcation techniques.
Diabetes mellitus, Kissing balloon technique, Left main coronary artery disease, Multi-vessel coronary artery disease, Percutaneous coronary intervention
Case Report
A 60-year-old female was admitted to the tertiary-care centre with complaints of chest pain since seven days. She had a medical history of ischaemic heart disease, hypertension and diabetes mellitus. Clinical history revealed the patient experienced chest pain associated with perspiration, chest discomfort and mild breathlessness (New York Heart Association grade II). Electrocardiography indicated T-inversions in leads V1-V6. 2D echocardiography showed 42% left ventricular ejection fraction, reduced left ventricular diastolic compliance, and apico-septal hyperkinesia. Coronary angiography revealed multi-vessel disease. The Left Main Coronary Artery (LMCA) had 30-40% diffuse stenosis. Proximal Left Anterior Descending (LAD) coronary artery had 60-70% stenosis, mid-LAD had 95% stenosis and distal LAD had 30-40% stenosis.
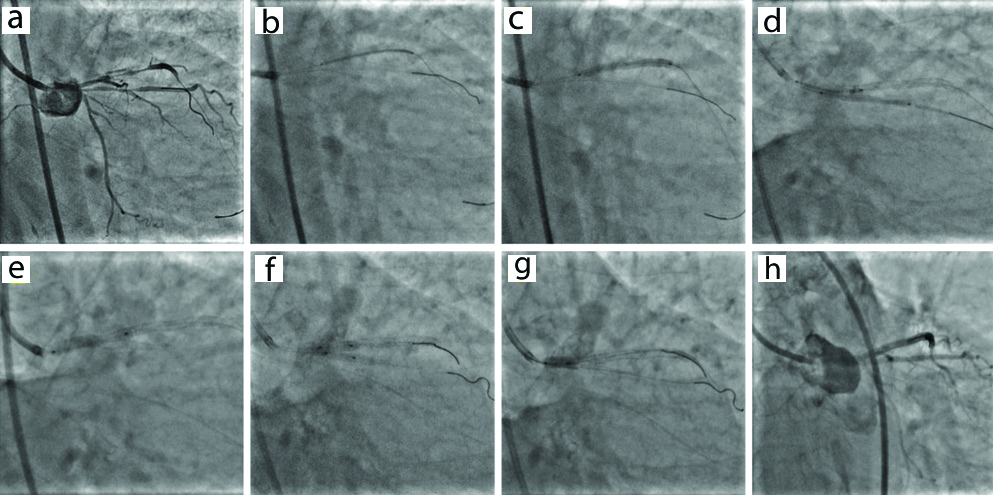
Furthermore, the first major septal branch had 90% stenosis in the proximal segment. Left Circumflex Artery (LCx) had plaque in the proximal segment and 70% stenosis in the mid-AV groove whilst the first Obtuse Marginal (OM) branch had 70% stenosis in the proximal segment and 90% stenosis in the mid segment. Right Coronary Artery (RCA) showed 50-60% stenosis in both proximal and mid RCA. In view of the diagnosis of acute coronary syndrome, stenting of all diseased vessels was planned [Table/Fig-1a]. The femoral vein was accessed and intravenous heparin (100 IU/kg) was administered to the patient. The LAD-LCx lesion was crossed with a 0.014 BMW (Balance Middle Weight) guidewire and LAD was pre-dilated with a 2.0×12 mm Maverick balloon (Boston Scientific, USA) at 10 atm. Proximal LAD was then negotiated and a 3.0×38 mm Promus Element Plus Everolimus-Eluting Stent (EES) (Boston Scientific, MA, USA), was deployed [Table/Fig-1b,c]. Next, LM-LAD was negotiated with a 3.5×23 mm Xience Prime EES (Abbott Vascular, Santa Clara, CA). Finally, ramus was pre-dilated with a 2.0×12 mm Maverick balloon (Boston Scientific, USA) at 16 atm, negotiated and a 2.5×28 mm Promus Element Plus EES (Boston Scientific, MA, USA) was deployed [Table/Fig-1d]. Guide-wire removed and the negotiated 3.5×23 mm Xience Prime EES was deployed in LM-LAD [Table/Fig-1e] and the lesion was postdilated with a 2.5×12 mm Sapphire balloon at 16 atm. Kissing balloon technique was performed in LAD and Ramus Intermedius (RI) [Table/Fig-1f,g] and a short 4.5 mm balloon was inflated in the left main artery to perform POT [Table/Fig-1h]. An excellent final result was achieved on coronary angiography. Postprocedure the patient is doing well. Check angiography will be scheduled at the 6 and 12-month follow-ups.
Coronary angiography showing: (a) Multi-vessel coronary artery disease, (b,c) Proximal left anterior descending coronary artery disease (LAD) negotiated and 3.0×38 mmPromus Element Plus Everolimus-Eluting Stent (EES) deployed at 12 am, (d) 2.5×28 mm Promus Element Plus EES deployed from ostium of ramus (e) 3.5×23 mm Xience Prime EES deployed in left main (LM) to LAD lesion, and (f,g) Kissing balloon technique performed in LAD and ramus intermedius and a short 4.5 mm balloon inflated in LM stem to perform proximal optimisation technique, and (h) Excellent final result.
Discussion
The present case reported with chest pain associated with perspiration, chest discomfort and mild breathlessness. She was later diagnosed with acute coronary syndrome. POT technique was employed to treat the challenging bifurcation lesion in the 60-year-old diabetic female with multi-vessel coronary artery disease. Similarly, Hoye A illustrated use of POT in a 67-year-old patient admitted with acute coronary syndrome [1]. A second case by Hoye A used POT in a two-stent strategy in a 79-year-old patient with acute coronary syndrome. The patient also experienced on-going symptoms of chest discomfort as observed in the present case. Furthermore, Kumar S described a patient presenting with left-sided chest pain and sweating [2]. The operators opted for provisional stenting using POT-side-POT technique over conventional two-stent implantation strategy. McGeoch RJ et al., have ventured further and reported one of the first cases of proximal optimisation and kissing balloon inflation within bioresorbable vascular scaffolds, using optical coherence tomography guidance [3].
Bifurcation lesions present as complex coronary interventions owing to their unique fractal anatomy. The diameter of the vessel proximal to the bifurcation is always larger than the diameter of the main vessel distal to the bifurcation. POT technique reconstructs normal geometry of the coronary tree by compensating for this discrepancy in vessel diameter. It further has several advantages: (i) it facilitates full stent apposition proximal to the bifurcation, thereby reducing strut mal-apposition; (ii) it precludes unintended wires or device passage behind stent struts; (iii) it facilitates side branch wiring by expanding stent cells overlying the side branch ostium, thereby allowing optimal re-cross through distal cells; and (iv) it improves final stent deformation following kissing balloon inflation or side branch dilation, thus optimising final stent geometry and flow dynamics [1]. According to the 14th European Bifurcation Club consensus document [4], POT is recommended as a mandatory step of bifurcation stenting.
The discrepancy in diameter size of both the vessels also plays a critical role in stent selection. If the diameter of the proximal main vessel is considered, the stent will be over-sized for the distal main vessel consequencing shifting of the carina. Alternatively, if the diameter of the distal main vessel is considered, the stent will be under-sized at the proximal main vessel, causing stent mal-apposition and possibly stent thrombosis. Moreover, these may not be revealed by angiography or ‘tactile feedback’ of ease of wire passage [1]. However, optical coherence tomography is one such imaging modality that may detect stent mal-apposition [5]. Contrary to reports on the kissing balloon technique in one-stent strategies [6-8], kissing balloon technique has been proven to mitigate rates of stent thrombosis, restenosis, target lesion failure, and major adverse cardiovascular rates in two-stent strategies [1,9]. Although kissing balloon technique is associated with elliptical deformation, a final POT can achieve circular geometry of the stent [10]. In line with this evidence, POT was performed towards the end of the procedure.
Conclusion(s)
Proximal Optimisation Techniques, kissing balloon technique, and re-POT are an essential part of bifurcation intervention procedures and have been proven to facilitate success in such procedures. Interventional cardiologists should be familiar with all bifurcation techniques. Imaging should be done whenever available according to hospital protocol.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 02, 2020
Manual Googling: Jul 21, 2020
iThenticate Software: Aug 10, 2020 (12%)
[1]. Hoye A, The proximal optimisation technique for intervention of coronary bifurcationsInterv Cardiol 2017 12(2):110-15.10.15420/icr.2017:11:2 [Google Scholar] [CrossRef]
[2]. Kumar S, Which strategy for bifurcation lesions? Provisional or two stent: A dilemmaHeart India 2019 7(1):31-33.10.4103/heartindia.heartindia_39_18 [Google Scholar] [CrossRef]
[3]. McGeoch RJ, Tanaka K, Overgaard CB, Bezerra HG, Džavík V, Proximal optimisation technique and kissing balloon inflations with the bioresorbable vascular scaffold for coronary bifurcation percutaneous coronary interventionCan J Cardiol 2014 30(11):1461. e5-e7.10.1016/j.cjca.2014.06.01425442451 [Google Scholar] [CrossRef] [PubMed]
[4]. Banning AP, Lassen JF, Burzotta F, Lefèvre T, Darremont O, Hildick-Smith D, Percutaneous coronary intervention for obstructive bifurcation lesions: The 14th consensus document from the European Bifurcation ClubEuroIntervention 2019 15(1):90-98.10.4244/EIJ-D-19-0014431105066 [Google Scholar] [CrossRef] [PubMed]
[5]. Otake H, Shite J, Ako J, Shinke T, Tanino Y, Ogasawara D, Local determinants of thrombus formation following sirolimus-eluting stent implantation assessed by optical coherence tomographyJACC Cardiovasc Interv 2009 2(5):459-66.10.1016/j.jcin.2009.03.00319463471 [Google Scholar] [CrossRef] [PubMed]
[6]. Korn Hv, Yu J, Ohlow MA, Huegl B, Schulte W, Wagner A, Interventional therapy of bifurcation lesions: A TIMI flow-guided concept to treat side branches in bifurcation lesions-A prospective randomized clinical study (Thueringer bifurcation study, THUEBIS study as pilot trial)Circ Cardiovasc Interv 2009 2(6):535-42.10.1161/CIRCINTERVENTIONS.108.83304620031771 [Google Scholar] [CrossRef] [PubMed]
[7]. Niemelä M, Kervinen K, Erglis A, Holm NR, Maeng M, Christiansen EH, Randomized comparison of final kissing balloon dilatation versus no final kissing balloon dilatation in patients with coronary bifurcation lesions treated with main vessel stenting: The Nordic-Baltic Bifurcation Study IIICirculation 2011 123(1):79-86.10.1161/CIRCULATIONAHA.110.96687921173348 [Google Scholar] [CrossRef] [PubMed]
[8]. Zhong M, Tang B, Zhao Q, Cheng J, Jin Q, Fu S, Should kissing balloon inflation after main vessel stenting be routine in the one-stent approach? A systematic review and meta-analysis of randomized trialsPloS one 2018 13(6):e019758010.1371/journal.pone.019758029949587 [Google Scholar] [CrossRef] [PubMed]
[9]. Gaido L, D’Ascenzo F, Imori Y, Wojakowski W, Saglietto A, Figini F, Impact of kissing balloon in patients treated with ultrathin stents for left main lesions and bifurcations: An analysis from the RAIN-CARDIOGROUP VII StudyCirc Cardiovasc Interv 2020 13(3):e00832510.1161/CIRCINTERVENTIONS.119.00832532102566 [Google Scholar] [CrossRef] [PubMed]
[10]. Rigatelli G, Dell’Avvocata F, Zuin M, Vassiliev D, Mazza A, Dinh HD, Complex coronary bifurcation revascularization by means of very minimal crushing and ultrathin biodegradable polymer DES: Feasibility and 1-year outcomes of the “Nano-crush” techniqueCardiovasc Revasc Med 2017 18(1):22-27.10.1016/j.carrev.2016.07.00327566904 [Google Scholar] [CrossRef] [PubMed]