Novel COVID-19 Global Outbreak and a Need for Proactive Dental Care
Prachi Gupta1, Abhinav Garg2, Lovejeet Ahuja3
1 Senior Resident, Department of Periodontology and Oral Implantology, Laxmibai Institute of Dental Sciences and Research, Patiala, Punjab, India.
2 Senior Resident, Department of Oral and Maxillofacial Surgery, Laxmibai Institute of Dental Sciences and Research, Patiala, Punjab, India.
3 Senior Resident, Department of Paediatric and Preventive Dentistry, Dashmesh Dental College, Faridkot, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Abhinav Garg, DANTCARE, Roxy Complex, Outside Sunami Gate, Sangrur, Punjab, India.
E-mail: garg.abhinav04@gmail.com
The global pandemic Novel Coronavirus Disease (COVID-19), which originated in Wuhan, has affected the countries worldwide and has been declared as a public health emergency by World Health Organisation. Because of the exclusive features of dental healthcare set-ups, risk of cross-contamination is greater between patients and dental personnel due to high chances of getting in contact with suspected or asymptomatic COVID-19 patients. Preventive measures are essential to be taken for prevention of furthermore spread of nosocomial infection. The present article provides a brief overview on COVID-19 in dental settings and recommended protocols for screening/assessment, patient management and precautions for dental health care professionals.
Coronavirus disease, Dental health care professionals, Novel coronavirus disease 2019, Personal protective equipment, Precautions, Severe acute respiratory syndrome coronavirus
Introduction
The widespread pandemic outbreak of coronavirus and its associated disease (COVID-19) have become a major concern worldwide and pose a solemn threat to human well-being, health and survival. The causative agent responsible for this novel disease is the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) [1] [Table/Fig-1] [2]. There are various transmission modes of the nosocomial outbreak such as Airborne spread (via cough, sneeze, respiratory droplets inhalation [3] or aerosols generation in the dental care settings [4]), Contact transmission (direct oral-mucosal contact via droplets/aerosols [5] or indirect via contaminated dental equipments and dental healthcare settings [6]) and feco-oral route of transmission [7]. The average latency period of novel coronavirus disease is approximately 5-6 days, but it could be as long as 14 days [8]. Most of the patients reported signs and symptoms including fever, cough, loss of taste and sensation, fatigue, myalgias, short breath, anorexia, sputum production, headache, confusion, rhinorrhoea, sore throat, haemoptysis and diarrhoea [9].
This illustration, created at the Centers for Disease Control and Prevention (CDC), reveals ultrastructural morphology exhibited by coronaviruses. Note the spikes that adorn the outer surface of the virus, which impart the look of a corona surrounding the virion, when viewed electron microscopically [2].
Image courtesy.
Released by CDC/Alissa Eckert & Dan Higgins https://phil.cdc.gov/Details.aspx?pid=23311
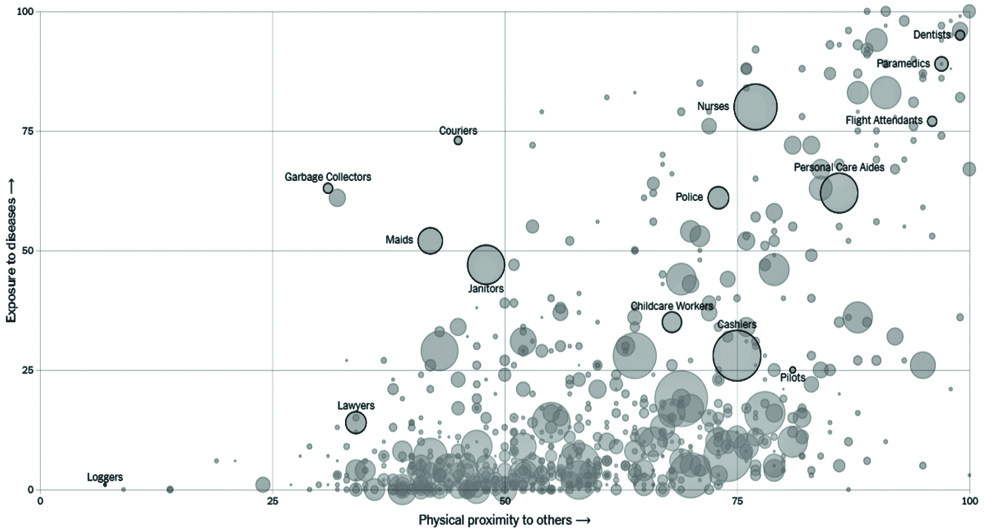
The diagnosis of COVID-19 can be made according to regulations and provisions of WHO with combined with epidemiological case history (travel history within 14 days), Clinical symptoms, Laboratory tests (Reverse Transcriptase Polymerase Chain Reaction- RT-PCR), CT imaging findings [10]. On 15 March 2020, the New York Times published an article entitled “The Workers Who Face the Greatest Coronavirus Risk”, where an striking schematic figure described that dentists are at greater risk of being affected by COVID-19 [Table/Fig-2] [11]. Dental Healthcare Personnel (DHCP) poses high risk for pneumonial infection due to the exclusive characteristics of the dental procedures such as direct communications with patient’s oro-pharyngeal region (including saliva and blood), handling of sharp equipments and most importantly aerosol generation [12,13]. This increases the probability that the DHCP’s might encounter asymptomatic COVID-19 infected patients because of the longer incubation period leading to development of only mild symptoms and they might treat those patients unknowingly, therefore, each and every one must be taken into consideration as likely to be infected by the coronavirus [12].
Image courtesy- NYT article: The Workers Who Face the Greatest Coronavirus Risk (11) and can be accessed on https://www.nytimes.com/interactive/2020/03/15/business/economy/coronavirus-worker-risk.html.
Adherence to standard preventive protocols during day-to-day clinical work won’t be as efficacious to prevent the spread. Keeping in mind the evolvement of this novel coronavirus and potential risk of cross infection, the dental health care professionals should make themselves aware and prepared for handling such disease, otherwise can be life-threatening. As suggested by American Dental Association, elective dental care should be deferred and only emergency care must be focused which will lead to drastic fall in interpersonal contact [14]. Therefore, it is of the utmost importance for dentists to adopt new preventive and extra-protective strategies and also upgrade the infection control policies, engineering control and supplies to avoid the COVID-19 infection [12,14]. Dental professionals must be aware and up-to-date about this progressing dreadful disease.
Prevention and Recommended Management Protocols for Dental Health Care Professionals
Patient EvaluationTele-screening and triaging: Whenever the appointments are scheduled, COVID-19 suspected patients should be initially screened telephonically. The patients must be asked for history of travel to COVID-19 affected areas and symptoms showing respiratory illness. If patient response is positive to any of the above two questions, then the elective care should be procrastinated for the next 2-3 weeks and patient should be encouraged to self-quarantine immediately and refer to local health department if necessary [10,15].
Upon arrival of the patient in dental setting:The patient should follow appropriate social distancing at least 6 feet/2 meters from each other in the waiting area [16].
Measuring the body temperature of every patient with the contact free infrared forehead thermometer is advised [13].
The patient should be provided with alcohol-based hand rub and surgical or face mask [17].
The patients should be educated for the respiratory hygiene/cough etiquette. Patients must be encouraged to use disposable tissues or handkerchiefs while coughing or sneezing and immediately discard into no-touch receptacles for disposal available at the health care facility entrance [18].
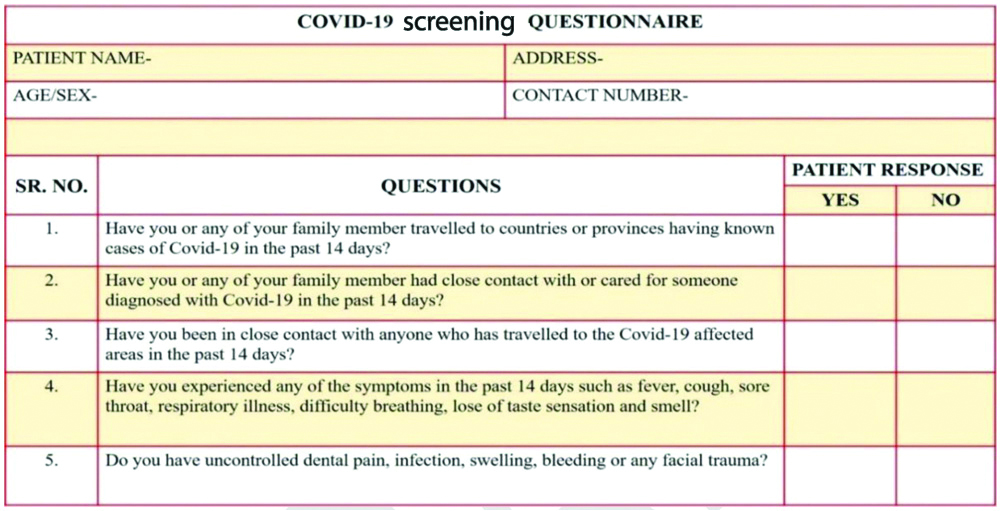
Complete medical history form and screening questionnaire must be filled by the patient before undergoing any procedure and after that; questionnaire must be assessed by the dentist [Table/Fig-3].
COVID-19 Screening questionnaire.
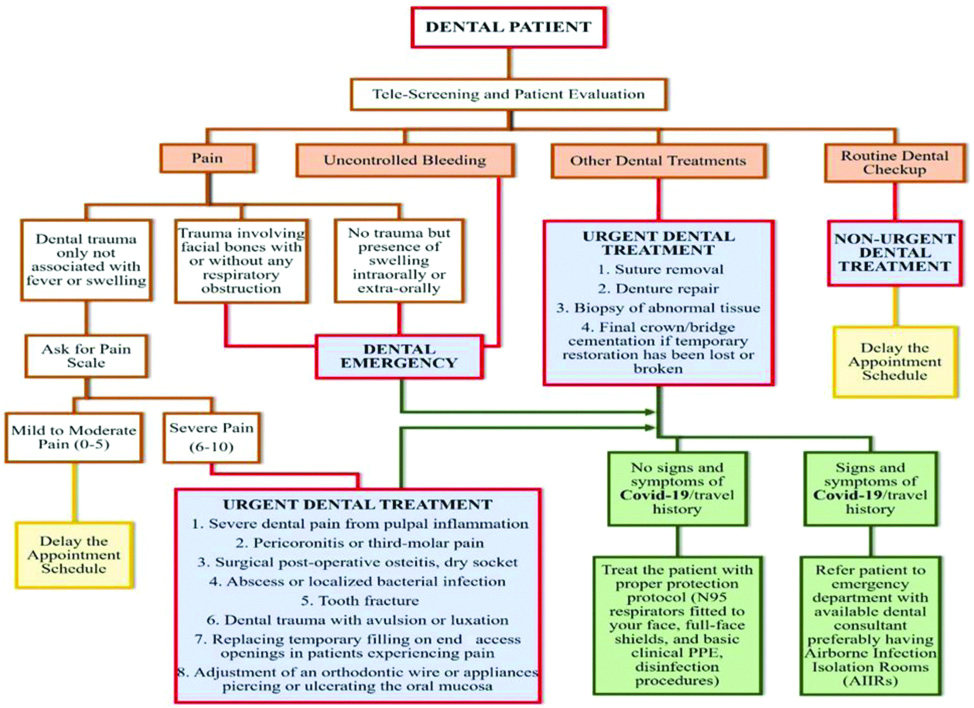
Only after proper assessment, dentist should proceed with the treatment [Table/Fig-4].
An overview of patient screening for COVID-19 and dental management.
Patients with a resolved COVID-19 infection can be seen in a dental setting: At least 3 days (72 hours) since COVID-19 infection symptoms resolved or at least 7 days since their symptoms first appeared (defined as resolution of fever without the use of fever-reducing medications and improvement in respiratory symptoms).
Precautions Before Dental CareHealth care workers who are directly or indirectly engaged in the care of confirmed or suspected patients of coronavirus are recommended to take Hydroxychloroquine as a prophylaxis of COVID-19 infection. Recommended dose- 400 mg two times a day on first day followed by 400 mg once a week for next consecutive 7 weeks [19].
DHCP’s experiencing influenza like illness should be encouraged to stay home.
Self-monitoring to any of the respiratory symptoms and temperature check is must for DHCP’s.
Dental staff should be encouraged to maintain respiratory etiquette and hand hygiene practices [18].
Place the signage in the waiting area for instructing the patient about respiratory hygiene/cough etiquette and social disinfectant.
Remove the magazines, reading material, toys and other objects from the waiting area in order to avoid being touched by anybody.
While scheduling the appointments, there should be enough time interval to reduce the possible contact of the patients with each other in the waiting area.
The standard precautions for the DHCP’s includes hand hygiene practices, Personal Protective Equipment (PPE), cough etiquette/respiratory hygiene, safe injection practices, proper sterilisation of devices and instruments, disinfection of all environmental surfaces [20].
Transmission-Based preventive measures include: placement of patient in isolation, adequately ventilated room, respiratory protection aided by N-95 masks [20].
Guidelines by Centers for Disease Control and Prevention recommended for donning and doffing of PPE [21].
Moreover, if you ever suspect a COVID-19 patient at your clinic then you must immediately contact your local health for preventing any transmission to DHCP’s or other patients.
Only the dental patients should be allowed in the dental care units, not the companions until or unless patient requires assistance especially in case of elderly patients, paediatric patients and patient with special needs.
Precautions during Dental Care
DHCP’s should follow the minimum infection prevention protocols in any dental healthcare setting, irrespective of suspected or confirmed COVID-19 patient.
Only essential health care workers (dentists and assistants) must be in the dental chair settings and that too wearing entire PPE. Any accompanying person with the patient should not be allowed in the dental operatory.
Preprocedural mouth rinse using 0.2% povidone or 1.5% hydrogen peroxide is recommended to minimise the salivary load of oral microbes as SARS-CoV-2 is vulnerable to oxidation [12,13].
Extraoral dental radiographs such as Panaromic radiograph or Cone Beam Computed Tomography (CBCT) must be preferred as the alternative to Intraoral Periapical (IOPA) Radiographs to avoid stimulation of salivary secretion and coughing. Whenever IOPA is mandatory, imaging sensors must be double barriered for avoiding any perforation and risk of cross-infection [22].
Whenever possible, disposable devices like examination instruments, syringes and blood pressure cuff must be preferred.
Use of hand-instrumentation is prioritised instead of ultrasonic instrumentation if necessary.
Minimisation of the use of a 3-in-1 syringe and high-speed handpieces are recommended to reduce the aerosol production.
Use of anti-retraction dental handpieces with anti-retractive valves is strictly advised for additional protection against cross contamination [23].
Any aerosol generating procedures if necessary, should be performed in good ventilated room preferably Airborne Infection Isolation Rooms (AIIR’s) [24].
While performing aerosol generating procedure use of rubber dam should be preferred in order to minimise the saliva and blood contaminated aerosol or spatter generation [25].
DHCP should prefer 4-handed dentistry to avoid infection.
Use of high-volume evacuators is preferred.
Resorbable sutures should be preferred to avoid the follow-up appointment.
Precautions after Dental CareBetween every patient, perform hand hygiene practice, clean PPE with soap and water, clean and disinfect reusable facial protective equipment.
The reusable instruments should be pre-treated, cleaned, sterilised and properly stored.
Non-autoclavable equipment’s such as dental chair, light and X-ray unit should be prioritised for disinfection.
Non-disposable equipment’s such as handpieces should be swiped to get rid of debris, followed by autoclaving by the method of heat-sterilisation between every patient.
Patient care areas, handles of doors, elevators, stools and washrooms must be disinfected frequently as it has been reported that virus remains viable on the inanimate surfaces up to 9 days [6].
The medical waste along with disposable PPE must be transferred to the provisional storage area [13].
Pharmacological Management
The patients who are in need for urgent dental assistance with complain of irreversible pulpitis, tooth fracture, intraoral or extraoral swelling, luxation/avulsion [26], pharmacologic approach in the form of antibiotics (Amoxycillin 500 mg or Metronidazole 400 mg three times/day) and analgesics (Paracetamol 500 mg or Diclofenac 50 mg or combination of both twice a day) is a substitute which would offer symptomatic relief to the patients [27,28].
Conclusion(s)
In conclusion, due to this drastic intervention of the life-threatening disease, it is the first most priority of the health care professionals for the protection and betterment of the natives and to curb the rapidly spreading disease. Therefore, until a vaccine or a drug becomes available, the policies and other protective and preventive measures adopted by the government are directed to every dental association, indicating the proper guidelines for preventing and controlling SARS-CoV-2 infection in daily practice.
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? NA
Was informed consent obtained from the subjects involved in the study? NA
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 21, 2020
Manual Googling: Jun 26, 2020
iThenticate Software: Aug 10, 2020 (12%)
[1]. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Early transmission dynamics in wuhan, china, of novel coronavirus-infected pneumoniaN Engl J Med 2020 382:1199-207.10.1056/NEJMoa200131631995857 [Google Scholar] [CrossRef] [PubMed]
[2]. Centers for Disease Control and Prevention: Public Health Image Library (PHIL). Available from: https://phil.cdc.gov/Details.aspx?pid=23311. Accessed 5 April 2020 [Google Scholar]
[3]. Centers for Disease Control and Prevention: Transmission of coronavirus disease 2019 (COVID-19). Available from: https://www.cdc.gov/coronavirus/2019-ncov/about/transmission.html. Accessed 11 April 2020 [Google Scholar]
[4]. Cleveland JL, Gray SK, Harte JA, Robison VA, Moorman AC, Gooch BF, Transmission of blood-borne pathogens in US dental health care settings: 2016 updateJ Am Dent Assoc 2016 147(9):729-38.10.1016/j.adaj.2016.03.02027233680 [Google Scholar] [CrossRef] [PubMed]
[5]. Sabino-Silva R, Jardim ACG, Siqueira WL, Coronavirus COVID-19 impacts to dentistry and potential salivary diagnosisClin Oral Investig 2020 24:1619-21.10.1007/s00784-020-03248-x32078048 [Google Scholar] [CrossRef] [PubMed]
[6]. Kampf G, Todt D, Pfaender S, Steinmann E, Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agentsJ Hosp Infect 2020 104(3):P246-251.10.1016/j.jhin.2020.01.02232035997 [Google Scholar] [CrossRef] [PubMed]
[7]. Zhang J, Wang S, Xue Y, Fecal specimen diagnosis 2019 novel coronavirus-infected pneumonia [Epub ahead of print]J Med Virol 2020 92(6):529-697.Accessed 12 April 202010.1002/jmv.2574232124995 [Google Scholar] [CrossRef] [PubMed]
[8]. Backer JA, Klinkenberg D, Wallinga J, Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20-28 January 2020Euro Surveill 2020 25(5):200006210.2807/1560-7917.ES.2020.25.5.200006232046819 [Google Scholar] [CrossRef] [PubMed]
[9]. Centers for Disease Control and Prevention: Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19). Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html. Accessed 12 April 2020 [Google Scholar]
[10]. World Health Organisation 2020: Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: interim guidance. Available from: https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected. Accessed 14 April 2020 [Google Scholar]
[11]. The workers who face the greatest coronavirus risk: The New York Times (New York). March 15, 2020. Available from: https://www.nytimes.com/interactive/2020/03/15/business/economy/coronavirus-worker-risk.html. Accessed 8 April 2020 [Google Scholar]
[12]. Ather A, Patel B, Ruparel NB, Diogenes A, Hargreaves KM, Coronavirus Disease 19 (COVID-19): Implications for Clinical Dental Care [Epub ahead of print]J Endod 2020 46(5):584-95.Accessed 10 April 202010.1016/j.joen.2020.03.00832273156 [Google Scholar] [CrossRef] [PubMed]
[13]. Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B, Transmission routes of 2019-nCoV and controls in dental practiceInt J Oral Sci 2020 12:910.1038/s41368-020-0075-932127517 [Google Scholar] [CrossRef] [PubMed]
[14]. ADA recommending dentists postpone elective procedures. Available from: https://www.ada.org/en/publications/ada-news/2020-archive/march/ada-recommending-dentists-postpone-elective-procedures. Accessed 14 April 2020 [Google Scholar]
[15]. Wang Y, Wang Y, Chen Y, Qin Q, Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures [Epub ahead of print]J Med Virol 2020 92(6):568-76.Accessed 14 April 202010.1002/jmv.2574832134116 [Google Scholar] [CrossRef] [PubMed]
[16]. Parhizkar A, Shamszadeh S, Mardani M, Asgary S, Dental ... Coronavirus disease: A review of literature [Epub ahead of print]Arch Clin Infect DisAccessed 16 April 2020;15(2)10.5812/archcid.103257 [Google Scholar] [CrossRef]
[17]. Bocchetti C, Sorrentino R, Cozzolino F, COVID-19: Dentistry and the new Coronavirus, a compilation from PubMed resourcesAvailable from: https://www.zerodonto.com/en/2020/03/covid-19-dentistry-new-coronavirus/. Accessed 14 April 2020 [Google Scholar]
[18]. Centers for Disease Control and Prevention: Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Accessed 14 April 2020 [Google Scholar]
[19]. Indian Council of Medical Research: Recommendation for empiric use of hydroxy-chloroquine for prophylaxis of SARS-CoV-2 infection. Available from: https://icmr.nic.in/sites/default/files/upload_documents/HCQ_Recommendation_22March_final_MM_V2.pdf. Accessed 17 April 2020 [Google Scholar]
[20]. American Dental Association: Interim Guidance for Minimising Risk of COVID-19 Transmission. Available from: https://www.ada.org/en/publications/ada-news/2020-archive/april/ada-releases-interim-guidance-on-minimising-covid-19-transmission-risk-when-treating-emergencies Accessed 15 April 2020 [Google Scholar]
[21]. Centers for Disease Control and Prevention: Healthcare Associated Infections (HAI)- Preventing HAIs. Available from: https://www.cdc.gov/hai/pdfs/ppe/ppe-sequence.pdf. Accessed 15 April 2020 [Google Scholar]
[22]. Meng L, Hua F, Bian Z, Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral MedicineJ Dent Res 2020 99(5):481-87.10.1177/002203452091424632162995 [Google Scholar] [CrossRef] [PubMed]
[23]. Spagnuolo G, De Vito D, Rengo S, Tatullo M, COVID-19 Outbreak: An Overview on DentistryInt J Environ Res Public Health 2020 17(6):209410.3390/ijerph1706209432235685 [Google Scholar] [CrossRef] [PubMed]
[24]. Occupational Safety and Health Administration: Guidance on Preparing Workplaces for COVID-19. Available from: https://www.osha.gov/Publications/OSHA3990.pdf. Accessed 15 April 2020 [Google Scholar]
[25]. Samaranayake LP, Reid J, Evans D, The efficacy of rubber dam isolation in reducing atmospheric bacterial contaminationASDC J Dent Child 1989 56(6):442-44. [Google Scholar]
[26]. American Dental Association: Interim Guidance for Management of Emergency and Urgent Dental Care. Available from: https://www.ada.org/~/media/CPS/Files/COVID/ADA_Int_Guidance_Mgmt_Emerg-Urg_Dental_COVID19. Accessed 17 April 2020 [Google Scholar]
[27]. Scottish Dental Clinical Effectiveness Programme (SDCEP): Management of Acute Dental Problems During COVID-19 Pandemic. March 2020. Available from: http://www.sdcep.org.uk/wp-content/uploads/2020/03/SDCEP-MADP-COVID-19-guide-300320.pdf. Accessed 18 April 2020 [Google Scholar]
[28]. Scottish Dental Clinical Effectiveness Programme (SDCEP): Drugs for the Management of Dental Problems During COVID-19 Pandemic. April 2020. Available from: http://www.sdcep.org.uk/wp-content/uploads/2020/04/SDCEP-MADP-COVID-19-drug-supplement-080420.pdf. Accessed 18 April 2020 [Google Scholar]