Spinal anaesthesia is the preferred method of anaesthesia for surgeries on the lower half of the body. This is due to its efficacy and rapid onset of action. Moreover, it is easy to perform and provides reliable surgical anaesthesia and muscle relaxation using a single drug. It also reduces blood loss and protects against thromboembolic complications. It is valuable in patients with a full stomach as it protects against pulmonary aspiration and is especially useful in patients with pulmonary disease. It’s chief drawback is the limited duration of postoperative analgesia. Post analgesia may be achieved by systemic analgesics, peripheral nerve blocks, local infiltration of local anaesthetics, etc. However, if a patient receives a spinal block the addition of another drug intrathecally, that will increase the duration of analgesia is the logical choice. Spinal opiates can provide profound postoperative analgesia with fewer systemic adverse effects than that with systemic opiates. Morphine [1-4] has been the gold standard of the opiates, however the side effects of respiratory depression, vomiting, pruritus has led to search of other adjuvants.
The present study was done to focus on intrathecal augmentation techniques that circumvent the need for additional intravenous agents and their consequential side effects. Also, unlike other studies, in this study, low doses of the adjuvant clonidine (30 mcg) and morphine (100 mg) were selected for comparison in intrathecal anaesthesia.
The primary aim was to compare Morphine and Clonidine as adjuncts to bupivacaine in spinal anaesthesia in terms of:
The secondary aim was to study and compare the haemodynamic stability, sedation, intraoperative and postoperative complications of both the adjuvants.
Materials and Methods
It was a double-blind randomised controlled study conducted at Goa Medical College during the year 2012-2015. Sample size was 100 and was estimated using G*Power 3 taking a power of 80 and alpha of 0.05. Approval of Study documents submitted, given by Institutional Ethics Committee, Goa Medical College on 13/2/2014.
Inclusion criteria
Patients aged between 20-40 years
ASA Grade 1 and 2
Types of surgeries: Lower limb orthopaedic surgeries such as Fracture femur, Fracture tibia, Fracture tibia and fibula, Fracture femur and tibia, Fracture ankle and Crush injury foot.
Exclusion criteria
The patients with raised intracranial pressure, coagulopathy and skin infection at the site of administration of subarachnoid block were excluded from the study.
After obtaining informed written consent, complete and thorough pre-anaesthetic check-up was done. Relevant investigations were done. Patients were explained in detail about Visual Analogue Scale (VAS) and how to interpret it. Patients were kept nil by mouth for at least 6 hours prior to surgery.
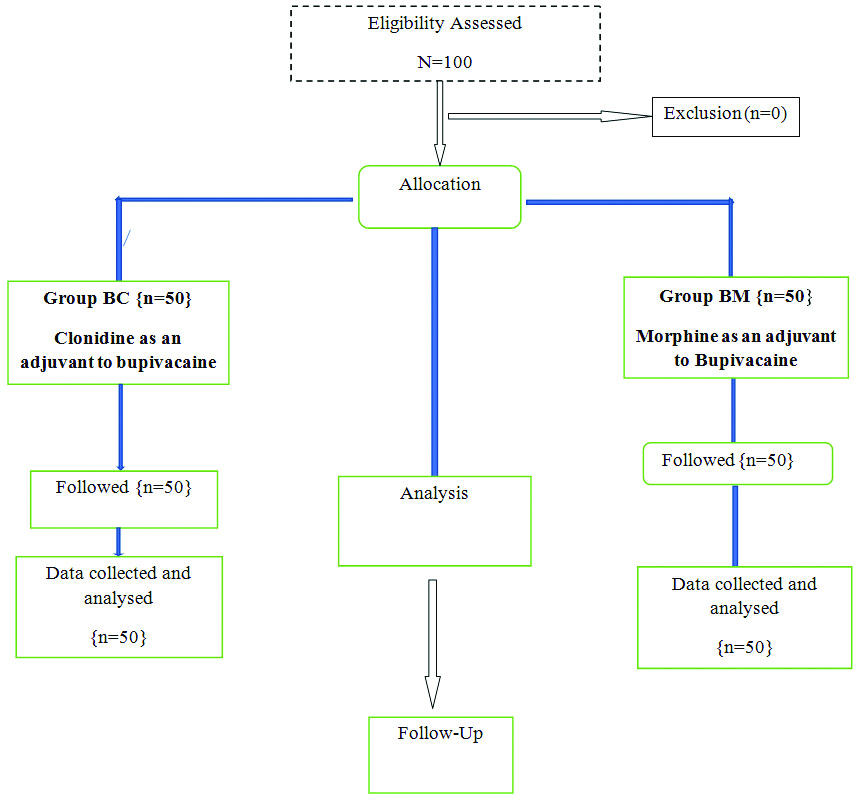
The patients were randomised using sealed opaque envelopes, into two groups (Group BM and Group BC) of 50 each as shown in flowchart [Table/Fig-1], who received the following medications intrathecally:
Group BM received a mixture of 2.6 mL (13 mg) of hyperbaric bupivacaine (0.5%) with 0.1 mL of preservative free Morphine (100 mcg) [1-4] and 0.1 mL 0.9% saline. Group BC received a mixture of 2.6 mL (13 mg) of hyperbaric-bupivacaine (0.5%) with 0.2 mL of clonidine (30 mcg) [5-10]. Total volume of solution in both the groups was 2.8 mL.
Preoperative preparation was done. Anaesthesia machine was checked. Advanced equipments and drugs for resuscitation, airway management and ventilation were kept ready. Patient’s baseline vitals were maintained. No Sedation/analgesic or any premedication was given to any of the patients.
The anaesthesiologist who administered the block, monitored the patient intraoperatively and postoperatively and was blinded to the composition of the drug that was given. After the block was administered: the heart rate, noninvasive blood pressure, oxygen saturation, respiratory rate and sedation score were recorded at regular intervals intraoperatively and postoperatively.
In case of any respiratory depression, oxygen was administered via face mask at the rate of 6 litres/minute. Respiratory depression was defined as a respiratory rate of <10 breaths/minute and hypoxia was defined as an oxygen saturation of <95%. Hypotension was defined as a fall in systolic blood pressure by >30% of baseline value and was managed with IV fluid boluses and IV ephedrine 6 mg increments. Bradycardia was defined as a fall in heart rate by >30% of baseline value and was treated with IV atropine 0.6 mg. Effects of the block were assessed as follows:
Sensory level
The sensory level was tested by pin-prick method and the highest dermatomal level of sensory blockade was noted. The time taken to achieve the highest sensory level was also noted, which was defined as the time from injection of the intrathecal drug to the loss of pin-prick sensation at the highest dermatome.
Motor blockade
Motor Blockade was assessed by modified Bromage Scale [12]. A Bromage Scale of 3 was considered as complete paralysis. A Bromage Scale of less than 3 was considered incomplete paralysis.
The patient’s level of sedation, following administration of the subarachnoid block was assessed using a sedation score [13]:
Sedation score
0- Wide awake
1- Sleeps comfortably, but responds to verbal commands
2- Deep sleep, but arousable
3- Not arousable
A sedation score of 3 was defined to be excessive sedation. Surgery was allowed to commence once the sensory level adequate for the surgery.
The duration of sensory blockade was defined as the time from intrathecal injection of the drug to the time taken for sensory level to regress to L5-S1 dermatome which was checked by pin-prick sensation over the nonoperated leg.
The duration of motor blockade was defined as the time from intrathecal injection of the drug to the time when the patient could lift the nonoperated leg with full flexion at hips and knees (Bromage scale 0).
Postoperatively, the duration of analgesia was assessed by VAS. It was elicited by a handwritten marking on a line measuring 10 cm (0 mark-No pain and 10 mark-worst possible pain).
The duration of analgesia was defined as the time from intrathecal injection of the drug to the time of administration of the rescue analgesic at a VAS of 3 or more. In the postoperative period, no analgesics were administered till the patient had VAS of 3. Thereafter, rescue analgesia was given with IV Tramadol 100 mg.
Patients were followed-up for 24 hours after administration of the subarachnoid block. Monitoring was continued in the postoperative period at regular intervals including for side effects namely respiratory depression, Postoperative Nausea and Vomiting (PNOV), excessive sedation and urinary retention.
Statistical Analysis
It was performed using Statistical Package for the Social Sciences (SPSS) software version 14. Results on continuous data are presented in mean and standard deviation and results on categorical data are presented in total number and as percentage. Student unpaired t-test has been used to find the significance of study parameters on continuous scale between the two groups (inter group analysis). The statistical significance of demographic data i.e., age, height, weight, duration of surgery, time taken to achieve the highest level of sensory blockade, duration of sensory blockade, duration of motor blockade, duration of analgesia and number of doses of rescue analgesics were evaluated by student t-test. The Pearson chi-square test was used to assess the statistical significance in the gender distribution, ASA status, type of surgery, highest level attained and adverse effects. The repeated measure ANOVA was used to assess statistical significance between groups with regard to heart rate and blood pressure saturation and respiratory rate. The p-value <0.05 was considered statistically significant.
Results
In this study, there were 29 males and 21 females in group BC and 28 males and 22 females in group BM. [Table/Fig-2] showed that the demographic features of both the groups were similar.
Patient demographic details.
| Parameters | Group BC | Group BM | p-value |
|---|
| Mean age (year) | 31.58±5.49 | 30.2±4.10 | 0.158 |
| Mean weight (kg) | 62.2±5.4 | 63.64±5.26 | 0.181 |
| Mean Height (cm) | 163.06±5.07 | 162.46±5.38 | 0.567 |
<0.05 statistically significant
The [Table/Fig-3] shows that the two groups were similar in terms of surgery, as per Pearson’s chi-square test which showed p-value of 0.33.
| Surgery | Group BC | Group BM |
|---|
| Fracture Femur | 15 (30%) | 13 (26%) |
| Fracture Ankle | 5 (10%) | 3 (6%) |
| Fracture Tibia | 13 (26%) | 14 (28%) |
| Fracture Tibia+Fibula | 7 (14%) | 10 (20%) |
| Fracture Femur+Tibia | 5 (10%) | 4 (8%) |
| Crush Injury Foot | 5 (10%) | 6 (12%) |
[Table/Fig-4a] shows that the time taken to achieve highest sensory level was lesser in Group BC than Group BM. The p-value=0.002 (<0.05). [Table/Fig-4b] shows that the extent of sensory blockade was clinically similar in both groups. The highest level was T6 and lowest, T10. [Table/Fig-4c] shows that the p-values for the duration of onset was 0.002 (<0.05) and hence, statistically significant. The highest sensory block was achieved faster in Group BC compared to Group BM.
Sensory Blockade. Time taken for highest sensory level.
| Time taken for highest sensory level | Group BC | Group BM |
|---|
| Duration (min) (Mean±Standard deviation) | 6.64±1.40 | 7.38±1.46 |
Highest sensory level attained.
| Dermatomal level | Group BC | Group BM |
|---|
| T6 | 6 (12%) | 4 (8%) |
| T8 | 31 (62%) | 32 (64%) |
| T10 | 13 (26%) | 14 (28%) |
Duration of sensory block.
| Duration of sensory block | Duration (Min.) (Mean±Standard deviation) |
|---|
| Group BC | 336.5±30.07 |
| Group BM | 214.4±23.83 |
[Table/Fig-5] shows that duration of motor block was higher in Group BC than Group BM. The p-value=<0.001 [11]. The duration of analgesia was defined as the time from intrathecal injection of the drug to the time of administration of the rescue analgesic at a VAS of 3 or more. The [Table/Fig-6] shows that the duration of analgesia was prolonged in Group BM and was statistically significant (p-value<0.05).
Motor Blockade: All the patients in both the groups had complete motor blockade {modified Bromage scale [11]}.
| Groups | Duration (Min) (Mean±Standard deviation) |
|---|
| Group BC | 308.4±29.30 |
| Group BM | 187.2±27.40 |
| Groups | Duration (Min) (Mean±Standard deviation) |
|---|
| Group BC | 427.4±25.13 |
| Group BM | 691.2±86.51 |
| p-value | <0.05 |
<0.05 statistically significant
The following [Table/Fig-7a,b and c] show that the changes in mean heart rate, systolic blood pressure and diastolic blood pressure, had significant differences within the same group (p-value <0.05), limited to the intraoperative period and were medically managed.
Comparison of changes in heart rate.
| Group BC | Group BM |
|---|
| Heart rate/min | Group BC Mean | n | Std. deviation | p-value | Group BM Mean | n | Std. deviation | p-value |
|---|
| 0 min | 82.72 | 50 | 6.524803539 | nil | 82.4 | 50 | 6.79735843 | nil |
| 2 min | 81.28 | 50 | 5.824087911 | 0.007 | 81 | 50 | 6.05080531 | 0.008 |
| 4 min | 79.48 | 50 | 6.098644881 | <0.05 | 79.16 | 50 | 6.221621286 | <0.05 |
| 6 min | 76.16 | 50 | 8.298905755 | <0.05 | 75.88 | 50 | 8.284827539 | <0.05 |
| 10 min | 73.88 | 50 | 7.932470084 | <0.05 | 73.72 | 50 | 7.803819055 | <0.05 |
| 15 min | 72.64 | 50 | 11.56659511 | <0.05 | 72.24 | 50 | 11.44027972 | <0.05 |
| 20 min | 75.32 | 50 | 9.869433332 | <0.05 | 75.4 | 50 | 9.758303633 | <0.05 |
| 30 min | 75.64 | 50 | 9.886622584 | <0.05 | 75.72 | 50 | 9.798042287 | <0.05 |
| 40 min | 79.76 | 50 | 8.306771273 | 0.012 | 79.76 | 50 | 8.277237043 | 0.017 |
| 50 min | 80.36 | 50 | 8.700832707 | 0.108 | 80.16 | 50 | 9.015542136 | 0.122 |
| 1 h | 80.12 | 50 | 8.235413822 | 0.030 | 80.32 | 50 | 8.094946773 | 0.078 |
| 1.5 h | 81.56 | 50 | 6.430666325 | 0.223 | 81.64 | 50 | 6.359181054 | 0.420 |
| 2 h | 82 | 50 | 6.246631745 | 0.472 | 82.12 | 50 | 6.106670826 | 0.773 |
| 2.5 h | 81.96 | 50 | 5.473349159 | 0.435 | 81.96 | 50 | 5.473349159 | 0.659 |
| 3 h | 81.56 | 50 | 5.969856252 | 0.303 | 81.52 | 50 | 5.918631943 | 0.444 |
| 4 h | 81.02 | 50 | 6.409463666 | 0.148 | 80.9 | 50 | 6.522332123 | 0.210 |
| 5 h | 81.48 | 50 | 7.371317829 | 0.278 | 81.04 | 50 | 7.551077771 | 0.240 |
| 6 h | 81.88 | 50 | 6.495335846 | 0.473 | 81.84 | 50 | 6.4755742 | 0.637 |
| 7 h | 83.08 | 50 | 6.666517005 | 0.756 | 83.28 | 50 | 6.487161575 | 0.453 |
| 8 h | 82.96 | 50 | 6.568197964 | 0.846 | 83.04 | 50 | 6.455372703 | 0.609 |
| 12 h | 82.32 | 50 | 5.441488392 | 0.723 | 82.48 | 50 | 5.245950819 | 0.945 |
| 24 h | 82.88 | 50 | 5.000571396 | 0.882 | 83.16 | 50 | 4.850247206 | 0.494 |
<0.05 statistically significant
Comparison of changes in systolic BP.
| Group BC | Group BM |
|---|
| SBP mmHg | Group BC Mean | N | Std. deviation | p-value | Group BM Mean | n | Std deviation | p-value |
|---|
| 0 min | 126.24 | 50 | 6.189391846 | nil | 126.56 | 50 | 6.061453991 | nil |
| 2 min | 126.24 | 50 | 6.149697188 | 1.000 | 126.44 | 50 | 6.105066481 | 0.888 |
| 4 min | 113.68 | 50 | 9.065386064 | <0.05 | 114.28 | 50 | 9.13401358 | <0.05 |
| 6 min | 105.88 | 50 | 6.80228053 | <0.05 | 105.76 | 50 | 6.852855803 | <0.05 |
| 10 min | 104.08 | 50 | 11.93697736 | <0.05 | 104.08 | 50 | 10.51715799 | <0.05 |
| 15 min | 104.68 | 50 | 7.489966077 | <0.05 | 104.68 | 50 | 7.489966077 | <0.05 |
| 20 min | 107.2 | 50 | 6.363159272 | <0.05 | 107.36 | 50 | 6.381606221 | <0.05 |
| 30 min | 111.12 | 50 | 5.332380867 | <0.05 | 111.32 | 50 | 5.168349517 | <0.05 |
| 40 min | 112.56 | 50 | 6.725401134 | <0.05 | 112.84 | 50 | 6.478724994 | <0.05 |
| 50 min | 114.48 | 50 | 6.572173871 | <0.05 | 114.56 | 50 | 6.565711799 | <0.05 |
| 1 h | 115 | 50 | 5.034574339 | <0.05 | 114.6 | 50 | 5.018333734 | <0.05 |
| 1.5 h | 121.96 | 50 | 7.596884431 | 0.003 | 122.36 | 50 | 7.20192718 | 0.004 |
| 2 h | 124.6 | 50 | 4.886466108 | 0.142 | 124.76 | 50 | 4.863693062 | 0.110 |
| 2.5 h | 124.72 | 50 | 6.385698306 | 0.259 | 124.52 | 50 | 6.296224978 | 0.117 |
| 3 h | 125.36 | 50 | 5.442688411 | 0.407 | 125.28 | 50 | 5.62443648 | 0.239 |
| 4 h | 124.6 | 50 | 5.514359733 | 0.181 | 124.28 | 50 | 5.436235192 | 0.054 |
| 5 h | 126.5 | 50 | 4.509626891 | 0.817 | 126.26 | 50 | 4.475830786 | 0.780 |
| 6 h | 125.92 | 50 | 9.133566708 | 0.816 | 126.08 | 50 | 9.061783399 | 0.730 |
| 7 h | 125.84 | 50 | 4.404821106 | 0.629 | 126 | 50 | 4.481253469 | 0.498 |
| 8 h | 126.76 | 50 | 5.769589523 | 0.614 | 126.88 | 50 | 5.77340843 | 0.754 |
| 12 h | 128.2 | 50 | 5.018333734 | 0.083 | 128.24 | 50 | 5.073178772 | 0.123 |
| 24 h | 125.84 | 50 | 5.726273141 | 0.644 | 126 | 50 | 5.728553616 | 0.513 |
<0.05 statistically significant
Comparison of changes in diastolic BP.
| Group BC | | Group BM |
|---|
| DBP mmHg | Group BC Mean | N | Std deviation | p-value | Group BM Mean | n | Std deviation | p-value |
|---|
| 0 min | 78.96 | 50 | 3.109957674 | nil | 78.92 | 50 | 3.409710024 | nil |
| 2 min | 78.52 | 50 | 3.227686352 | 0.117 | 78.32 | 50 | 3.43713217 | 0.062 |
| 4 min | 71.42 | 50 | 4.199562659 | <0.05 | 71.58 | 50 | 4.140836946 | <0.05 |
| 6 min | 65.08 | 50 | 5.601894723 | <0.05 | 65.2 | 50 | 5.771145679 | <0.05 |
| 10 min | 62.08 | 50 | 7.526388949 | <0.05 | 62.04 | 50 | 7.499551007 | <0.05 |
| 15 min | 62.12 | 50 | 5.305522729 | <0.05 | 62.04 | 50 | 5.134755523 | <0.05 |
| 20 min | 63.24 | 50 | 3.852166101 | <0.05 | 63.16 | 50 | 3.547692553 | <0.05 |
| 30 min | 64.28 | 50 | 4.295417587 | <0.05 | 64.32 | 50 | 3.798173568 | <0.05 |
| 40 min | 66.84 | 50 | 4.730966161 | <0.05 | 66.84 | 50 | 4.643889995 | <0.05 |
| 50 min | 69.04 | 50 | 3.795593578 | <0.05 | 68.8 | 50 | 3.854496447 | <0.05 |
| 1 h | 69.56 | 50 | 4.126371139 | <0.05 | 69.24 | 50 | 4.312109196 | <0.05 |
| 1.5 h | 77.48 | 50 | 3.072192596 | 0.011 | 77.64 | 50 | 2.932993178 | 0.036 |
| 2 h | 78.04 | 50 | 2.372977119 | 0.089 | 78 | 50 | 2.356060357 | 0.111 |
| 2.5 h | 78.32 | 50 | 2.189399321 | 0.255 | 78.28 | 50 | 2.213502166 | 0.290 |
| 3 h | 78.24 | 50 | 2.93160122 | 0.231 | 78.04 | 50 | 2.98267104 | 0.156 |
| 4 h | 77.68 | 50 | 2.780691442 | 0.029 | 77.84 | 50 | 2.67535998 | 0.085 |
| 5 h | 77.8 | 50 | 3.213491965 | 0.057 | 77.96 | 50 | 3.116512965 | 0.137 |
| 6 h | 78.12 | 50 | 2.692696092 | 0.146 | 78.2 | 50 | 2.563479778 | 0.237 |
| 7 h | 78.44 | 50 | 3.239803471 | 0.419 | 78.48 | 50 | 3.092056973 | 0.508 |
| 8 h | 78.44 | 50 | 2.865416592 | 0.322 | 78.4 | 50 | 2.828427125 | 0.360 |
| 12 h | 78.88 | 50 | 2.291421446 | 0.890 | 78.76 | 50 | 2.317282011 | 0.795 |
| 24 h | 78.88 | 50 | 2.774813838 | 0.888 | 78.88 | 50 | 2.715338142 | 0.945 |
<0.05 statistically significant
[Table/Fig-7d,e] show that there was no significant change in respiratory rate and peripheral oxygen saturation (p-value >0.05).
Comparison of changes in respiratory rate.
| Group BC | Group BM |
|---|
| Resp. rate | Group BC Mean | n | Std. deviation | p-value | Group BM Mean | n | Std. deviation | p-value |
|---|
| 0 min | 12.52 | 50 | 0.886174995 | nil | 12.48 | 50 | 0.862838221 | nil |
| 2 min | 12.64 | 50 | 1.005292119 | 0.466 | 12.6 | 50 | 0.989743319 | 0.436 |
| 4 min | 12.46 | 50 | 0.885483841 | 0.583 | 12.42 | 50 | 0.859283042 | 0.518 |
| 6 min | 12.44 | 50 | 0.860943953 | 0.438 | 12.44 | 50 | 0.860943953 | 0.674 |
| 10 min | 12.48 | 50 | 0.862838221 | 0.659 | 12.44 | 50 | 0.836903915 | 0.659 |
| 15 min | 12.2 | 50 | 0.670059394 | 0.059 | 12.2 | 50 | 0.670059394 | 0.099 |
| 20 min | 12.18 | 50 | 0.660550173 | 0.049 | 12.18 | 50 | 0.660550173 | 0.075 |
| 30 min | 12.24 | 50 | 0.624663175 | 0.095 | 12.2 | 50 | 0.571428571 | 0.075 |
| 40 min | 12.24 | 50 | 0.656521445 | 0.090 | 12.2 | 50 | 0.606091527 | 0.090 |
| 50 min | 12.5 | 50 | 0.814411018 | 0.871 | 12.5 | 50 | 0.814411018 | 0.864 |
| 1 h | 12.64 | 50 | 0.942424143 | 0.348 | 12.56 | 50 | 0.907114735 | 0.510 |
| 1.5 h | 12.56 | 50 | 0.884330717 | 0.735 | 12.56 | 50 | 0.884330717 | 0.471 |
| 2 h | 12.48 | 50 | 0.862838221 | 0.659 | 12.4 | 50 | 0.808122036 | 0.159 |
| 2.5 h | 12.48 | 50 | 0.862838221 | 0.709 | 12.44 | 50 | 0.836903915 | 0.659 |
| 3 h | 12.58 | 50 | 0.905538514 | 0.627 | 12.54 | 50 | 0.885483841 | 0.583 |
| 4 h | 12.5 | 50 | 0.839095723 | 0.850 | 12.5 | 50 | 0.839095723 | 0.837 |
| 5 h | 12.46 | 50 | 0.813408048 | 0.537 | 12.46 | 50 | 0.813408048 | 0.821 |
| 6 h | 12.58 | 50 | 0.882713812 | 0.537 | 12.54 | 50 | 0.862128358 | 0.497 |
| 7 h | 12.4 | 50 | 0.832993128 | 0.204 | 12.4 | 50 | 0.832993128 | 0.351 |
| 8 h | 12.44 | 50 | 0.812152594 | 0.399 | 12.44 | 50 | 0.812152594 | 0.642 |
| 12 h | 12.5 | 50 | 0.863074712 | 0.855 | 12.42 | 50 | 0.810391692 | 0.472 |
| 24 h | 12.46 | 50 | 0.862128358 | 0.083 | 12.46 | 50 | 0.862128358 | 0.709 |
<0.05 statistically significant
Comparison of changes in SPO2.
| Group BC | | Group BM |
|---|
| SPO2 | Group BC Mean | n | Std. deviation | p-value | Group BM Mean | n | Std. deviation | p-value |
|---|
| 0 min | 99.12 | 50 | 0.435187035 | nil | 99.08 | 50 | 0.395897327 | nil |
| 2 min | 99.06 | 50 | 0.239897937 | 0.411 | 99.06 | 50 | 0.239897937 | 0.766 |
| 4 min | 99.06 | 50 | 0.424264069 | 0.497 | 99.06 | 50 | 0.424264069 | 0.811 |
| 6 min | 99.06 | 50 | 0.239897937 | 0.411 | 99.06 | 50 | 0.239897937 | 0.766 |
| 10 min | 99.04 | 50 | 0.197948664 | 0.209 | 99.04 | 50 | 0.197948664 | 0.485 |
| 15 min | 99.02 | 50 | 0.377424138 | 0.168 | 99 | 50 | 0.349927106 | 0.252 |
| 20 min | 99.08 | 50 | 0.274047516 | 0.533 | 99.06 | 50 | 0.239897937 | 0.743 |
| 30 min | 99.04 | 50 | 0.197948664 | 0.252 | 99.04 | 50 | 0.197948664 | 0.533 |
| 40 min | 99.04 | 50 | 0.282842712 | 0.290 | 99.04 | 50 | 0.282842712 | 0.569 |
| 50 min | 99.08 | 50 | 0.274047516 | 0.598 | 99.08 | 50 | 0.274047516 | 1.000 |
| 1 h | 99.04 | 50 | 0.197948664 | 0.252 | 99.04 | 50 | 0.197948664 | 0.533 |
| 1.5 h | 99.04 | 50 | 0.197948664 | 0.290 | 99.04 | 50 | 0.197948664 | 0.569 |
| 2 h | 99.06 | 50 | 0.239897937 | 0.411 | 99.06 | 50 | 0.239897937 | 0.766 |
| 2.5 h | 99.08 | 50 | 0.274047516 | 0.533 | 99.06 | 50 | 0.239897937 | 0.743 |
| 3 h | 99.08 | 50 | 0.274047516 | 0.569 | 99.08 | 50 | 0.274047516 | 1.000 |
| 4 h | 99.06 | 50 | 0.239897937 | 0.411 | 99.06 | 50 | 0.239897937 | 0.766 |
| 5 h | 99.02 | 50 | 0.141421356 | 0.133 | 99.02 | 50 | 0.141421356 | 0.322 |
| 6 h | 99.04 | 50 | 0.197948664 | 0.252 | 99.04 | 50 | 0.197948664 | 0.533 |
| 7 h | 99.02 | 50 | 0.141421356 | 0.133 | 99.04 | 50 | 0.197948664 | 0.533 |
| 8 h | 99.08 | 50 | 0.395897327 | 0.674 | 99.1 | 50 | 0.36421568 | 0.811 |
| 12 h | 99.08 | 50 | 0.274047516 | 0.485 | 99.06 | 50 | 0.239897937 | 0.709 |
| 24 h | 99.04 | 50 | 0.197948664 | 0.209 | 99.04 | 50 | 0.197948664 | 0.485 |
<0.05 statistically significant
In [Table/Fig-8], it was found that group BM had significantly higher sedation score than group BC (p-value <0.05).
| Sedation score | Group BC | Group BM | p-value |
|---|
| 0 | 21 (42%) | 9 (18%) | <0.05 |
| 1 | 23 (46%) | 20 (40%) |
| 2 | 6 (10%) | 21 (42%) |
| 3 | 0 | 0 |
The mean peripheral oxygen saturation was maintained in all cases perioperatively. There were no instances of hypoxia or respiratory depression. [Table/Fig-9] shows that the side effect profile between the two groups were comparable. Hypotension was treated with IV ephedrine 6 mg bolus and bradycardia was treated with 0.6 mg IV Atropine. Nausea and vomiting was treated with IV Ondanseterone 4 mg.
| Adverse effects | Group BC | Group BM | p-value |
|---|
| Bradycardia | 3 (6%) | 1 (2%) | 0.3124 |
| Hypotension | 10 (20%) | 9 (18%) | 0.799 |
| Nausea and vomiting | 3 (6%) | 8 (16%) | 0.1165 |
| Shivering | 4 (8%) | 4 (8%) | 1 |
| Respiratory depression | 0 | 0 | -- |
| Excessive sedation | 0 | 0 | -- |
| Urinary retention | 0 | 0 | -- |
| Dry mouth | 2 (4%) | 0 | 0.1595 |
| Headache | 0 | 0 | -- |
| High spinal | 0 | 0 | -- |
| Pruritis | 0 | 3 (6%) | 0.072 |
| Others | 0 | 0 | -- |
Discussion
Segmental analgesia induced by opioids and nonopiods, particularly alpha-2 agonists, when used as adjuvants to bupivacaine have been used to successfully treat both intraoperative and postoperative pain. Clonidine, a partial alpha-2 agonist is known to increase both sensory and motor block of local anaesthetics [14]. This was primarily due to stimulation of alpha-2 receptors in dorsal horn of spinal cord which reduces release of substance P [15]. Intrathecal Morphine in the dose range of 100-200 mcg has exhibited effective analgesia, especially in obstetric and orthopaedic surgeries [16,17]. The study aimed to evaluate the effect on sensory and motor block, postoperative analgesia, haemodynamics and complications of Clonidine as compared to Morphine as an adjunct to intrathecal Bupivacaine.
Sensory Block
In the study, it was observed that addition of Clonidine as compared to morphine significantly prolongs the duration of sensory block. This was in concurrence with the findings of Sethi BS et al., and Justin DM et al., which found that regression of sensory level was prolonged more with Clonidine than Morphine [11,18].
The maximal extension of the sensory blockade was T6. The upper level of sensory blockade level attained was similar in both the groups as found by Strebel S et al., [19].
Motor Block
A complete motor blockade of lower extremities was observed in all patients. This result was in concurrence with findings by Sethi BS et al., and Justin DM et al., [11,18]. The study time {mean (Standard deviation)} to regress below L4 with Clonidine (30 mcg) was 216 (97.1) minutes and with Morphine (100 mcg) was 109 (57.8) minutes, respectively.
Duration of Analgesia
Both Clonidine and Morphine when added as an adjuvant to bupivacaine in spinal anaesthesia increases the duration of analgesia is a well-known result [2,5,16,21-23]. In this study, the duration of analgesia in group BM was significantly longer.
Similar results were obtained in another study by Fogarty DJ et al., and it was observed that visual analogue scores for analgesia were significantly better in the morphine group at 2, 4, 6, 8, 10 and 12 hour after operation compared with the saline controls and significantly better than the Clonidine group from 4 to 10 hours [24]. Hence, Morphine increases the duration of spinal analgesia as compared to that of Clonidine.
In a study by Dobrydnjov I et al., time to the first rescue analgesic with 30 micrograms Clonidine with bupivacaine was 253±71 min [25]. Thus, patients receiving Morphine as adjuvant to Bupivacaine were pain free and comfortable for longer duration after surgery compared to patients receiving Bupivacaine and Clonidine.
Sedation
In this study, it was found that the group that received intrathecal Bupivacaine with morphine were more sedated, as assessed by sedation score. No patient was excessively sedated. This underlines the safety of intrathecal Clonidine and Morphine at the low doses given in this study.
Haemodynamic Parameters
There was no significant difference in heart rates, systolic and diastolic pressures between the two groups. There was no significant change in respiratory rate and peripheral oxygen saturation from baseline in both the groups (p>0.05), and supplemental oxygen or any other form of airway management was not needed. No respiratory depression was found with 100 micrograms of morphine when added as an adjunct to bupivacaine in spinal anaesthesia as found in a study by Ezzat A et al., [26].
Complications
Incidence of hypotension, bradycardia, shivering nausea and vomiting were not statistically significant. There were 2 incidences of dry mouth in Group BC and 0 in Group BM. In Group BM there were 3 incidences of pruritus and 0 In Group BC. The comparison of total number of subjects to have side-effects in both the groups had no statistical significance. This was similar result obtained in a study by Fogarty DJ et al., which states side effects were similar in all groups [24].
Limitation(s)
Limitation of study was that, the speed of injection while giving the spinal was not definite and this could have had a possible role in onset of analgesia.
Conclusion(s)
It was found that the addition of intrathecal Clonidine (30 micrograms) to bupivacaine improved the quality of the block in terms of faster onset of action and duration. However, the duration of postoperative analgesia was prolonged more when morphine (100 micrograms) was added to bupivacaine. No significant side effects were noted with the use of these adjuncts.
<0.05 statistically significant
<0.05 statistically significant
<0.05 statistically significant
<0.05 statistically significant
<0.05 statistically significant
<0.05 statistically significant
<0.05 statistically significant