Lung cancer is the most commonly diagnosed and fatal cancer annually since 1985 in the world. Worldwide, there are 2.09 million new cases of lung cancer per year, with 1.76 million deaths, making lung cancer the leading cause (18.4%) of cancer-related mortality. In India about 67,795 cases of lung cancer cases are reported annually (5.9% of total cancer cases), i.e., the fourth leading cause of cancer and the third leading cause of cancer deaths in India (8.1%) [1]. As the prognosis of lung cancer is unfavourable, early diagnosis plays an important role in increasing the survival in lung cancer patients. Early diagnosis of lung cancer can be contributed by the use of various methods. Imaging tests (chest X-ray and Computed Tomography (CT)), sputum cytology and FOB are the most commonly used methods. Currently, FOB is considered the primary method for evaluating the tracheobronchial tree in patients with suspected lung cancer [2]. Initially, endobronchial examination was carried out for the purpose of removing inhaled foreign bodies using a rigid bronchoscope with provision for suction and illumination [3]. Technologic advances facilitated development of bronchoscopy and the advent of flexible FOB, pioneered by Shigeto Ikeda in 1967, has revolutionised the diagnosis and therapeutic approach in respiratory diseases. FOB replaced the rigid, open tube bronchoscope in the diagnosis and management of inflammatory, infectious and malignant diseases of the chest [2,3]. Even though histopathological examination of bronchial biopsy specimen remains the confirmatory or the gold standard test, morphological appearance along with side and site of the lesion is also important for the diagnosis [2]. The description of endoscopic images can be subjective and bronchoscopists can encounter difficulties in describing endobronchial lesions. The studies comparing the endoscopic presentations with histopathology were less, especially in India.
Hence, the present study was done with the objectives of finding out the various endoscopic presentations of bronchogenic carcinoma in relation to side, site and morphology, their simple characterisation and co-relating these presentations with their histopathology.
Materials and Methods
This was a descriptive cross-sectional study conducted at Institute of Respiratory Diseases, SMS Medical College, Jaipur, Rajasthan, India, during the period March 2018 to May 2019 in a prospective manner after taking necessary permission from the college ethics committee (IEC no: 848/MC/IC/2019). Sample size was calculated at 95% confidence level and alpha error 0.05 assuming left bronchogenic carcinoma level 54.289% (38) as per reference article [4]. At absolute allowable error of 10%, the minimum sample size required for the study was 100.
Inclusion criteria: Patients in whom clinico-radiological findings were suggestive of lung malignancy were selected after taking informed written consent.
Exclusion criteria: Those who were acid fast bacilli or HIV positive and those having coagulation abnormalities were excluded. After applying inclusion and exclusion criteria, 122 adult patients of either sex were evaluated. Detailed history was taken and clinical examinations along with relevant investigations were done. Then the patients underwent diagnostic FOB and findings were noted carefully with regard to side, site and morphology of the lesion. The morphological findings were first classified into an endobronchial growth or a non-specific finding. The former was further classified in detail into exophytic, nodular, cauliflower, polypoidal, infiltrative and ulcerative types of growth; and the latter into external compression, secondary and/or tertiary carinal widening, ulcerative mucosa and corrugative mucosa. Endobronchial biopsy, washings and brushings were taken wherever possible and specimens were analysed by cytological and histopathological evaluation. In the cases where bronchial biopsy could not be done or when the histopathology came as inconclusive for malignancy, other invasive procedures for tissue diagnosis like CT guided biopsy, pleural biopsy or peripheral lymph node biopsy were considered in feasible cases to obtain a histopathological diagnosis. Twenty cases were excluded as a histopathological diagnosis of lung malignancy could not be made or as alternative diagnoses came out. Thus, this study was conducted in 102 diagnosed cases of primary lung malignancy. Twelve cases of lung malignancy were diagnosed by procedures other than FOB as bronchial biopsy could not be done in eight cases and came as inconclusive in four cases. Cytological samples (via bronchial wash and/or brush) were obtained in 87 cases, among which two cases were finally diagnosed by procedures other than FOB.
Statistical Analysis
The collected data were revised, coded, tabulated and introduced to a Personal Computer (PC) using IBM SPSS Statistics, Version 25.0 software. For quantitative data, mean±SD (Standard Deviation), minimum and maximum values (range) were used. For non-quantitative data, percentage was used. Qualitative variables were tested by chi-square test. The correlations were considered significant (S) when p-value was <0.05, not significant (NS) when p-value was >0.05.
Results
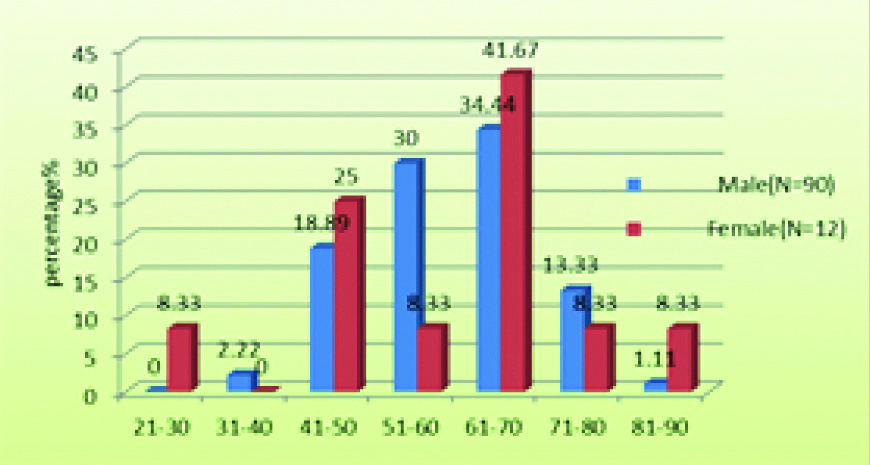
The present study was done in 102 patients {90 males (88.2%) and 12 females (11.8%)} with primary lung cancer. The study population had a mean±SD age of 59.5±11.1 years with a male to female ratio of 7.5:1 [Table/Fig-1].
Age and sex distribution of study subjects.
Of the total 102 patients, 97 patients were smokers, whereas five patients were non-smokers. The number of smokers among males and females were 89 (98.9%) and 8 (66.7%), respectively. The presenting complaints of the patients were productive cough with or without expectoration (n=77, 75.49%) followed by chest pain (n=70, 68.63%) and the most frequently observed physical sign was clubbing of fingers (n=58, 56.86%). The major roentographic findings were mass lesion (n=70, 68.63%) and pleural effusion (n=15, 14.71%); and lung mass was the most frequent finding (n=89, 87.25%) in chest CT followed by mediastinal lymph nodes (n=53, 51.96%). Among the bronchoscopic findings, 45 (44.12%) cases were on the right side, 40 (39.24%) cases were on the left side and 17 (16.67%) cases were seen bilaterally [Table/Fig-2]. The main stem bronchi were involved in maximum cases 36 (35.29%) followed by lobar bronchi 28 cases (27.45%). The left main bronchus was the most commonly involved bronchus, 22 cases (21.15%) out of the total 102 cases.
Distribution of study subjects according to side of lesion and histopathology.
| Histopathology | R | % | L | % | B/L | % | p-value |
|---|
| NSCLC-NOS (N=22) | 11 | 24.44 | 9 | 22.5 | 2 | 11.76 | 0.547 |
| SQCC (N=33) | 16 | 35.56 | 12 | 30 | 5 | 29.41 | 0.827 |
| SCC (N==19) | 7 | 15.56 | 7 | 17.5 | 5 | 29.41 | 0.445 |
| AC (N=13) | 8 | 17.78 | 4 | 10 | 1 | 5.88 | 0.365 |
| UN (N=10) | 3 | 6.67 | 4 | 10 | 3 | 17.65 | 0.431 |
| PDN (N=3) | 0 | 0 | 3 | 7.5 | 0 | 0 | 0.091 |
| NEC (N=1) | 0 | 0 | 0 | 0 | 1 | 5.88 | 0.080 |
| Lymphoma (N=1) | 0 | 0 | 1 | 2.5 | 0 | 0 | 0.457 |
| Total (N=102) | 45 | 100 | 40 | 100 | 17 | 100 | - |
R: Right; L: Left; B/L: Bilateral; NSCLC-NOS: Non-small cell carcinoma not otherwise specified; SQCC-Squamous cell carcinoma, SCC: Small cell carcinoma; AC: Adenocarcinoma; UN: Undifferentiated malignancy; PDN: Poorly differentiated neoplasm; NEC: Neuroendocrine carcinoma
SQCC was the most common type with 33 cases (32.35%) followed by Non-SCC Not Otherwise Specified (NSCLC-NOS) with 22 cases (21.57%) [Table/Fig-3]. SQCC was the most common type seen in almost equal proportions in both males and females (n=29, 32.22% and n=4, 33.33%, respectively). In females, AC was the second common histopathological type (n=3, 25%). Among smokers, SQCC was the most common type with 32 cases (32.99%) followed by NSCLC not otherwise specified 22 (22.68%). AC was the most common type of malignancy in non-smokers with 2 cases (40%).
Distribution of study subjects according to site of lesion and histopathology.
| Site | NSCLC-NOS | % | SQCC | % | SCC | % | AC | % | UN | % | OTH | % | p-value |
|---|
| T | 0 | 0 | 1 | 3.03 | 4 | 21.05 | 0 | 0 | 2 | 20 | 1 | 20 | 0.042 |
| C | 1 | 4.55 | 2 | 6.06 | 1 | 5.26 | 0 | 0 | 1 | 10 | 0 | 0 | 1.00 |
| MSB | 8 | 36.36 | 12 | 36.36 | 6 | 31.58 | 4 | 30.77 | 3 | 30 | 3 | 60 | 1.00 |
| IMB | 5 | 22.73 | 6 | 18.18 | 1 | 5.26 | 0 | 0 | 0 | 0 | 0 | 0 | 0.149 |
| ULB | 2 | 9.09 | 7 | 21.21 | 2 | 10.53 | 2 | 15.38 | 2 | 20 | 0 | 0 | 0.835 |
| MLB | 1 | 4.55 | 0 | 0 | 1 | 5.26 | 0 | 0 | 0 | 0 | 0 | 0 | 0.827 |
| LLB | 1 | 4.55 | 1 | 3.03 | 2 | 10.53 | 4 | 30.77 | 0 | 0 | 0 | 0 | 0.030 |
| SB | 3 | 13.64 | 1 | 3.03 | 2 | 10.53 | 1 | 7.69 | 1 | 10 | 1 | 20 | 0.863 |
| U&LLB | 0 | 0 | 2 | 6.06 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.591 |
| B/L ULB | 0 | 0 | 1 | 3.03 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1.00 |
| 2&/3C | 1 | 4.55 | 0 | 0 | 0 | 0 | 2 | 15.38 | 1 | 10 | 0 | 0 | 0.178 |
| Total | 22 | 100 | 33 | 100 | 19 | 100 | 13 | 100 | 10 | 100 | 5 | 100 | - |
T: Trachea; C: Main carina; MSB: Main stem bronchi; IMB: Intermediate bronchus; ULB: Upper lobe bronchi; MLB: Middle lobe bronchus; LLB: Lower lobe bronchi; SB: Segmental bronchi; U&LLB: Upper and lower lobe bronchi; B/L ULB: Bilateral ULB; 2&/3C: Secondary and/or tertiary carina; NSCLC-NOS: Non-small cell carcinoma not otherwise specified; SQCC: Squamous cell carcinoma; SCC; Small cell carcinoma; AC: Adenocarcinoma, UN: Undifferentiated malignancy; OTH: Others
Cytological examination showed malignant cells only in 30 cases (34.48%) out of the 87 cases where a cytological specimen was obtained. Among the cases which were diagnosed via procedures other than FOB (n=12), cytological specimens were obtained only in two cases and both of these cytological examination came as inconclusive.
The different histopathological types of lung cancer in relation to the bronchoscopic and morphological appearances are given in [Table/Fig-4,5]. The different endoscopic presentations is given in [Table/Fig-6].
Distribution of study subjects according to bronchoscopic appearances and histopathology.
| Type | Endobronchial growth | No growth | p-value |
|---|
| N | % | N | % | |
|---|
| SQCC | 32 | 37.21 | 1 | 6.25 | 0.032 |
| NSCLC-NOS | 18 | 20.93 | 4 | 25 | 0.082 |
| SCC | 18 | 20.93 | 1 | 6.25 | 0.02 |
| AC | 6 | 6.98 | 7 | 43.75 | 0.135 |
| PDN | 2 | 2.33 | 1 | 6.25 | 0.962 |
| NEC | 1 | 1.16 | 0 | 0 | 0.343 |
| Lymphoma | 1 | 1.16 | 0 | 0 | 0.343 |
| Undifferentiated | 8 | 9.30 | 2 | 12.5 | 0.950 |
| Total | 86 | 100 | 16 | 100 | - |
SQCC: Squamous cell carcinoma; NSCLC-NOS: Non-small cell carcinoma not otherwise specified; SCC: Small cell carcinoma; AC: Adenocarcinoma; UN: Undifferentiated malignancy; PDN: Poorly differentiated neoplasm; NEC: Neuroendocrine carcinoma
Distribution of study subjects according to detailed morphological appearance and histopathology.
| Bronchoscopic finding | NSCLC-NOS | % | SQCC | % | SCC | % | AC | % | UN | % | OTH | % | p-value |
|---|
| Exophytic growth | 11 | 50 | 21 | 63.64 | 13 | 68.42 | 5 | 38.46 | 5 | 50 | 1 | 20 | 0.041 |
| Nodular growth | 5 | 22.73 | 5 | 15.15 | 3 | 15.79 | 0 | 0 | 2 | 20 | 2 | 40 | 0.432 |
| Cauliflower growth | 1 | 4.55 | 2 | 6.06 | 1 | 5.26 | 0 | 0 | 0 | 0 | 0 | 0 | 1.00 |
| Necrotic growth | 0 | 0 | 3 | 9.09 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.292 |
| Polypoidal growth | 0 | 0 | 0 | 0 | 1 | 5.26 | 0 | 0 | 1 | 10 | 1 | 20 | 0.105 |
| Infiltrative growth | 1 | 4.55 | 0 | 0 | 0 | 0 | 1 | 7.69 | 0 | 0 | 0 | 0 | 1.000 |
| Ulcerative growth | 0 | 0 | 1 | 3.03 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.581 |
| External compression | 3 | 13.64 | 1 | 3.03 | 1 | 5.26 | 3 | 23.08 | 0 | 0 | 1 | 20 | 0.216 |
| Carinal widening | 1 | 4.55 | 0 | 0 | 0 | 0 | 2 | 15.38 | 1 | 10 | 0 | 0 | 0.178 |
| Ulcerative mucosa | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 7.69 | 1 | 10 | 0 | 0 | 0.229 |
| Corrugative mucosa | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 7.69 | 0 | 0 | 0 | 0 | 0.250 |
| Total | 22 | 100 | 33 | 100 | 19 | 100 | 13 | 100 | 10 | 100 | 5 | 100 | - |
SQCC: Squamous cell carcinoma; NSCLC-NOS: Non-small cell carcinoma not otherwise specified; SCC: Small cell carcinoma; AC: Adenocarcinoma; UN: Undifferentiated malignancy
Different endoscopic presentations: a) Exophytic growth; b) Exophytic growth completely occluding the main bronchus; c) Polypoidal growth; d) Ulcerative growth; e) Necrotic growth; f) Nodular growth g) Widening of secondary carina; h) External compression.
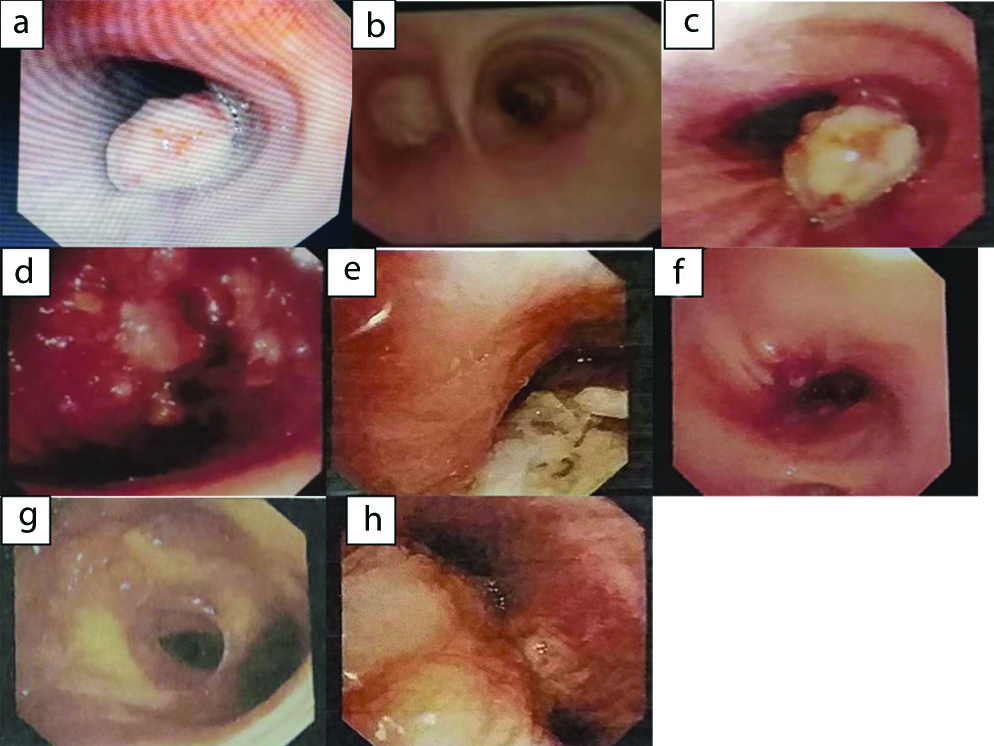
A significant relationship was found between the histopathological type and tracheal and lower lobe bronchus lesions (p-value 0.04 and 0.03, respectively); for the rest of the sites the relationship was insignificant. Most common morphologic presentation of bronchogenic carcinoma was endobronchial growth (n=86, 84.31%) and for all the endobronchial growths, SQCC was the most common histopathological diagnosis i.e., 32 cases out of 86 (37.21%). SQCC, NSCLC-NOC and SCC presented as endobronchial growths in maximum number {32 (96.97%) out of 33, 18 (81.82%) out of 22, 18 (94.74%) out of 19, respectively}. For AC, non-specific morphological finding was the most common (7 out of 13, 53.85%) rather than endobronchial growth (6 out of 13, 46.15%). External compression was the most common among the non-specific findings of AC (n=3 out of 7, 23.08%). All the histopathological types presented as an exophytic growth in the maximum number. For AC, external compression was seen as the second most common finding rather than other endobonchial growth presentations. The relationship between exophytic growth and histopathological type came significant in present study (p-value 0.041); rest of the presentations was not significantly related to the histopathological types.
Discussion
Lung cancer is the leading cause of cancer-related deaths in India and globally [1]. Lung cancer continues to be diagnosed in considerably more men than women according to the recent studies on the epidemiology of lung cancer in India [5]. The Surveillance, Epidemiology and End Results (SEER) data from 2004 to 2008 report the median age at diagnosis for cancer of the lung and bronchus was 71 years [6]. The present study was comparable with the study of Gupta RC et al., in which the percentage of total smokers was 81.6% and 60% of the total females were smokers [7] and also with that of Safwat T et al., where 86.1% of the total lung cancer patients were smokers [8]. A review article from India also suggested that 90% of all cases of lung malignancy resulted from tobacco exposure [9]. The general characteristics of the population including age group, sex ratio and smoker to non-smoker ratio of the present study was comparable to the literature as depicted in [Table/Fig-7] [4,10-15]. More than 80% of lung cancers develop in smokers, and one in nine smokers develops lung cancer [2]. The overall smoker to non-smoker ratio was the highest in the present study and this might be due to the higher male to female ratio and more number of females smokers compared to other similar studies. [13,14,15]. It might also be due to the higher percentage of SQCC and NSCLC not otherwise specified in the present study as smoking was related to NSCLC and SCC rather than AC.
Comparison of general characteristics of patients with other similar studies [4,10-15].
| Author publication (Year) | Age (years) | Male: Female | Smoker: Non-smoker |
|---|
| Lee GD et al., (2013) [10] | 71 | 5.57:1 | - |
| Gao L et al., (2012) [11] | ≥60 | 3.39:1 | - |
| Rabahi MF et al., (2012) [12] | 66 | 1.44:1 | - |
| Karpe SP et al., (2014) [4] | 51-60 | 2.3:1 | - |
| Kshatriya RM et al., (2016) [13] | - | 4:1 | 3.17:1 |
| Kumar V et al., (2017) [14] | 54.71 | 4.6:1 | 2:1 |
| Muhammad FA et al., (2019) [15] | 61.605±12.319 | - | 4.4:1 |
| Present study | 59.5±11.1 | 7.5:1 | 19.4:1 |
A detailed clinical evaluation as well as non-invasive and invasive testing is required in patients who present with suspected lung cancer to establish both the histopathologic diagnosis and disease stage. The goals of further non-invasive and invasive work-up are: 1) definitive establishment of histopathologic diagnosis; and 2) determination of disease stage in the most cost effective and least invasive manner possible [2]. The physical signs, symptoms and radiological findings of the present study were in concordance with other similar studies as shown in [Table/Fig-8] [15,16].
Comparison of major symptoms, signs and radiological findings of lung malignancy with other similar studies [15,16].
| Author publication (Year) | Major symptom | Major clinical sign | Radiological findings |
|---|
| Alamoudi OS, (2010) [16] | Cough (76.3%) | Clubbing (40.4%) | Lung mass (82.5%) |
| Muhammad FA et al., (2019) [15] | Productive cough (20.99%) | - | - |
| Present study | Cough (75.49%) | Clubbing (56.86%) | Lung mass (87.25%) (CT finding) |
There has been a shift in the pathologic distribution of NSCLC during the last four decades. SQCC was the most common histological type of NSCLC till 1970. There has been a dramatic increase in the incidence of AC from 1975 [17-19]. About the distribution of the histological subtypes in India not much information was available. According to Behera D and Balamugesh T SQCC was still the predominant histological subtype of NSCLC in India [9]. In the present study, majority of the cases came out as SQCC (32.35%). This was in comparison with other similar international and Indian studies [4,9-11,15]. This might be due to the higher smoker to non-smoker ratio in the present study compared to other similar studies. In the present study, NSCLC-NOS constitute a major histopathological type as a number of NSCLC couldn’t be classified into its various types.
Both SQCC and SCC usually present as central airway lesions while AC appears as a peripheral airway lesion. The usual manifestations of bronchogenic carcinoma are exophytic mass lesions with partial or total bronchial lumen occlusion, peribronchial tumours with extrinsic compression of the airway, with submucosal tumour infiltration, or with some combination of these entities [2]. Both SQCCs and SCCs tended to show mass like appearance; on the contrary ACs was often associated with non-specific findings like external compression or infiltration [20]. Right side was more frequently involved in the present study (n=45, 44.12%) and the comparison with other similar studies are shown in [Table/Fig-9] [4,11]. In the present study, SQCC form the largest percentage among right sided as well as left sided lesions. Among bilateral lesions, both SQCC and SCC are in equal proportions and form the most common group. However, these differences in histopthological types among the different sides were not statically significant. This was in partial comparison with the study of Karpe SP et al., who found out that SQCC was the most common subtype 11 (34.37%) on the right side followed by SCC (28.12%) [4].
Comparison of side of bronchoscopic abnormalities with other similar studies [4,11].
| Author publication (Year) | Side of bronchoscopic abnormality |
|---|
| Right | Left | Bilateral |
|---|
| Gao L et al., (2012) [11] | 51.58% | 43.2% | - |
| Karpe SP et al., (2014) [4] | 44.28% | 54.28% | 1.42% |
| Present study | 44.12% | 39.24% | 16.67% |
A comparison of the present study with various similar studies in terms of the sites and morphologic presentations of bronchogenic carcinoma and their correlation with histopathology are shown in [Table/Fig-10,11], respectively [4,10-12,14,15]. Endobronchial growth was the most common presentation with 86 cases (84.31%), higher when compared to other similar studies. Minor non-specific presentations of lung malignancy bronchoscopically might be missed by the observers as they were not prominent as endobronchial masses and this could be a reason. SQCC, NSCLC-NOC and SCC presented as endobronchial growths in maximum number {32 (96.97%), 18 (81.82%), 18 (94.74%), respectively} whereas AC presented with non-specific findings in maximum number (7, 53.85%). This was in comparison with the studies of Safwat T et al., and Muhammad FA et al., [8,15]. According to Karpe SP et al., out of the 26 cases showing exophytic growth, maximum cases were SQCC i.e., 17 (65.38%), out of the 13 cases showing nodular mass, both SQCC and SCC were in the highest number i.e., 5 (38.46%), out of the 11 cases showing irregular mucosa, maximum cases were SQCC i.e., 5 (45.45%), out of the 18 cases showing external compression, maximum cases were AC i.e., 8 (44.44%) and out of the 2 cases showing ulceration, 2 (100%) were AC [4]. The present study is in partial concordance with this study when compared to the details depicted in [Table/Fig-6]. The endoscopic growths were divided into more different types like exophytic, nodular, cauliflower, necrotic, polypoidal, infiltrative and ulcerative rather than dividing only into exophytic and nodular. These might be the reasons for lower percentages of SQCC and SCC among the exophytic growths and lower percentages of SCC and AC among the nodular growths when compared to the study of Karpe SP et al., [4].
Comparison of site of bronchoscopic abnormalities with other similar studies [4,10,11,15].
| Author Publication (Year) | Site of lesion | SQCC | NSCLC-NOS | SCC | AC | Others | Total |
|---|
| n | % | N | % | N | % | N | % | N | % | N | % |
|---|
| Lee GD et al., (2013) [10] (N=611) | T&C | - | - | - | - | - | - | - | - | - | - | 3 | 0.5 |
| MSB | - | - | - | - | - | - | - | - | - | - | 75 | 12.3 |
| IMB | - | - | - | - | - | - | - | - | - | - | - | - |
| LB | - | - | - | - | - | - | - | - | - | - | 501 | 82 |
| SB & 2&/3C | - | - | - | - | - | - | - | - | - | - | 32 | 5.2 |
| Mul LB | - | - | - | - | - | - | - | - | - | - | - | - |
| B/L | - | - | - | - | - | - | - | - | - | - | - | - |
| Gao L et al., (2012) [11] (N=1489) | T&C | 10 | 6.7 | 0 | 0 | 3 | 0.2 | 3 | 0.2 | 0 | 0 | 16 | 1.07 |
| MSB | 119 | 8 | 0 | 0 | 52 | 3.49 | 26 | 1.75 | 0 | 0 | 197 | 13.23 |
| IMB | - | - | - | - | - | - | - | - | - | - | - | - |
| LB | 531 | 35.7 | 0 | 0 | 359 | 24.11 | 327 | 21.96 | 2 | 0.13 | 1219 | 81.87 |
| SB & 2&/3C | 18 | 1.2 | 0 | 0 | 18 | 1.2 | 17 | 1.14 | 0 | 0 | 53 | 3.56 |
| Mul LB | - | - | - | - | - | - | - | - | - | - | - | - |
| B/L | 2 | 1.3 | 0 | 0 | 0 | | 2 | | 0 | | 4 | |
| Karpe SP et al., (2014) [4] (N=70) | T&C | - | - | - | - | - | - | - | | - | - | - | - |
| MSB | 16 | 22.9 | 0 | 0 | 12 | | 0 | | 1 | | 29 | |
| IMB | 1 | 1.4 | 0 | 0 | 0 | | 0 | | 0 | | 1 | |
| LB | 13 | 18.57 | 0 | 0 | 2 | 2.86 | 13 | 18.57 | 7 | 10 | 35 | 50 |
| SB & 2&/3C | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 7.14 | 0 | 0 | 5 | 7.14 |
| Mul LB | - | - | - | - | - | - | - | - | - | - | - | - |
| B/L | - | - | - | - | - | - | - | - | - | - | - | - |
| Muhammad FA et al., (2019) [15] (N=81) | T&C | - | - | - | - | - | | - | | - | | - | |
| MSB | 12 | 14.81 | 0 | 0 | 5 | 6.17 | 6 | 7.41 | 2 | 2.47 | 25 | 30.86 |
| IMB | - | - | 0 | 0 | 6 | 7.41 | 0 | 0 | 1 | 1.23 | 7 | 8.64 |
| LB | 18 | 22.22 | 0 | 0 | 13 | 16.05 | 13 | 16.05 | 2 | 2.47 | 46 | 56.8 |
| SB & 2&/3C | - | - | - | - | - | - | - | - | - | - | - | - |
| Mul LB | - | - | - | - | - | - | - | - | - | - | - | - |
| B/L | - | - | - | - | - | - | - | - | - | - | - | - |
| Present study (N=102) | T&C | 3 | 2.94 | 1 | 0.98 | 5 | 4.9 | 0 | 0 | 4 | 3.92 | 13 | 12.75 |
| MSB | 12 | 11.76 | 8 | 7.84 | 6 | 5.88 | 4 | 3.92 | 6 | 5.88 | 36 | 35.29 |
| IMB | 6 | 5.88 | 5 | 4.9 | 1 | 0.98 | 0 | 0 | 0 | 0 | 12 | 11.76 |
| LB | 8 | 7.84 | 4 | 3.92 | 5 | 4.9 | 6 | 5.88 | 2 | 1.96 | 25 | 24.51 |
| SB & 2&/3C | 1 | 0.98 | 4 | 3.92 | 2 | 1.96 | 3 | 2.94 | 3 | 2.94 | 13 | 12.75 |
| Mul LB | 1 | 0.98 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0.98 |
| B/L | 2 | 1.96 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 1.96 |
T-&C: Trachea& Main carina; MSB: Main stem bronchi; IMB: Intermediate bronchus; LB: Lobar bronchi; SB & 2&/3C: Segmental bronchi and/or secondary and/or tertiary carina; Mul LB: Multiple lobar bronchi; B/L: Bilateral; NSCLC-NOS: Non-small cell carcinoma not otherwise specified; SQCC: Squamous cell carcinoma; SCC: Small cell carcinoma; AC: Adenocarcinoma; UN: Undifferentiated malignancy
Comparison of morphological appearances with other similar studies [4,10-12,14].
| Author Publication (Year) | Total cases | Histopathology N (% out of total cases) | Bronchoscopic findings |
|---|
| Endoscopic growth N (% out of total cases) | Other findings n (% out of total cases) | | Nl Study N (%) |
|---|
| SQCC | NSCLC-NOS | SCC | AC | Ot | SQCC | NSCLC | SCC | AC | OT | Total | SQCC | NSCLC | SCC | AC | Ot | Total |
|---|
| Lee GD et al., (2013) [10] | 611 | 323 (52.9) | 62 (10.2) | 107 (17.5) | 82 (13.42) | 37 (6.1) | - | - | - | - | - | 423 (69.2) | - | - | - | - | - | 47 (7.7) | 69 (11.3) |
| Gao L et al., (2012) [11] | 1489 | 680 (45.7) | - | 432 (29.0) | 375 (25.2) | 2 (0.1) | 660 (44.3) | - | 414 (27.8) | 337 (22.6) | 2 (0.1) | 1414 (95) | 10 (0.7) | - | 16 (1.1) | 24 (1.6) | 0 (0) | 50 (3.4) | 25 (1.7) |
| Rabahi MF et al., (2012) [12] | 105 | 40 (38.1) | - | 15 (14.3) | 24 (22.9) | 26 (25.5) | 33 (31.4) | - | 12 (11.4) | 12 (11.4) | 19 (18.1) | 74 (70.5) | 7 (6.7) | - | 3 (2.9) | 12 (11.4) | 9 (8.6) | 31 (29.5) | - |
| Karpe SP et al., (2014) [4] | 70 | 30 (42.9) | - | 14 (20) | 18 (25.7) | 8 (11.4) | 22 (31.4) | - | 10 (14.3) | 4 (5.7) | 3 (4.3) | 39 (55.7) | 8 (11.4) | - | 7 (10) | 11 (15.7) | 5 (7.1) | 31 (44.3) | - |
| Kumar V et al., (2017) [14] | 45 | 28 (62.2) | - | 1 (2.2) | 12 (26.7) | 4 (8.9) | 23 (51.1) | - | 1 (2.2) | 7 (15.6) | 1 (2.2) | 32 (71.1) | 5 (11.1) | - | - | 5 (11.1) | 3 (6.7) | 17 (37.8) | - |
| Present study | 102 | 33 (32.4) | 22 (21.6) | 19 (18.6) | 13 (12.7) | 15 (14.7) | 32 (31.4) | 18 (17.6) | 18 (17.6) | 6 (5.9) | 12 (11.8) | 86 (84.3) | 1 (1) | 4 (3.9) | 1 (1) | 7 (6.87) | 3 (2.9) | 16 (15.7) | - |
SQCC: Squamous cell carcinoma; NSCLC-NOS: Non-small cell carcinoma not otherwise specified; SCC: Small cell carcinoma; AC: Adenocarcinoma; Ot: Others; Nl study: Normal study
Limitation(s)
First one is the small sample size of the study population. So the representation of patients in many of the histopathological types seen in minority could not be effectively calculated. This was a single center study. Due to financial constraints, the present study could not classify the patients diagnosed as NSCLC into SQCC or AC and this became a major limitation of present study as the representation of SQCC and AC in present study could be more and could correlate with the bronchoscopic presentations more effectively [4].
Conclusion(s)
The bronchoscopic appearance is associated to histological type. Both SQCC and SCC were more in the central airways as compared to the peripheral airways; hence endoscopically they were visualised easily and had the presentation of intraluminal growth commonly. ACs was more common in the peripheral airways and endoscopically they had non-specific features like external compression, secondary and/or tertiary carinal widening and ulcerative/corrugative mucosa more than intraluminal growth. These findings represent the importance of a standardised description of FOB findings as a tool in the diagnosis of lung cancer.
R: Right; L: Left; B/L: Bilateral; NSCLC-NOS: Non-small cell carcinoma not otherwise specified; SQCC-Squamous cell carcinoma, SCC: Small cell carcinoma; AC: Adenocarcinoma; UN: Undifferentiated malignancy; PDN: Poorly differentiated neoplasm; NEC: Neuroendocrine carcinoma
T: Trachea; C: Main carina; MSB: Main stem bronchi; IMB: Intermediate bronchus; ULB: Upper lobe bronchi; MLB: Middle lobe bronchus; LLB: Lower lobe bronchi; SB: Segmental bronchi; U&LLB: Upper and lower lobe bronchi; B/L ULB: Bilateral ULB; 2&/3C: Secondary and/or tertiary carina; NSCLC-NOS: Non-small cell carcinoma not otherwise specified; SQCC: Squamous cell carcinoma; SCC; Small cell carcinoma; AC: Adenocarcinoma, UN: Undifferentiated malignancy; OTH: Others
SQCC: Squamous cell carcinoma; NSCLC-NOS: Non-small cell carcinoma not otherwise specified; SCC: Small cell carcinoma; AC: Adenocarcinoma; UN: Undifferentiated malignancy; PDN: Poorly differentiated neoplasm; NEC: Neuroendocrine carcinoma
SQCC: Squamous cell carcinoma; NSCLC-NOS: Non-small cell carcinoma not otherwise specified; SCC: Small cell carcinoma; AC: Adenocarcinoma; UN: Undifferentiated malignancy
T-&C: Trachea& Main carina; MSB: Main stem bronchi; IMB: Intermediate bronchus; LB: Lobar bronchi; SB & 2&/3C: Segmental bronchi and/or secondary and/or tertiary carina; Mul LB: Multiple lobar bronchi; B/L: Bilateral; NSCLC-NOS: Non-small cell carcinoma not otherwise specified; SQCC: Squamous cell carcinoma; SCC: Small cell carcinoma; AC: Adenocarcinoma; UN: Undifferentiated malignancy
SQCC: Squamous cell carcinoma; NSCLC-NOS: Non-small cell carcinoma not otherwise specified; SCC: Small cell carcinoma; AC: Adenocarcinoma; Ot: Others; Nl study: Normal study