The hip joint has a huge account of the functional demands on it by the human body. Biomechanics of hip joints are complex, but a stable painless hip is required for normal locomotion [1]. Hip joint is affected by numerous diseases. With the advancement in anaesthesia, intraoperative and postoperative care, risk of operating on the hip has become very low, thus increasing the widespread acceptance of elective surgery [2]. THR is a surgical technique that has relieved pain of many of people arising from the hip joint. Currently, it is adult reconstructive hip process most frequently done. THR has succeeded in alleviating pain due to hip joint pathology while maintaining hip joint mobility and stability [1]. Instability can be defined as the complete subluxation (dislocation) of the femoral head from the acetabular socket [1]. The risk factors causing instability after THR can be preoperative, intraoperative and postoperative which includes elements like alcoholism, neurocognitive disorder, gender female, surgical approach and malpositioning of femoral and acetabular components [3].
The surgical interventions after unstable THR includes revision of malpositioned prosthesis, increasing the size of femoral component, application of a constrained liner, soft tissue reinforcement procedures and osteotomy and advancement of the greater trochanter. A sequential approach is introduced for the treatment of repeated dislocation and multiple variables for the cause of post THR instability [1,2,4]. To assess the effectiveness of procedures such as THR, it is necessary to examine the long-term effects of an operative procedure. Scales of patient-derived result provides a method for comparison of results. The Harris hip score is a commonly used score for assessing hip functions [1,5].
This present study has been conducted to evaluate preoperative, intraoperative and postoperative risk factors influencing instability after THR surgery.
Materials and Methods
A retrospective study was conducted which included the patients who underwent THR from June 2013 to June 2019 (six years) at the institute and tertiary care centre. Institutional Ethics Committee (IEC) approval was obtained (DMIMS (DU)/IEC/2018-19/7398).
Inclusion criteria: Patient undergoing THR in the hospital irrespective of the aetiology and age and patient consenting to participate in this study.
Exclusion criteria: The patients who were not consenting to participate in the study and patient below 18 years of age and patient with polyneuropathy. A total number of 130 cases underwent THR in the given study period. Sample size of 98 or more cases was needed to have a confidence interval of 95% with 5% margin of error. A total of eight patients who had instability were included in the group having postoperative dislocation and 122 patients were in normal THR group.
Methods of Data Collection
A pre-tested, semi structured questionnaire was developed and used for data collection which included clinical details of the patients, associated co-morbidity, personal habits/addictions, clinical hip range of motion assessment, preoperative, postoperative and follow-up clinical outcome scorings (Harris Hip Score) and radiological assessment of the patients. Preoperative, postoperative and six month follow-up data was recorded in the questionnaire. Clinical outcome was measured using Harris Hip score [Table/Fig-1].
Grading of Harris hip score.
| Grading for the Harris Hip Score [1] |
|---|
| Successful result |
| Postoperative increase in Harris Hip Score of >20 points + radiographically stable implant + no additional femoral reconstruction |
| Or Score- |
| <70 | Poor | 70-79 | Fair | 80-89 | Good | 90-100 | Excellent |
The radiological assessment was done using the parameters like femoral stem positioning, horizontal and vertical offset, acetabular inclination, inadequate version with the help of anteroposterior and lateral radiographs which was done preoperatively, postoperatively and at every follow-up [6].
To evaluate the risk factors, risk factor were classified into three division: i) Preoperative; ii) Intraoperative; iii) Postoperative risk factors. Furthermore, in the preoperative group, the factors evaluated were age, gender, alcoholism and history of previous ipsilateral hip surgeries. In the intraoperative group, the risk factors included were approach used and capsule repair/capsulectomy done. Postoperative risk factors were femoral offset derangement, component malpositioning and patient non-compliance.
Statistical Analysis
Data was analysed by using Statistical Package for the Social Sciences (SPSS) software version 17.0 Statistical tools used were proportions and percentages and other appropriate Statistical tests of significance like student’s t-test, chi-square test.
Results
Dislocation post THR was observed in 8 (6.15%) patients and all these patients were males. The majority of the patients in the study were in the age group of 31-40 years and 41-50 years (27.69% each) with total mean age of 41.14±12.40 years. Mean age was 40.82±12.06 years in normal THR patients and 44.63±12.98 years in dislocated THR patients. However, no statistical significance was found between side affected and incidence of dislocation [Table/Fig-2]. Six (75%) patients in hip dislocation group were chronic alcoholics while 41 (33.61%) in non-dislocation group were alcoholics and incidence of dislocation and alcoholism was statistically significant (p-value: 0.047).
Demographic distribution of the study population.
| Age group (years) | No. of patients | Percentage |
|---|
| ≤20 | 2 | 1.54 |
| 21-30 | 29 | 22.31 |
| 31-40 | 36 | 27.69 |
| 41-50 | 36 | 27.69 |
| 51-60 | 20 | 15.38 |
| 61-70 | 5 | 3.85 |
| >70 | 2 | 1.54 |
| Sex | | |
| Male | 101 | 77.69 |
| Female | 29 | 22.31 |
| Side affected | | |
| Right | 70 | 53.8 |
| Left | 60 | 46.2 |
| Total: 130 |
Capsule was resutured in 50% patients of dislocation group and 81.97% of non-dislocation group. Proportion of component malpositioning was more in dislocation patients (25%) as compared to non-dislocation patients (11.48%) but the difference was not significant [Table/Fig-3].
Risk factors of instability with functional outcome.
| Risk factors | | Hip dislocation | No hip dislocation | Odds ratio (Confidence interval) | p-value |
|---|
| No. of patients | % | No. of patients | % |
|---|
| Sex | Male | 8 | 100.00 | 93 | 76.23 | NA | 0.260 |
| Female | 0 | 0.00 | 29 | 23.77 |
| Side | Right | 4 | 50.00 | 66 | 54.10 | 0.8485 (0.2029-3.589) | 0.887 |
| Left | 4 | 50.00 | 56 | 45.90 |
| Alcohol abuse | Yes | 6 | 75.00 | 41 | 33.61 | 5.9268 (1.1453-43.6534) | 0.047 |
| No | 2 | 25.00 | 81 | 66.39 |
| Previous hip surgery | Yes | 2 | 25.00 | 12 | 9.84 | 3.0556 (0.5539-16.8547) | 0.452 |
| No | 6 | 75.00 | 110 | 90.16 |
| Surgical approach | Posterior | 0 | 0.00 | 13 | 10.66 | NA | 0.459 |
| Posterolateral | 5 | 62.50 | 92 | 75.41 |
| Lateral | 3 | 37.50 | 17 | 13.93 |
| Capsule resutured | Yes | 4 | 50.00 | 100 | 81.97 | 0.22 (0.0511-0.9480) | 0.083 |
| No | 4 | 50.00 | 22 | 18.03 |
| Capsulectomy | Yes | 4 | 50.00 | 20 | 16.39 | 5.100 (1.1768-22.1030) | 0.050 |
| No | 4 | 50.00 | 102 | 83.61 |
| Component malposition | Yes | 2 | 25.00 | 14 | 11.48 | 2.5714 (0.4724-13.9974) | 0.566 |
| No | 6 | 75.00 | 108 | 88.52 |
| Patient non-compliance | Yes | 3 | 37.50 | 17 | 13.93 | 3.7059 (0.8102-16.9498) | 0.199 |
| No | 5 | 62.50 | 105 | 86.07 |
NA: Not applicable
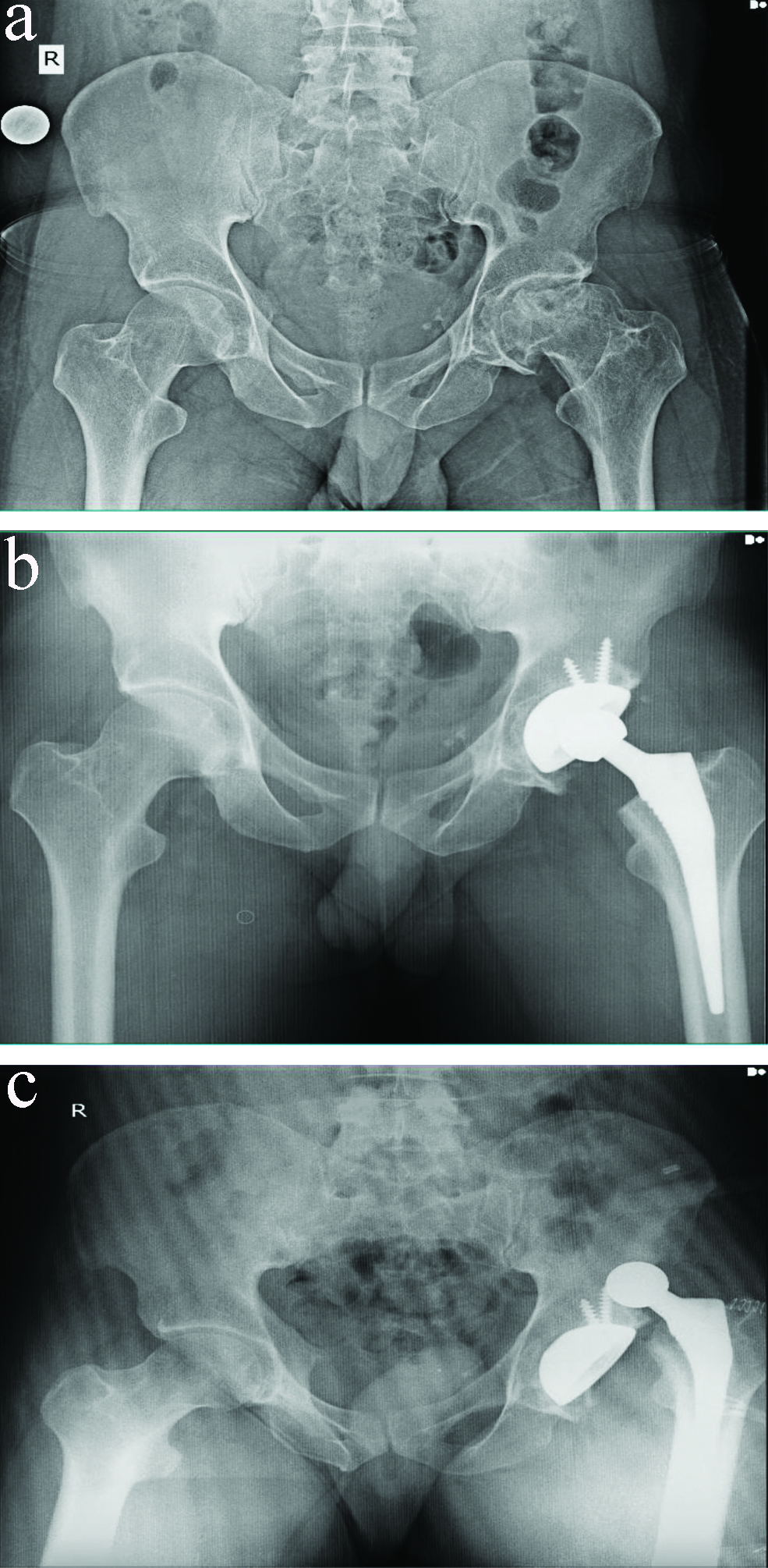
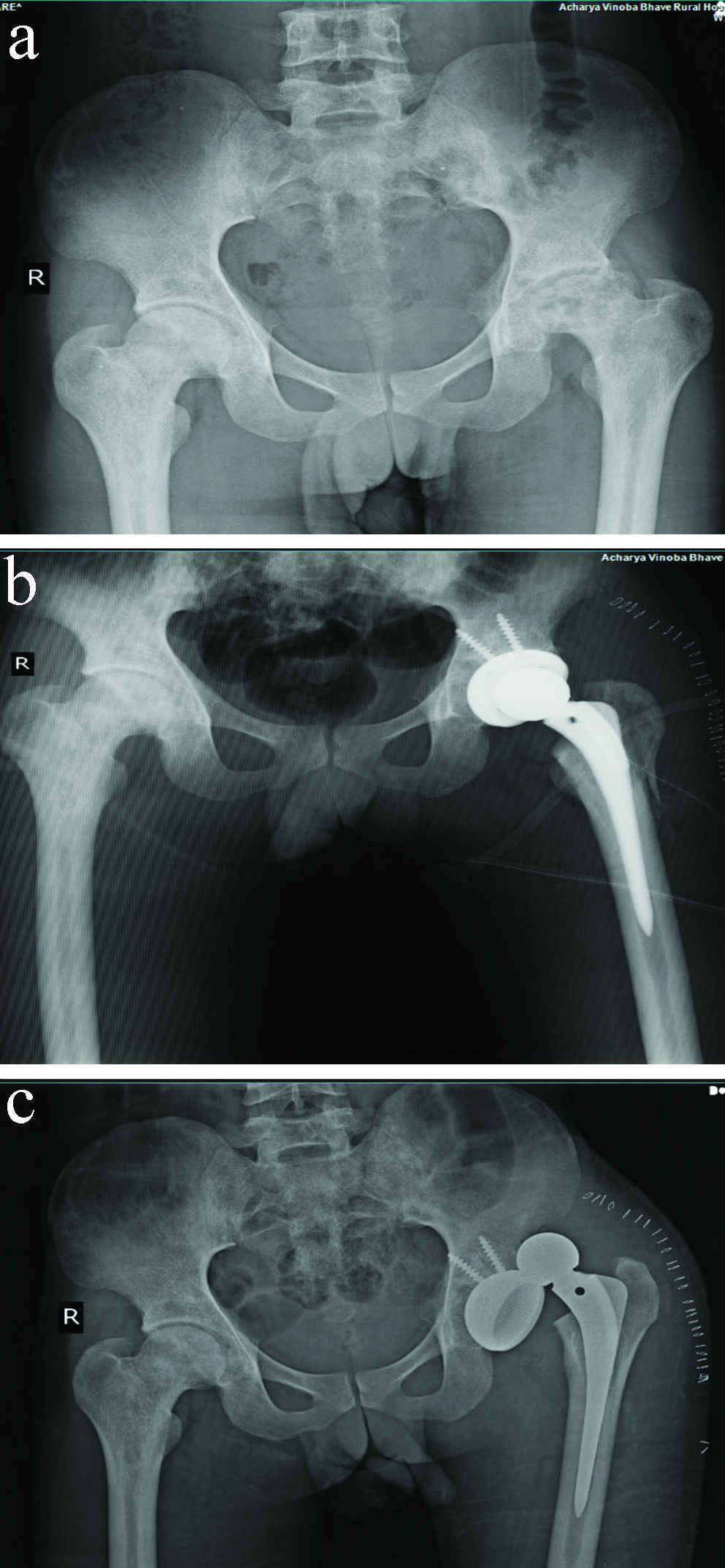
The mean preoperative Harris hip score among the hip dislocated patients was 54.88±5.11, while among non-dislocation patients was 54.57±4.74 which increased to 70.219±3.45 in hip dislocation patients and 80.94±5.35 in normal THR patients at the end of six months follow-up. It was seen that the mean postoperative and follow-up Harris Hip score among the hip dislocated patients was less as compared to non-dislocated patients and the difference observed in the score was also statistically significant. (p-value 0.004). In the present study, two deaths were observed one from each group. But the deaths were not associated with dislocation or complication due to surgery. The radiographs of some cases in this study is shown in [Table/Fig-4,5].
Avascular necrosis of left femoral head. (a) Preoperative X-ray of pelvis with both hips anteroposterior view shows destruction of left femoral head and decreased joint space. (b) Postoperative X-ray of pelvis with both hips anteroposterior view shows implant in situ on left side. (c) X-ray of pelvis with both hips anteroposterior view shows dislocation after THR.
Avascular necrosis of left femoral head. (a) Preoperative X-ray of pelvis with both hips anteroposterior view shows flattening and destruction of left femoral head, with subchondral sclerosis and decreased intra-articular space. (b) Postoperative X-ray of pelvis with both hips anteroposterior view acetabular socket fixed with 2 screws and femoral component placed centrally in the femur. (c) X-ray of pelvis with both hips anteroposterior view shows dislocated femoral componenet from the acetabular socket.
Discussion
The present study was conducted in the Department of Orthopaedics with the aim to study the risk factors influencing instability after THR. For this purpose, retrospective analysis of all the hip replacement surgeries conducted from years June 2013 to June 2019 were selected and were analysed for hip instability. Thus, in the present study total 130 cases of hip replacement were recorded. It was observed that majority of the patients in the study were in the age group of 31-40 years and 41-50 years (27.69% each). It was observed that 77.69% patients were male and 22.31% were female. In the Masaoka T et al., study, the patients ranged in age from 23 to 84 years (mean 61.6 years) and there were 20.68% men and 79.32% women [7]. Incidence of dislocation was observed in 6.15% cases in present study. Masaoka T et al., observed that out of the 317 hips included, 10 (3.2%) were dislocated [7]. Leichtle UG et al., reported dislocation rate after primary THA of 1.1% [8]. Woo RY and Morrey BF encountered overall 2.44% dislocation rate at the end of first year after surgery [9]. von Knoch M et al., studied 19680 cases of hip replacement and observed 2.60% incidence of postoperative dislocation [10]. The overall dislocation rate reported by van Stralen GM et al., was 1.36% [11]. International literature and registers have mentioned annual rate of THR dislocations after primary THR was between 0.2% and 10% [12,13]. Scottish National Arthroplasty Registry has documented a dislocation rate of 1.9% after hip replacement surgeries [14]. Whereas, a dislocation rates of up to 28% was reported after revision and implant exchange surgeries by some authors [15,16]. Thus, wide variation in the incidence was observed. Hence, the findings of present study had similarity with literature.
The mean age of patients with hip dislocation was 44.63±12.98 years while that of non-dislocated patients was 40.82±12.06 years. Thus, the age was not observed as an independent risk factor for hip instability among hip replacement patients as the results were not significant. Bourne RB and Mehin R and Newington DP et al., have not found age as an independent predictor of instability that was similar to present study [17,18]. While Morrey BF and Ekelund A et al., concluded that in patients older than 80 years of age operated with THR had a two to three times increase in the rate of dislocation compared with a younger group [19-21]. It was seen that all the cases with hip dislocation were male. Among the non-dislocation patients 76.23% patients were male and the difference was not significant (p-value- 0.260). Thus, gender was not observed as a significant risk factor for hip instability after hip replacement surgery. In contrary, Berry DJ observed female gender as a significant risk factor associated with dislocation [22]. A Study by Wetters NG et al., didn’t find conclusive evidence about women being a risk factor for dislocation which was similar to present study [15]. It was seen that 75% patients in hip dislocation group were alcoholics while 33.61% in non-dislocation group were alcoholics and the difference observed was statistically significant (p-value- 0.047). Two alcoholic patients went in alcohol withdrawal postsurgery and resulted in dislocation. Thus, alcoholism was identified as risk factor for dislocation post THR. A dislocation rate as high as 23% was associated with alcoholism according to Lu Y et al., [23]. Similarly, in comparison to present study, Paterno SA et al., also found alcoholism as a risk factor for postoperative dislocation [24]. It was seen that 25% patients with hip dislocation and 9.84% patients with non-dislocation group had history of previous hip surgery. Woo RY and Morrey BF evaluated incidence of instability to double in hips that underwent any previous surgical procedure [9]. Thus, the results were not comparable which may be due to less number of cases which underwent previous hip surgeries. It was seen that majority of the patients were operated from postero-lateral approach in both the groups and the results were insignificant (p=0.459). The incidence of instability as quoted in the literature reports higher dislocation for the posterior approach (5.8%) vs the anterolateral approach (2.3%) [25].
Capsule was resutured in 50% patients of dislocation group and 81.97% of non-dislocation group. Thus, capsule re-suturing appears to be protective factor to prevent dislocation. Capsule resuturing restores the soft tissue tension across the hip joint and has been evaluated as a factor in dislocation [26]. Capsulectomy was done in 50% patients of hip dislocation group and 16.39% of non-dislocation group thus capsulectomy appears as a significant risk factor for postoperative hip dislocation (p-value- 0.05). In comparison to present study, a dislocation frequency of 4.8% after capsulectomy and 0.7% after capsular repair has been reported following the posterolateral approach by Mallory TH et al., [26]. In the literature, postoperative soft-tissue tension has been reported as a factor in dislocation. However, after a posterior approach, reconstruction of capsule and external rotators reduced the dislocation rate from 4.1% to 0.0% as studied by Pellicci PM et al., [27]. The proportion of malposition was more in dislocation patients (25%) as compared to non-dislocation patients (11.48%) but the difference was not significant. Implant-related risk factors like malpositioning of components are a common cause of instability [9]. A study by Callanan MC et al., concluded increased risk of acetabular cup malposition for minimally invasive approaches resulted in unstable hip replacements [28]. It was seen that the mean postoperative and follow-up Harris Hip score among the hip dislocated patients was less as compared to non-dislocated patients and the difference observed in the score was also statistically significant (p-value 0.004). Thus, the functional outcome was better among the non-dislocation patients as compare to hip dislocated patients. Gupta S et al., also used Harris hip scoring for evaluation of functional outcome of THR and concluded good clinical outcome was observed in maximum number of cases (78%) [29].
Limitation(s)
Sample size of patient with postoperative dislocation was less as compared to normal THR group, resulting in difficulty in comparison of statistics. As the study was done in a medical institute, different surgeons with a varying surgical skills and approach preference were performing surgery. Follow-up period of present study was less. Radiological complications like stress shielding, calcar resorption, etc., requires long term studies.
Conclusion(s)
Thus, the incidence of hip instability after THR was 6.15%. Alcohol addiction was identified as a statistically significant independent preoperative risk factor. It was observed that capsulectomy was a significant risk factor for hip dislocation. Postoperative risk factors like decreasing femoral offset, component malposition and patient non compliance were also associated with hip dislocation, but none of the were statistically significant. However, clinical outcome of all the patients significantly improved postoperatively as evaluated by Harris Hip Score.
NA: Not applicable