Association between Blood Pressure and Obesity Indices in Medical Students
Shalini Gandhi1, Jitender Sorout2, Rohit Raina3, Abhay Raina4, Urvashi Miglani5, Kailash Manchanda6, Satyanath Reddy7
1 Associate Professor, Department of Physiology, KD Medical College Hospital and Research Center, Mathura, Uttar Pradesh, India.
2 Tutor, Department of Physiology, KD Medical College Hospital and Research Center, Mathura, Uttar Pradesh, India.
3 Registrar Department of Gynaecology and Obstetrics, Inderprastha Apollo Hospital, New Delhi.
4 Radiologist, Department of Radiology, Krishna Scan Center, Cuddalore, Tamil Nadu, India.
5 Specialist, Obstetrics and Gynaecology, Deen Dayal Upadhyay Hospital, Delhi.
6 Professor & HOD, Department of Physiology, KD Medical College Hospital and Research Center, Mathura, Uttar Pradesh, India.
7 Assistant Professor, Department of Physiology, KD Medical College Hospital and Research Center, Mathura, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Jitender Sorout, VPO- Gorota, Teh. Hodal, Dist. Palwal (Haryana), Hodal, Haryana, India.
E-mail: jitendersorout123@gmail.com
Introduction
Obesity is strongly associated with other metabolic disorders including Hypertension (HTN), diabetes and Cardiovascular Diseases (CVD). High Blood Pressure (BP) is ranked as the third most important risk factor for attributable burden of disease in South Asia.
Aim
The aim of present was to study the association between BP and obesity indices in medical student’s population.
Materials and Methods
A cross sectional study was conducted on a group of 100 healthy young medical students. BP, pulse and Hb O2% was measured by using sphygmomanometer, pulse oximeter. Obesity indices were measured by using weighing machine, stadiometer, measuring tape and impedance based Body Composition Analyser (BCA).
Results
There was poor correlation of Systolic Blood Pressure (SBP) and Diastolic Blood Pressure (DBP) with Total Body Fat (TF) and the association was not significant. SBP and DBP were mildly correlated with BMI. Whole body Visceral Fat (VF) correlation of SBP was moderate and significant. DBP was correlated with whole body VF and correlation was significant. But the whole body, trunk, leg Skin Fat (SF) and Muscle Fat (MF) were not having significant correlation with SBP and DBP. Finger to heart distance was positively correlated with SBP (p<0.05). Also, O2%, chest and hip size were positively correlated with SBP (p<0.05). Only whole body VF and Waist Hip Ratio (WHR) were significantly (p<0.05) affected SBP. None of the other parameters affected DBP.
Conclusion
The present study results found that Body Mass Index (BMI), VF and WHR had significant correlation with systolic and SBP and DBP. VF and WHR were significant predictors of SBP.
Body mass index, Cardiovascular Diseases, Fat, Hypertension
Introduction
As per World Health Organisation (WHO), Obesity is considered as one of the most common yet neglected public health problem both in developed as well as developing countries. Statistically, according to the 2012 WHO report, worldwide, one in six adults are obese and about 2-8 million individual deaths occur due to overweight or obesity every year [1]. Obesity due to its high morbidity and mortality risks is recognised as a disease itself. Obesity has a strong association with other metabolic disorders namely HTN, diabetes, dyslipidemia, CVD and even some forms of cancer [2].
Thus, obesity is the epidemic for young adults in developing country like India due to sedentary lifestyle, eating habits and inadequate physical activity. Obesity has been found to increase the risk of morbidities and mortalities, including CVD, diabetes, gallbladder disease, respiratory disease, cancer, arthritis and gout [3]. Central distribution of body fat suggests excessive deposition of intra-abdominal fat in other words known as abdominal obesity found to be one of the important predictors of CVD risk [4].
India, with 1.3 billion people is the second most populous country in the world and is currently experiencing rapid epidemiological transition. Industrialisation and urbanisation also contribute to increased prevalence of obesity. Studies from different parts of India have provided evidence of the rising prevalence of obesity [5].
Similarly, in 2010 in South Asia high BP was ranked as third most important risk factor for diseases. Also in India, cardiovascular health status and health care systems are substantially burdened by HTN. About 57% of deaths due to stroke and 24% of deaths due to Coronary Heart Disease are directly related to HTN. HTN is rated as one of the most important cause of premature death worldwide by WHO [6,7]. The co-morbidity of obesity includes diseases such as CHDs, HTN, stroke and certain type of cancer. So, the aim of present study was to study the association between BP and obesity indices in Medical students.
Materials and Methods
A cross sectional study was conducted on a group of 100 healthy young medical students.
Inclusion criteria: Subjects of both genders; aged between 18-25 years were recruited for the study after taking written informed consent. The study was approved by the Institutional Ethical Committee (KDMCHRC/IEC/2018/01) of KD Medical College Hospital and Research Center, Mathura, Uttar Pradesh, India. The duration of study was six months from January 2019 to June 2019.
Exclusion criteria: The subjects of Acute illness (Acute myocardial infarction, Hypothyroidism, Liver disorder, Renal diseases) and known cases of any chronic illness- HTN, diabetes etc., were excluded from the study.
Blood Pressure
Resting BP (Systolic and diastolic) were measured after a sitting rest of 15-30 minutes by using mercury sphygmomanometer in sitting posture. Pulse rate and % oxygen saturation were measured by using pulse oximeter in same sitting position [7].
Obesity Indices
Anthropometric measures: Weight and height were measured in accordance with National Health and Nutrition Examination Survey (NHANES) anthropometric measuring guidelines with help of weighing machine and stadiometer [8]. Waist circumference, chest circumference, hip circumference and WHR were assessed. Waist circumference was measured at level of umbilicus and hip circumference was measured at maximum protrusion of hip in standing position in centimetres with heals together at linen measuring tape. Three measurements was taken for each site and average score recorded as final [9]. TF, VF was measured. Also, SF and MF of (whole body, arm, trunk and leg) was measured by using an impedance based BCA {Karada Scan of Omron Healthcare (Body Composition Monitor HBF-701)} [Table/Fig-1] [10].
Bioelectrical Impedance Analyser (BIA) Modal (HBF-701).
Image was taken from the booklet of the instrument
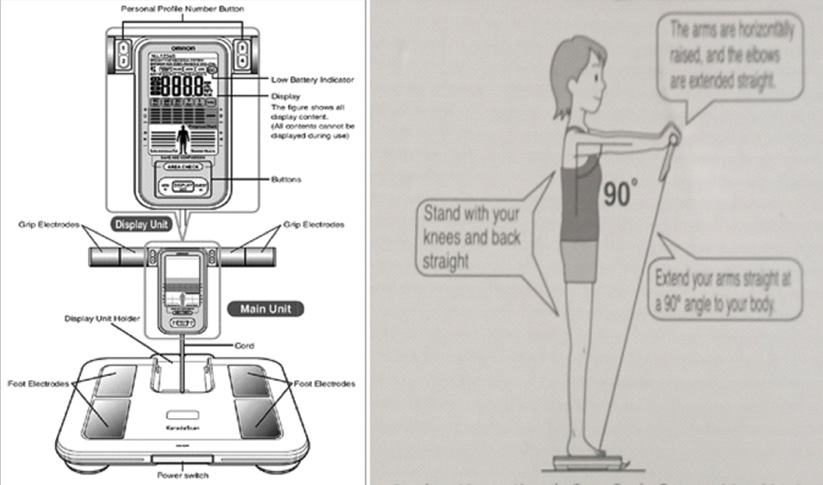
Bioelectrical Impedance Analyser (BIA) produces a close estimate of fat mass in a wide range of body compositions. It is a non-invasive measurement of body composition and also has many advantages compared with other methods because it is inexpensive, simple, fast, safe, portable and easy to perform, as well as requires minimum operator training [11].
Statistical Analysis
The results are presented in percentages and mean (SD). The Pearson correlation coefficient was calculated. Those parameters found to be significantly correlated were entered in multivariate linear regression analysis. The p-value <0.05 was considered significant. All the analysis was carried out on SPSS 16.0 version (Chicago, Inc., USA).
Results
The present cross-sectional study investigated 100 subjects (mean age 20.42±1.35 years, range 18-25 years), including 29 males and 71 females. The anthropometric obesity indices, demographic characteristics and disease variables of the study population are shown in [Table/Fig-2].
Distribution of Mean and SD of Different study parameters.
| Study parameters | Mean | SD | Minimum | Maximum |
|---|
| Age (years) | 20.42 | 1.35 | 18.00 | 25.00 |
| Height (cm) | 161.44 | 8.21 | 134.00 | 193.00 |
| Weight (kg) | 59.59 | 11.73 | 38.80 | 108.60 |
| Total body fat | 26.14 | 6.85 | 12.20 | 50.00 |
| BMI | 22.83 | 3.78 | 16.70 | 33.20 |
| VF | 6.32 | 4.83 | 0.50 | 40.00 |
| Whole body |
| Skin fat | 19.11 | 5.74 | 8.50 | 34.80 |
| Muscle fat | 31.21 | 3.21 | 22.40 | 38.30 |
| Arm |
| Skin fat | 28.59 | 8.44 | 13.10 | 48.80 |
| Muscle fat | 36.93 | 5.62 | 18.10 | 57.30 |
| Trunk |
| Skin fat | 16.93 | 5.82 | 7.10 | 44.30 |
| Muscle Fat | 24.82 | 6.15 | 13.60 | 54.00 |
| Leg |
| Skin fat | 28.11 | 8.22 | 9.00 | 53.50 |
| Muscle Fat | 46.58 | 5.89 | 19.10 | 54.40 |
| SBP (mmHg) | 112.56 | 8.30 | 92.00 | 138.00 |
| DBP (mmHg) | 75.44 | 8.77 | 56.00 | 106.00 |
| Pulse/Minute | 85.15 | 11.19 | 58.00 | 100.00 |
| O2 % | 93.54 | 7.82 | 63.00 | 110.00 |
| Chest size (cm) | 32.05 | 2.85 | 26.00 | 43.00 |
| Hip size (cm) | 33.53 | 2.94 | 25.00 | 45.00 |
| CHR | 0.95 | 0.04 | 1.17 | 0.875 |
| WHR | 1.76 | 0.24 | 1.23 | 2.41 |
V Fat: Visceral fat; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; CHR: Chest hip ratio; WHR: Waist hip ratio; BMI: Body mass index
The correlations between SBP and obesity indices were summarised in [Table/Fig-3]. SBP and DBP were mildly correlated with some of the parameters summarised in above mentioned [Table/Fig-3].
Correlation of study parameters with Blood Pressure (BP).
| Study parameters | SBP | DBP |
|---|
| Correlation coefficient (r) | p-value | Correlation coefficient (r) | p-value |
|---|
| Total body fat | -0.03 | 0.73 | 0.16 | 0.11 |
| BMI | 0.29 | 0.003* | 0.21 | 0.04* |
| VF | 0.34 | 0.001* | 0.23 | 0.02* |
| Whole body |
| Skin fat | 0.12 | 0.22 | 0.08 | 0.40 |
| Muscle fat | -0.17 | 0.08 | -0.17 | 0.07 |
| Arm |
| Skin fat | 0.12 | 0.22 | 0.01 | 0.92 |
| Muscle fat | -0.04 | 0.64 | 0.02 | 0.77 |
| Trunk |
| Skin fat | 0.08 | 0.37 | 0.16 | 0.11 |
| Muscle fat | -0.04 | 0.64 | -0.04 | 0.66 |
| Leg |
| Skin fat | 0.07 | 0.44 | 0.06 | 0.50 |
| Muscle fat | -0.14 | 0.14 | -0.12 | 0.20 |
| Others |
| Pulse | -0.12 | 0.22 | 0.10 | 0.31 |
| O2 % | 0.27 | 0.005* | 0.04 | 0.69 |
| Chest size | 0.27 | 0.005* | 0.003 | 0.97 |
| Hip size | 0.27 | 0.005* | 0.01 | 0.88 |
| CHR | 0.01 | 0.89 | -0.05 | 0.11 |
| WHR | 0.30 | 0.002* | 0.62 | 0.27 |
*Significant (<0.05); VF: Visceral fat; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; CHR: Chest hip ratio; WHR: Waist hip ratio; BMI: Body mass index
There was poor correlation of SBP and DBP with TF and the association was not significant. SBP and DBP were mildly correlated with BMI (p<0.05). And with the whole body VF, the correlation of SBP was moderate and significant. DBP was correlated with whole body VF and correlation was significant. But the whole body, trunk, leg SF and MF were not having significant correlation with SBP and DBP. With the pulse rate also, there was no significant correlation. Finger to heart distance was positively correlated with SBP (p<0.05) but no correlation with DBP. O2 %, chest and hip size were positively correlated with SBP (p<0.05). But the correlation with DBP was not significant. Only whole body VF and WHR were significantly (p<0.05) affected in SBP [Table/Fig-4]. None of the parameters affected DBP except BMI and VF.
Regression analysis SBP as outcome.
| Parameters | Beta coefficient | p-value |
|---|
| (Constant) | 54.08 | |
| BMI | 0.38 | 0.53 |
| VF | 0.57 | 0.005* |
| O2% | 0.07 | 0.52 |
| Chest | -0.10 | 0.87 |
| Hip | 0.19 | 0.73 |
| WHR | 10.09 | 0.002* |
*Significant; VF: Visceral fat; WHR: Waist hip ratio; BMI: Body mass index
Discussion
One of the leading risk factor for chronic arterial HTN is obesity [12]. Various efforts have been made by previous studies to find a correlation between various anthropometric index and BP and also incidence or prevalence of HTN when used to define obesity. A positive correlation was found between the prevalence of elevated BP and increasing adipose tissue by Mark AL et al., [13]. It was stated by Fuchus FD et al., that prediction of the incidence of HTN was even better with the correction of waist by stature or hip circumference than that of BMI [14]. Also, there were claims by Ghosh JR and Bandyopadhyay AR that both SBP and DBP as continuous variables have a stronger correltaions with BMI and WC than with other anthropometric indices [15]. Also, in the present study VF and BMI was significantly correlated with SBP and DBP [Table/Fig-3]. Obesity or excess relative weight is found to be associated with increased risk of disease morbidity and mortality [16]. BMI is widely accepted as one of the best indicator of nutritional status in adults [17,18] The importance of BMI and skinfolds has been recognised for estimating CVD risk factors, particularly due to their positive association with HTN [19]. Amongst the adult Brazilian men there was a significant linear correlation between both SBP and DBP for all anthropometric measurements and with higher BMI, WC and various skin fold locations there was increase in BP seen [20]. A significant positive correlation of BMI with SBP and DBP was earlier reported by many investigators [19,21,22]. Some studies suggested that general adiposity was more strongly correlated with BP [23,24], while other studies suggested central or visceral adiposity was more strongly correlated with BP than general adiposity [25,26]. VF is an important component and has been shown to be associated with a greater cardio metabolic risk, as compared with subcutaneous fat and other obesity measurements, including BMI [27-29]. But in the present study, there was no significant correlation of BP (SBP/DBP) with TF and SF or MF of different regions (whole body, arm trunk, leg). VF and WHR were significant predictors of change in SBP [Table/Fig-4]. Kurniawan LB et al., demonstrated that BW, BMI, WC, BF and VF had a significant correlation with insulin resistance but BW, BF and VF had a slightly better predictor value [30]. Bluher S et al., reported that BMI and WC were best predictors of cardiometabolic comorbidities in obese pubertal adolescents [31]. The WC was strongly associated with glucose and lipid disturbance in obese subjects.
Limitation(s)
Sample size in the study was small, including only healthy young adult population, thus for external validity of results, further study on a larger population including a wider age group of individuals is suggested.
Conclusion(s)
Present study conclude that BMI, VF and WHR had significant correlation with systolic and diastolic BP. VF and WHR were significant predictors of change in SBP. So, fat management is necessity for BP management.
V Fat: Visceral fat; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; CHR: Chest hip ratio; WHR: Waist hip ratio; BMI: Body mass index
*Significant (<0.05); VF: Visceral fat; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; CHR: Chest hip ratio; WHR: Waist hip ratio; BMI: Body mass index
*Significant; VF: Visceral fat; WHR: Waist hip ratio; BMI: Body mass index
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 05, 2020
Manual Googling: Jun 29, 2020
iThenticate Software: Jul 31, 2020 (21%)
[1]. Organisation WH. Obesity: Preventing and managing the global epidemic: World Health Organisation; 2000 [Google Scholar]
[2]. Pradeepa R, Anjana RM, Joshi SR, Bhansali A, Deepa M, Joshi PP, Prevalence of generalized & abdominal obesity in urban & rural India-the ICMR-INDIAB Study (Phase-I)[ICMR-INDIAB-3]Indian J Med Res 2015 142(2):139/10.4103/0971-5916.16423426354211 [Google Scholar] [CrossRef] [PubMed]
[3]. Pi-Sunyer FX, Health implications of obesityAm J Clin Nutr 1991 53:1595S-603S.10.1093/ajcn/53.6.1595S2031492 [Google Scholar] [CrossRef] [PubMed]
[4]. Larsson B, Svärdsudd K, Welin L, Wilhelmsen L, Björntorp P, Tibblin G, Abdominal adipose tissue distribution, obesity and risk of cardiovascular disease and death: 13 year follow up of participants in the study of men born in 1913Br Med J (Clin Res Ed) 1984 288:1401-04.10.1136/bmj.288.6428.14016426576 [Google Scholar] [CrossRef] [PubMed]
[5]. Mohan V, Deepa R, Obesity and abdominal obesity in Asian IndiansIndian J Med Res 2006 123(5):593-96. [Google Scholar]
[6]. Anchala R, Kannuri NK, Pant H, Khan H, Franco OH, Di Angelantonio E, Hypertension in India: A systematic review and meta-analysis of prevalence, awareness and control of hypertensionJ Hypertens 2014 32(6):117010.1097/HJH.000000000000014624621804 [Google Scholar] [CrossRef] [PubMed]
[7]. Messelbeck J, Sutherland L, Applying environmental product design to biomedical products researchEnviron Health Perspect 2000 108(Suppl 6):99710.1289/ehp.00108s699711121364 [Google Scholar] [CrossRef] [PubMed]
[8]. National Health and Nutrition Examination Survey (NHANES)- Anthropometry [13] Procedures Manual, January 2007 [Google Scholar]
[9]. William D McArdle, Frank I Katch, Essentials of Exercise physiology 2000 2nd editionLippincott William & Wilkins [Google Scholar]
[10]. Houtkooper LB, Lohman TG, Going SB, Howell WH, Why bioelectrical impedance analysis should be used for estimating adiposityAm J Clin Nutr 1996 64:436S-48S.10.1093/ajcn/64.3.436S8780360 [Google Scholar] [CrossRef] [PubMed]
[11]. Roubenoff R, Applications of bioelectrical impedance analysis for body composition to epidemiologic studiesAm J Clin Nutr 1996 64:459S-62S.10.1093/ajcn/64.3.459S8780363 [Google Scholar] [CrossRef] [PubMed]
[12]. Kannel WB, Brand M, Skinner JJ Jr, Dawber TR, McNamara PM, The relation of adiposity to blood pressure and development of hypertension: The Framingham studyAnn Intern Med 1967 67:48-59.10.7326/0003-4819-67-1-486028658 [Google Scholar] [CrossRef] [PubMed]
[13]. Mark AL, Correia M, Morgan DA, Shaffer RA, Haynes WG, Obesity induced hypertension: New concepts from the emerging biology of obesityHypertension 1999 33:537-41.10.1161/01.HYP.33.1.5379931161 [Google Scholar] [CrossRef] [PubMed]
[14]. Fuchs FD, Gus M, Moreira LB, Moraes SR, Wiehe M, Pereira GM, Anthropometric indices and the incidence of hypertension: A comparative analysisObes Res 2005 13:1515-17.10.1038/oby.2005.18416222051 [Google Scholar] [CrossRef] [PubMed]
[15]. Ghosh JR, Bandyopadhyay AR, Comparative evaluation of obesity measures: Relationship with blood pressures and hypertensionSingapore Med J 2007 48:232-35. [Google Scholar]
[16]. Tyagi R, Body composition and nutritional status of the institutionalised and non-institutionalised senior citizensEAA Summer School eBook 2007 1:225-319. [Google Scholar]
[17]. James WP, Ferro-Luzzi A, Waterlow JC, Definition of chronic energy deficiency in adultsEur J Clin Nutr 1988 42:969-81. [Google Scholar]
[18]. Ferro-Luzzi A, Sette S, Franklin M, James WP, A simplified approach of assessing adult energy deficiencyEur J Clin Nutr 1992 46:173-86. [Google Scholar]
[19]. Dua S, Kapoor S, Blood pressure, waist to hip ratio and body mass index among affluent Punjabi girls of DelhiActa Med Auxol 2000 32:153-57. [Google Scholar]
[20]. Cassani Roerta SL, Nobre F, Pazin-Fiho A, Schmidt A, Relationship between blood pressure and anthropometry in a cohort of Brazilian men: A cross-sectional studyAm J Hypertens 2009 22:980-84.10.1038/ajh.2009.10419498339 [Google Scholar] [CrossRef] [PubMed]
[21]. Wang H, Cao J, Li J, Chen J, Wu X, Duan X, Blood pressure, body mass index and risk of cardiovascular disease in Chinese men and womenBMC Public Health 2010 10:18910.1186/1471-2458-10-18920384993 [Google Scholar] [CrossRef] [PubMed]
[22]. Ferguson TS, Younger NO, Tulloch-Reid MK, Wright MB, Ward EM, Ashley DE, Prevalence of prehypertension and its relationship to risk factors for cardiovascular disease in Jamaica: Analysis from a cross- sectional surveyBMC Cardiovasc Disord 2008 8:2010.1186/1471-2261-8-2018752689 [Google Scholar] [CrossRef] [PubMed]
[23]. Wang H, Necheles J, Carnethon M, Wang B, Li Z, Wang L, Adiposity measures and blood pressure in Chinese children and adolescentsArch. Dis. Child 2008 93:738-44.10.1136/adc.2007.12758918381342 [Google Scholar] [CrossRef] [PubMed]
[24]. Chen Z, Smith M, Du H, Guo Y, Clarke R, Bian Z, Blood pressure in relation to general and central adiposity among 500 000 adult Chinese men and womenInt J Epidemiol 2015 44:1305-19.10.1093/ije/dyv01225747585 [Google Scholar] [CrossRef] [PubMed]
[25]. Ho SC, Chen YM, Woo JL, Leung SS, Lam TH, Janus ED, Association between simple anthropometric indices and cardiovascular risk factorsInt J Obes Relat Metab Disord 2001 25:1689-97.10.1038/sj.ijo.080178411753592 [Google Scholar] [CrossRef] [PubMed]
[26]. Chandra A, Neeland IJ, Berry JD, Ayers CR, Rohatgi A, Das SR, The relationship of body mass and fat distribution with incident hypertension: Observations from the Dallas Heart StudyJ Am Coll Cardiol 2014 64:997-1002.10.1016/j.jacc.2014.05.05725190234 [Google Scholar] [CrossRef] [PubMed]
[27]. Després JP, Physical activity and the risk of coronary heart diseaseJ Assoc Medicale Can 1989 141:939 [Google Scholar]
[28]. Shah RV, Murthy VL, Abbasi SA, Blankstein R, Kwong RY, Goldfine AB, Visceral adiposity and the risk of metabolic syndrome across body mass index: The MESA studyJACC Cardiovasc Imaging 2014 7:1221-35.10.1016/j.jcmg.2014.07.01725440591 [Google Scholar] [CrossRef] [PubMed]
[29]. Kang SH, Cho KH, Park JW, Yoon KW, Do JY, Association of Visceral fat Area with chronic kidney disease and metabolic syndrome risk in the general population: Analysis using multi-frequency bioimpedanceKidney Blood Press Res 2015 40:223-30.10.1159/00036849825966816 [Google Scholar] [CrossRef] [PubMed]
[30]. Kurniawan LB, Bahrun U, Hatta M, Arif M, Body mass, total body fat percentage and visceral fat level predict insulin resistance better than waist circumference and body mass index in healthy young male adults in IndonesiaJ Clin Med 2018 7:9610.3390/jcm705009629723977 [Google Scholar] [CrossRef] [PubMed]
[31]. Bluher S, Molz E, Wiegand S, Otto KP, Sergeyev E, Tuschy S, Body mass index, waist circumference and waist-to-height ratio as predictors of cardiometabolic risk in childhood obesity depending on pubertal developmentJ Clin Endocrinol Metab 2013 98:3384-93.10.1210/jc.2013-138923775352 [Google Scholar] [CrossRef] [PubMed]