Unilateral Nevus of Ota with Palatal and Optic Disc Pigmentation with Coincidental Preauricular Tag- A Case Report
Prasanna Nareddy1, Ambati Divya2
1 Assistant Professor, Department of Ophthalmology, Santhiram Medical College and Hospital, Kurnool, Andhra Pradesh, India.
2 Resident, Department of Ophthalmology, Santhiram Medical College and Hospital, Nandyala, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Prasanna Nareddy, Flat No. 306, B4, B.K.Singh Towers, Alluri Sitharamaraju Nagar, K.C.Canal, Near Manikanta Ayyappa Swami Temple, KC Canal, Kurnool, Nandyala, Andhra Pradesh, India.
E-mail: prasannan.08@gmail.com
Nevus of Ota also known as oculodermal melanosis presents as hyperpigmentation of face involving ophthalmic and maxillary branches of trigeminal nerve associated with ocular hyperpigmentation. It is due to confinement of melanocytes in the dermis. Most commonly it is unilateral but sometimes it may have bilateral presentation. Typically, it presents at birth but can also be an acquired condition. Frequently seen in Japanese and rarely in Indian subcontinent. It has more predilection towards females. Less frequently, hyperpigmentation is seen in other sites like oral mucosa, tympanum and nasal mucosa. These patients are at high risk of developing glaucoma and malignancy. The author reported a case of 12-year-old male child with unilateral pigmentation of left side face involving forehead, periorbital and cheek, along with ocular pigmentation. Hyperpigmentation of conjunctiva, iris and angles is present in left eye with intraocular pressure being normal in both eyes. Fundus showing optic disc pigmentation in the left eye with cup disc asymmetry in both eyes. Child has coexistent preauricular tag on the left side.
Congenital, Heterochromia iridis, Ocular pigmentation
Case Report
A 12-year-old male child presented with complaints of abdominal pain since 3 days to Paediatric Department where the child was admitted and further evaluation was done. Child was referred to ophthalmology in view of ocular pigmentation. History of bluish discoloration on the left side of face involving forehead, periorbital and malar areas with pigmentation of conjunctiva of left eye was present, since birth [Table/Fig-1]. It was non-progressive. No history of trauma, infections, convulsions, drug intake, exposure to radiation or any other treatment. Antenatal, natal and postnatal history was uneventful. No history of developmental delay. No evidence of pigmentation on other sites of body.
Hyperpigmentation on left side of face.

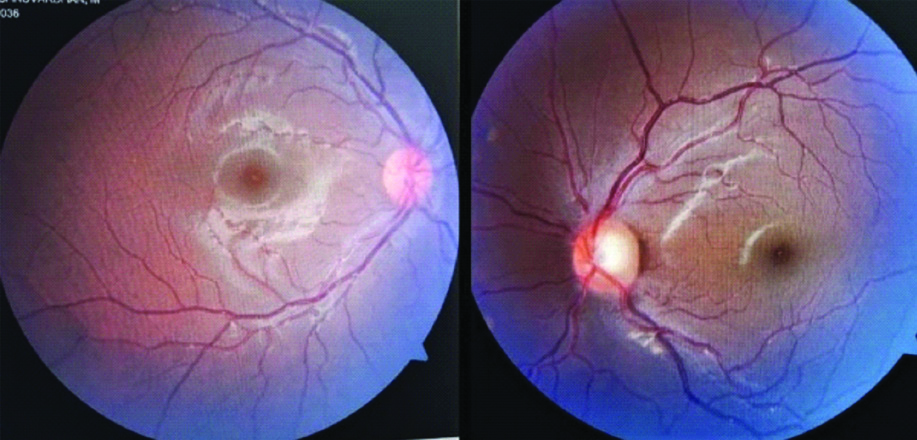
On ophthalmological examination, right eye anterior segment was normal. Left eye showed bluish pigmentation in the periorbital area extending onto the cheeks, with conjunctival pigmentation and heterochromia iridis while other findings being normal [Table/Fig-2]. Posterior segment showed cup disc ratio of 0.2:1 in the right eye and 0.5:1 with mild pigmentation on the disc in the left eye with periphery being normal in both eyes [Table/Fig-3]. Visual acuity in both eyes was 20/20. Intraocular Pressure (IOP) being 12 mm of Hg in right eye and 14 mm of Hg in left eye. Gonioscopy revealed open angles in both eyes with hyperpigmentation of angles in the left eye.
Conjunctival pigmentation of left eye with heterochromia iridis.

Left optic disc pigmentation with cup disc asymmetry in both eyes.
Extraocular examination showed preauricular tag on the left side. Oral examination showed mild palatal pigmentation on the left side [Table/Fig-4]. Child was referred to glaucoma specialist and dermatologist.
Palatal pigmentation and pre-auricular tag.

Taking into consideration of other differentials like sturge weber syndrome, blue nevus, drug induced hyperpigmentation and café-au-lait spots were ruled out.
Sturge weber has typical port wine stain, majority present with history of siezures, where as in this case it’s a dark pigmentation with absent history of seizure. Blue nevus presents as small, well defined plaques or papules which can present anywhere over the body. Drug induced hyperpigmentation is due to intake of drugs like amiodrone, minocycline, gold and can be seen anywhere on the body. Café-au-lait spots also present in the other sites of the body with axillary freckling and cutaneous nodules, which were absent in this case. The typical feature of scleral pigmentation is not seen in above conditions. Based on the history, clinical findings and dermatological conjecture and ruling out the differentials, a diagnosis of Nevus of ota was made.
Discussion
Nevus of ota, also called as oculomucodermal melanosis is the bluish pigmentation of skin and ocular structures. It usually involves the face along the distribution of ophthalmic and maxillary branches of trigeminal nerve. It appears because of confinement of melanocytes in the superficial layers of dermis. It was described by Hulke in 1861 and in 1939 it was first observed in a Chinese patient by Pusey. Masao Ota, a Japanese dermatologist was the first person to name this condition as “Nevus fuscucerulus ophthalmomaxillaris” in 1939 which subsequently came to be called as “Nevus of Ota” [1,2]. It is largely seen in Asian population with an incidence of 0.014-0.034%. Typically, it is unilateral though sometimes bilateral presentation may be seen. Most commonly, it is congenital but can be acquired during adulthood or pregnancy. It has slow progression and usually stabilises by adulthood. It is predominantly seen in females than males with a ratio of 5:1. The pathogenesis is multifactorial. Sometimes predisposing factors like infections, genetics, UV light exposure, trauma or female sex hormones may be the cause in acquired conditions [3]. Ocular pigmentation is seen in eyelids, sclera, cornea, iris and retina. Occasionally, other sites like tympanum (55%), pharynx (25%), nasal mucosa (30%) and palate (20%) are also involved [4]. Though various classifications were proposed, clinical classification given by Tanino H is commonly followed [2].
In ocular pigmentation, conjunctival and iris pigmentation are most evident. In few studies, they have described the iris pigmentation as mammillations of iris, a distinctive feature in oculodermal melanocytosis [5]. They present as small and smooth nodules which are distributed homogenously. Few studies reported that patients with angle pigmentation have high risk of developing raised intraocular pressure and glaucoma later. In a study, it was mentioned that pathogenesis of glaucoma could be either because of angle abnormality due to abnormal neural crest cells or obstruction of trabecular meshwork due to melanocytes [5].
Oral pigmentation has been reported by some authors. It can involve either buccal mucosa or palate. Based on literature research till now, 51 cases have been reported with intraoral involvement worldwide including the present report [6-9]. Present case is about 23rd case with palatal involvement in India [Table-Fig-5] [3,4,7-16].
Comparision of various case reports of Nevus of ota with pigment distribution [3,4,7-16].
| Authors | Age/sex | Cutaneous | Sclera | Hetero chromia iridis | Angles | Fundus | Optic disc | Disc cupping | Intraoral |
|---|
| Maguire J and Holt D [8] | 48/F | U/L | + | - | - | - | - | - | Buccal mucosa, Palate |
| Acaba-Berrocal LA et al., [15] | 51/M | U/L | + | + | - | - | - | - | - |
| Syed MA et al., [7] | 22/F | B/L | + | - | - | - | - | - | Palate |
| Maheshwari R et al., [3] | 23/F | U/L | + | - | - | - | - | - | - |
| Solanki J et al., [13] | 56/M | U/L | + | - | - | - | - | - | Palate |
| Mukhopadhyay AK [4] | 24/M | U/L + Shoulder | + | - | - | - | - | - | Palate |
| Borra K [9] | 30/F | U/L | + | - | - | - | - | - | Palate |
| Cronemberger S et al., [10] | 14 cases | 14 | 14 | 8 | 8 | 6 | 1 | 5 | 1 Palate |
| Kono T et al., [11] | 16 cases | U/L15, B/L1 | 16 | - | - | - | 3 | - | - |
| Swan PG [12] | 29/F | B/L | + | - | - | + | - | - | - |
| Rishi P et al., [14] | 18/F | U/L | + | - | - | - | - | + | - |
| Gupta GP and Gangwar DN [16] | 5/M | Scalp pigment | + | + | - | + | + | - | - |
| 52/F | U/L | + | + | + | + | + | - | - |
| Present case | 12/M | U/L | + | + | + | - | + | + | Palate |
+Present; -Absent; U/L- Unilateral; B/L- Bilateral; F- Female; M-Male
There are few studies which reported palatal pigmentation, but optic disc pigmentation with disc cupping has been reported in very few cases till now. Few reports have mentioned about the fundus pigment mottling as a feature but reports showing optic disc pigmentation were rare [10-12]. According to literature, till now 11 cases of optic disc pigmentation including the present case were reported worldwide. In India, about 3 cases reported till date including the present one [10-12]. In this case, preauricular tag was coincidentally noticed.
The possible differentials for nevus of ota could be sturge weber syndrome, blue nevus, melasma, café-au-lait spots of neurofibromatosis, actinic lentigo and drug induced pigmentation. Melasma is pregnancy associated with bilateral presentation and absent palatal and fundus pigmentation [3]. Others like Mongolian spot where spot is usually seen in lumbosacral area and resolves by the age of 3-6 years, with absent pigmentation on face. Differential for oral pigmentation can be oral melanotic macule which is small in size and is not associated with scleral pigmentation [13].
Ocular complications are predominantly glaucoma (10%) and melanoma (1 in 400) [14]. Patients with angle pigmentation are at high risk of developing glaucoma in future. The risk of uveal melanoma increases with oculodermal melanocytosis. A 3% of patients with uveal melanoma have oculodermal melanosis which is thought to be the precursor of malignancy. The risk of uveal melanoma metastasis in these patients is 1.6 times more than with those without oculodermal melanocytosis [15].
Conclusion(s)
This report is an infrequent case of nevus of ota with palatal pigmentation and optic disc pigmentation. Even though, the probability of developing glaucoma and malignancy is less, it would be prudent to advise an annual follow-up and screening for these two conditions by an ophthalmologist and if needed by dermatologist. Based on the clinical presentation with preauricular tag, it is assumed that nevus of ota could be part of bigger picture, probably an unidentified syndromic presentation.
+Present; -Absent; U/L- Unilateral; B/L- Bilateral; F- Female; M-Male
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? NA
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Apr 16, 2020
Manual Googling: Jun 26, 2020
iThenticate Software: Jul 31, 2020 (8%)
[1]. Ota M, Nevus fuscoceruleus ophthalmomaxillarisTokyo Med J 1939 63:1243-45. [Google Scholar]
[2]. Tanino H, Nevus fuscoceruleus ophthalmomaxillaris OtaJpn J Dermatol 1939 46:435-51. [Google Scholar]
[3]. Maheshwari R, Desai V, Sunil Kumar MV, Gaurav I, Unilateral nevus of ota: A case report of oculodermal melanocytosis!J Dent Allied Sci 2016 5:39-42.10.4103/2277-4696.185192 [Google Scholar] [CrossRef]
[4]. Mukhopadhyay AK, Unilateral nevus of ota with bilateral nevus of Ito and palatal lesion: A case report with a proposed clinical modification of tanino’s classificationIndian J Dermatol 2013 58:286-89.10.4103/0019-5154.11394323918999 [Google Scholar] [CrossRef] [PubMed]
[5]. Plateroti AM, Scavella V, Abdolrahimzadeh B, Plateroti R, Rahimi S, An update on oculodermal melanocytosis and rare associated conditionsSeminars in Ophthalmology 2016 32(4):524-28.10.3109/08820538.2015.111813327083007 [Google Scholar] [CrossRef] [PubMed]
[6]. Pedraza E, Cicero-Casarrubias A, García-de la Cruz JJ, Méndez-Flores S, Fernández-Cuevas L, Nevus of ota with intraoral involvement: Case report and review of the literatureJournal of Dental and Maxillofacial Surgery 2018 1(1):26-32.10.18314/jdms.v1i1.1192 [Google Scholar] [CrossRef]
[7]. Syed MA, Amatya B, Alam S, Bilateral nevus of OtaPigment Int 2018 5:120-22. [Google Scholar]
[8]. Maguire J, Holt D, Nevus of Ota- An intraoral presentation: A case reportJ Med Case Reports 2019 13:17410.1186/s13256-019-2101-031171040 [Google Scholar] [CrossRef] [PubMed]
[9]. Borra K, Nevus of Ota in a young female- A case reportInt J Sci Res 2020 9(1):1495-97. [Google Scholar]
[10]. Cronemberger S, Calixto N, Freitas HL, Nevus of Ota: Clinical-ophthalmological findingsRev Bras Oftalmol 2011 70(5):278-83.10.1590/S0034-72802011000500002 [Google Scholar] [CrossRef]
[11]. Kono T, Kurome H, Shibuya Y, Ocular findings in Japanese women with nevus of OtaGraefe’s Arch Clin Exp Ophthalmol 1995 233:667-71.10.1007/BF001646678566821 [Google Scholar] [CrossRef] [PubMed]
[12]. Swann PG, The fundus in oculodermal melanocytosis Is this a new observation?Clin Exp Optom 2003 86(3):183-86.10.1111/j.1444-0938.2003.tb03101.x12767253 [Google Scholar] [CrossRef] [PubMed]
[13]. Solanki J, Gupta S, Sharma N, Singh M, Bhateja S, Nevus of ota”- A rare pigmentation disorder with intraoral findingsJ Clin Diagn Res 2014 8(8):ZD49-50.10.7860/JCDR/2014/9978.477225302286 [Google Scholar] [CrossRef] [PubMed]
[14]. Rishi P, Rishi E, Bhojwani D, Giant nevus of OtaIndian J Ophthalmol 2015 63(6):532-33.10.4103/0301-4738.16260726265645 [Google Scholar] [CrossRef] [PubMed]
[15]. Acaba-Berrocal LA, Bekerman VP, Shields CL, Oculodermal Melanocytosis: Not to be overlookeRetina today 2017 :41-43. [Google Scholar]
[16]. Gupta GP, Gangwar DN, Naevus of OtaBr J Ophthalmol 1965 49(7):364-68.10.1136/bjo.49.7.3645828913 [Google Scholar] [CrossRef] [PubMed]