Incidental Detection of Microfilaria in Fine Needle Aspiration Cytology- A Report of Three Cases
Gayatri Rath1, Ashok Kumar Panda2
1 Assistant Professor, Department of Pathology, S.C.B Medical College, Cuttack, Odisha, India.
2 Consultant Nephrologist, Department of Nephrology, Care Hospital, Bhuabneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Gayatri Rath, N4/288, IRC Village, Nayapalli, Bhubaneswar-751015, Odisha, India.
E-mail: swagatpanda339@gmail.com
Lymphatic filariasis, a major global health problem, is a mosquito-borne parasitic disease, encountered mainly in the tropics and subtropics. The disease is endemic in Southeast Asia, including the Indian subcontinent. It is transmitted by mosquitoes and is caused by the filarial nematodes Wuchereria bancrofti, Brugia malayi and Brugia timori. Usually, the infected person remains asymptomatic for years together and later manifests with features and consequences of lymphatic obstruction. The adult forms of the nematodes live in human lymphatics, whereas the infective larval form, the microfilaria circulates in the peripheral blood. The nocturnal periodicity of the microfilaria makes it challenging to detect in routine peripheral blood smear examinations. Also, it is quite unusual to find the microfilaria in fine needle aspirations. However, rare cases have been reported in certain unusual sites, like lymph nodes, cutaneous swellings, bone marrow, bronchial aspirate, breast, nipple discharge, cervicovaginal smears, pleural, pericardial, ascitic fluids, ovarian cyst fluids or even thyroid. Very few cases of microfilaria in thyroid aspirates have been reported till date. Also, it is unusual to find microfilaria in lymph node and breast aspirations. Herewith, three cases of microfilariasis are reported at three uncommon sites like thyroid, lymph node and breast.
Breast, Lymph node, Thyroid
Introduction
Filariasis is an infectious disease, prevalent in both rural and urban regions. It is a significant health problem in tropical countries like India. Individuals get infected by the bite of Culex mosquitoes. Majority of infected individuals do not show any symptoms for a long period of time [1]. The adult worm lives in lymphatic vessels of the definitive host, and the microfilaria circulates in the peripheral blood. It is a challenge to find microfilaria in routine peripheral blood smears, fine needle aspirations and body fluids, despite its high incidence in the tropical zone because of its nocturnal periodicity [2]. In the present series three cases are reported showing unusual sites for microfilaria.
Case Series
Case 1
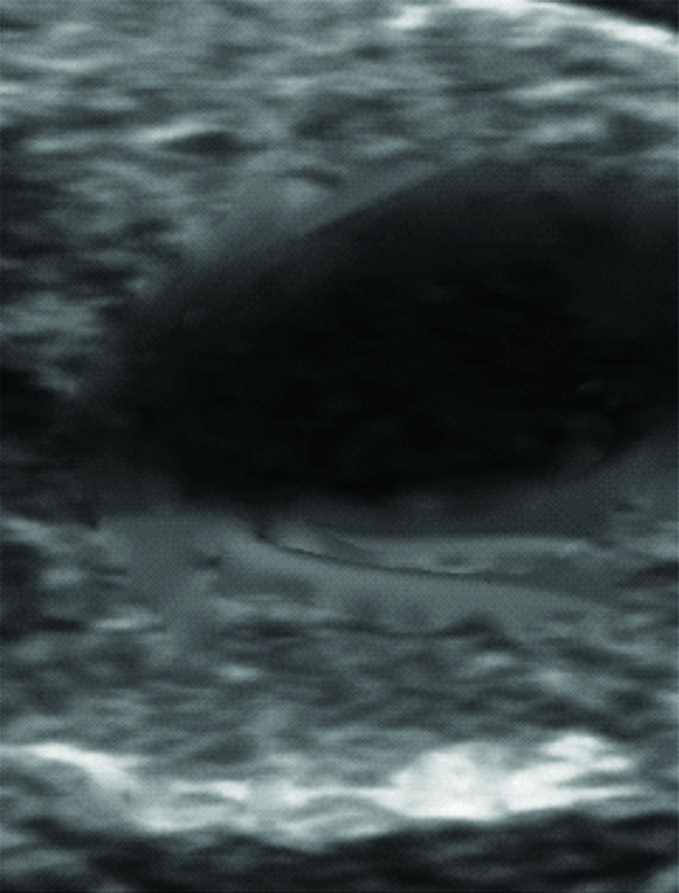
A 32-year-old female patient attended the Ear Nose Throat (ENT) Out Patient Department (OPD) with a solitary thyroid nodule of eight months duration. She did not have any associated co-morbidity. On local examination, the swelling measured about 4×3×1 cm, was soft to firm, non-tender and was moving with deglutition. She was clinically diagnosed to have colloid goitre. Routine haematological investigations showed Total Leukocyte Count (TLC) to be 6,200/ cmm of blood. The differential count showed mild eosinophilia with eosinophil count 14% and total eosinophil count 870/ cmm of blood. Erythrocyte Sedimentation Rate (ESR) was 22mm in the first hour. Thyroid serology was normal. Ultrasonography of the thyroid showed a single large cystic mass lesion in the right lobe with provisional diagnosis of nodular colloid goitre [Table/Fig-1]. Fine Needle Aspiration Cytology (FNAC) was done using a 23 gauge needle and a 10 mL syringe. Smears were stained with Giemsa stain. Cytosmears revealed benign follicular epithelial cells in clusters and singles, macrophages, blood mixed colloid background. Higher magnifications showed microfilaria, with the presence of a hyaline sheath, a cephalic and a caudal space, somatic cells which appeared as granules throughout the body [Table/Fig-2]. A diagnosis of Wuchereria bancrofti filaria in the thyroid was made. Patient was advised Diethylcarbamazine (DEC) for 21 days. The cycle was repeated after that and the patient followed-up to six months. The patient responded well to the therapy with subsidence of swelling after three months.
Ultrasonographic image showing a large cystic lesion in the right lobe of the thyroid.
Microphotograph showing microfilaria with clusters of thyroid follicular epithelial cells, macrophages on a blood mixed thin colloid background. (Giemsa stain x40).

Case 2
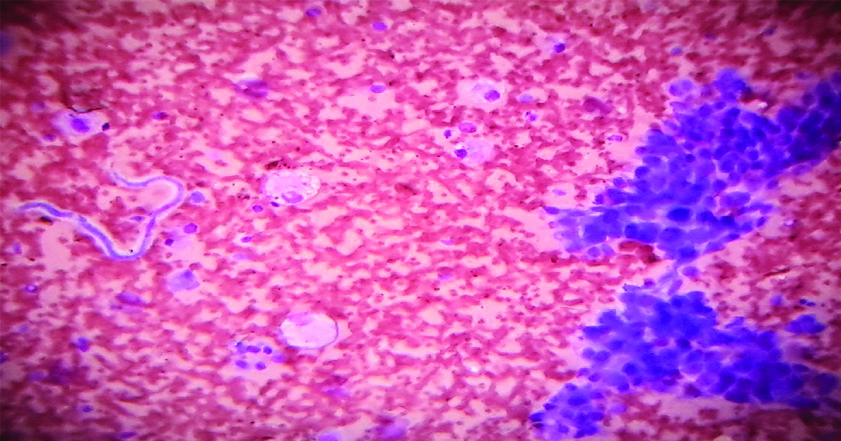
A 30-year-old male, presented with intermittent low grade fever for past two months and enlargement of the left upper cervical lymph node for last six months. Clinical diagnosis was tuberculosis of lymph node. On examination, the lymph node measured 2×2×1 cm was firm and non-tender. The routine investigations revealed TLC to be 11200 per cubic mm of blood; Differential count was within normal limits. Association of fever and lymph node enlargement raised the possibility of tuberculosis. FNAC was done from the node. Cytosmears stained with Giemsa stain revealed scattered lymphoid cells and microfilaria over a haemorrhagic background [Table/Fig-3]. Detection of microfilaria was an incidental finding. He was treated with Diethylcarbamazine for a period of three weeks. The cycle was repeated after that and the lesion subsided. The patient was followed-up till six months.
Microphotography shows ensheathed, coiled and curved microfilaria with scattered mature lymphocytes on a haemorrhagic background. (Giemsa stain x40).

Case 3
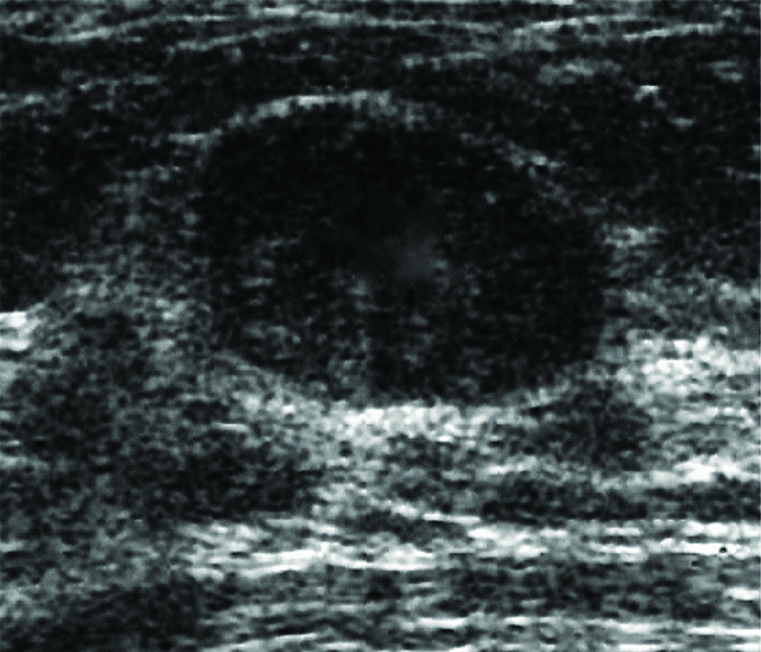
A 36-year-old female presented with the complaints of a painless left breast mass of one month duration. She had no other associated symptoms. Clinical diagnosis was fibroadenoma of left breast. Her general examination findings were normal except mild pallor. Breast examination findings revealed a firm, mobile lump of size 2×2×1 cm in the upper outer quadrant of left breast. Ultrasonography showed a hypo-echoic lesion with relatively sharp margin [Table/Fig-4]. There were also no palpable axillary lymph nodes. Routine haematological findings were within normal limits. The lump was aspirated and smears stained with Giemsa stain. Microscopic examination findings revealed benign ductal epithelial cells in large clusters and singles, cyst macrophages and sheathed microfilaria of Wuchereria bancrofti [Table/Fig-5]. So, a diagnosis of filarial breast lump was made based on cytomorphology, which was also an incidental finding. She was treated with DEC for a period of three weeks and the lesion subsided completely within a month.
Ultrasonographic picture showing a hypo-echoic lesion with relatively sharp margin.
Cytosmear shows clusters of ductal epithelial cells, cyst macrophages and ensheathed microfilaria on a haemorrhagic background. (Giemsa stain x40).
Discussion
According to the present scenario, about 120 million people in 81 countries are infected with lymphatic filariasis. About 1.34 billion people live in endemic and high risk areas. In India about 370 million people are at the risk of contracting filarial infection [3]. The disease is caused by the nematodes and is transmitted by the bite of Culex mosquito. The life cycle of the common species, Wuchereria bancrofti, is found in two hosts. Man is the definitive and mosquito, the intermediate host. The adult worm resides in lymph vessels and frequently causes inflammation and obstruction leading to lymphedema, lymphangiovarix and fibrosis. Filariasis causes a spectrum of diseases starting from asymptomatic microfilaremia to acute lymphangitis, acute and chronic lymphadenitis, oedema of limbs and genitalia and tropical pulmonary eosinophilia [4]. Despite the high incidence and prevalence and a wide variety of tissue affection, it is unusual to find microfilaria in FNAC smears. Diagnosis of lymphatic filariasis is made by demonstration of microfilaria in peripheral blood smear examination [5]. In the case no-1, the patient presented with thyroid swelling of eight months duration, which was clinically and radiologically diagnosed as nodular colloid goitre. Thyroid serology however was normal. Detection of microfilaria in the thyroid aspirate was an incidental finding. There were no signs and symptoms of filarial infection and also no other associated co-morbidity. Peripheral blood smear examination showed absence of microfilaria, which rules out possible contamination from the blood. So it might have been due to possible rupture of the blood vessel by the invasion of the microfilaria. Some researchers have attributed the presence of microfilaria in thyroid aspirates to lodging and rupture of thyroid blood vessels [6]. Kundu AK et al., reported microfilaria in a solitary thyroid nodule of a woman aged 38 years [7]. Case 2 presented with fever and lymphadenopathy and was clinically suspected as a case of tuberculosis, which after aspiration of the lymph node showed the incidental presence of microfilaria. Although filariasis is common in tropical countries including India, it is rare to find microfilaria in lymph node cytology. Lymphadenitis never raises a suspicion for filariasis. It has always been detected incidentally while doing FNAC of enlarged lymph nodes for evaluation of other lesions. Similarly, case 3 presented with a breast mass which was diagnosed clinically as fibroadenoma. After aspiration, it was found out to be filarial breast mass. Filariasis involving breast is a rare occurrence. Peculiarity of the present case was that, the peripheral blood eosinophil count was normal, whereas Khan R et al., reported peripheral blood eosinophilia [8]. Dayal A and Seivaraju K reported that chronic inflammation and fibrosis due to disruption of lymphatic vessels was the cause of filarial breast nodule [9]. Thorough screening of the cytology smears should be carried out in all cases. This will help in targeted therapy and avoid undue delay in further management.
Conclusion(s)
Presence of microfilaria in blood and lymphatic system is a common occurrence. Present series is unique in a sense that microfilaria was detected at unusual sites like Thyroid, Breast and Lymph node using simple techniques like FNAC. The detection of microfilaria in all these cases were incidental. This study underlines the importance of careful screening of the patients from endemic regions of lymphatic filariasis even at unusual sites.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 13, 2020
Manual Googling: Jun 29, 2020
iThenticate Software: Jul 28, 2020 (10%)
[1]. Mitral SK, Mishra RK, Verna P, Cytological diagnosis of microfilaria in filarial endemic areas of eastern Uttar PradeshJ Cytology 2009 26:11-14.10.4103/0970-9371.5133321938142 [Google Scholar] [CrossRef] [PubMed]
[2]. Choudhury M, Langer S, Aggarwal M, Agrawal C, Microfilaria in thyroid gland noduleIndian J Pathol Microbiol 2008 51:94-96.10.4103/0377-4929.4041518417874 [Google Scholar] [CrossRef] [PubMed]
[3]. WHO (2015), Global Programme to eliminate lymphatic filariasis: Progress Report, September, 2016 [Google Scholar]
[4]. Macadam AJ, Sharpe HA, Infectious diseases. In: Kumar V, Abbas AK, Fausto N, editorsRobbins and Cotran Pathologic Basis of Disease 2007 7th EdPhiladelphiaElsevier [Google Scholar]
[5]. Rawat V, Rizvi G, Sharma N, Pandey H, An unusual presentation of Wuchereria bancrofti infectionIndian J Med Microbiol 2009 27:382-83.10.4103/0255-0857.5544219736421 [Google Scholar] [CrossRef] [PubMed]
[6]. Varghese R, Raghuveer CV, Pai MR, Bansal R, Microfilaria in cytologic smears; A report of six casesActa Cytol 1996 40:299-301.10.1159/0003337558629415 [Google Scholar] [CrossRef] [PubMed]
[7]. Kundu AK, Giri A, Ghosh G, Saha SR, Microfilaria in a thyroid nodule that resolved on treatmentTropical Doct 2002 32:24810.1177/00494755020320043112405321 [Google Scholar] [CrossRef] [PubMed]
[8]. Khan R, Harris SH, Maheswari V, Filarial breast mouseJ Coll Physicians Surg Pak 2011 21:513 [Google Scholar]
[9]. Dayal A, Seivaraju K, Filariasis of the breastWebmed Cent Surg 2010 1:WMC00942 [Google Scholar]