Introduction
Special needs children experience poorer oral health when compared to their compatriots. Moreover, Special Care School Children (SCSC) experience significant barriers to access proper oral health care. It has been found that they have high unmet oral health needs.
Aim
The aim of this study was to assess the effectiveness of preventive oral health measures in a group of SCSC; boys, in Al-Kharj Governorate of Saudi Arabia.
Materials and Methods
A longitudinal study was designed among SCSC in Al-Kharj Governorate of Saudi Arabia starting from October 2016 for a period of eight months. Only schools for boys were included in the study. Out of 936 students enrolled in the special needs education programme in 18 boys schools; 163 SCSC (boys) from eight primary schools were eventually included in the study. After the base line survey; the subjects were evaluated with predefined criteria at three monthly intervals until six months. The effectiveness of various preventive measures was evaluated for reduction in the risk of oral diseases. SCSC were divided into groups as per their specific health care need. Preventive oral health measures such as supervised tooth brushing with a fluoridated tooth paste was introduced with the help of teachers and parents of SCSC. Plaque levels were assessed by means of Plaque index. Various indices were used to measure dental caries including Decayed, Missing, and Filled Teeth (DMFT/dmft) as well as Decayed, Missing, and Filled Surfaces (DMFS/dmfs) index. The risk for dental caries was assessed by means of a cariogram model at the start and at the end of campaign. The data was computed using SPSS v20 programme. Means of the overall plaque score and the caries indices scores were calculated and compared among various special need groups among the SCSC. The significance level was set at p<0.05.
Results
The overall mean plaque score of the group was 1.55. Plaque scores and mean decayed (D) component were significantly higher in intellectual disabilities as compared to physical disabilities. The mean DMFT and DMFS score was 3.2 and 6.42, respectively with mean decayed (D) component score of 2.67. There was no significant difference among caries prevalence and decayed (D) component among various groups of disabilities. Plaque index score reduced to 1.35 after three months and finally to 1.1 after six months. This was statistically significant (p<0.05). The actual chance to avoid new cavities in the cariogram increased from 5% to 73% at the end, for the SCSC boys.
Conclusion
There was a significant decrease in the risk for oral diseases after incorporation of preventive oral health measures for SCSC.
Introduction
‘Individuals with Special Health Care Needs’ (ISHCN) is a term that encompasses a wide variety of physical, developmental, and intellectual impairments that mandates health care interventions and/or specialised health care programmes [1]. There is an impact of special health care needs on the quality of life including oral health and may be compounded by barriers in communication [1,2]. Most of the special health care needs are either present at birth or develop in the early few years of life [3]. The Children with Special Health Care Needs (CSHCN) present a challenge to the dental team as many of them have high unmet oral health needs [4-9]. Moreover, CSHCN are either dependent on parents, siblings or caregivers for their care including diet and oral hygiene maintenance [10]. In spite of increased services provided for CSHCN in recent years, there are still significant barriers that exist especially for their oral health care. [11,12]. However, it has been shown that oral health related quality of life for CSHCN can be improved by better oral health services utilisation [13,14]. The transition from childhood to adulthood presents further difficulties in terms of appropriate oral health care for ISHCN [15]. Since education is an important part of the development of an individual within a society, there has been an emphasis of imparting education to CSHCN, taking into consideration their specific health care needs. Special Care School Children (SCSC) are provided with special education in various forms according to their specific needs among various societies [16]. However, SCSC continue to have high oral health unmet needs and their condition in terms of oral health care is not much different from other CSHCN [17]. Therefore, it is important that preventive oral health programmes should be initiated as early as possible [18]. Huebner CE et al., noted that the majority of the parents of SCSC do not follow minimal recommendations and guidelines set for the preventive dental care for their children, especially at home [19]. A similar study in Al-Kharj, Saudi Arabia with a different age group found out that there was a high level of dental caries and unmet need including retained deciduous teeth among such individuals [20]. Therefore, the aim of the present study was to assess the effectiveness of preventive oral health measures for reduction in the risk of oral diseases in a group of SCSC boys.
Materials and Methods
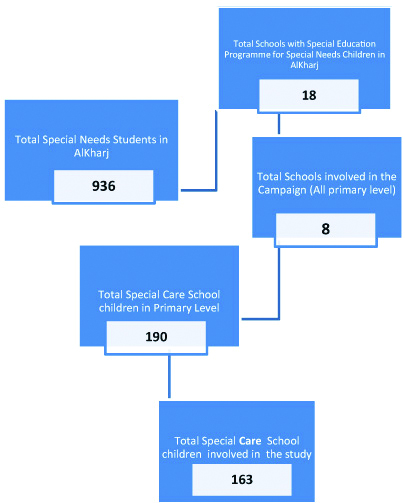
A longitudinal study was conducted starting from October 2016 for a period of eight months in Al-Kharj governorate of Saudi Arabia including the training and calibration of examiners. There were an overall 936 SCSC in 18 boys’ schools that have programmes for special education and accommodate SCSC as per their specific needs. Only primary level schools were involved in the study. Eight primary schools were chosen randomly by random number table from the list of schools. Out of the potential 190 SCSC boys, eventually 163 boys aged between 6-15 years participated in the study. The list of SCSC, studying in the selected eight primary schools was used to send passive consent letters for parents/guardians for the involvement of their wards in the study. The school children who were not listed as SCSC were excluded. If the parents or the guardians sent a signed consent letter not willing their wards to be included, those SCSC were also excluded. There were some SCSC who were very uncooperative and were eventually excluded from the study. [Table/Fig-1] describes the process of inclusion and exclusion for the sample selection. The reason for boys only sample was due to the fact that there is segregation of gender in schools in Saudi Arabia and it was not possible to enrol the female students, as they have separate schools where males do not have access. After the incorporation of the inclusion and exclusion criteria and knowing the overall SCSC in the province, a combination of randomisation and stratification of the sample over the actual population was used. However, it was ensured that the sample represents an effective size for the scientific interest. The sample size was estimated considering the analytical plan, and level of confidence (p≤0.05).
Sampling process for Special Care School Children (SCSC).
Ethical Approval, School Permission and Consent
The copy of the passive consent letter in Arabic language to be distributed to the parents/guardians of SCSC was attached with the proposal for ethical clearance. The letter asked the Parents/guardians to sign and return the letter stating their refusal in case they were not willing their ward to be the part of this study. As a source of motivation powered toothbrushes and toothpastes were provided by the research team both at the schools and for home use. A formal ethical approval was granted by the Ethics committee at College of Dentistry, Prince Sattam bin Abdulaziz University; Al-Kharj vide no PSAU/Dent-CFR/1430. Permission was sought and granted by respective authorities from the Ministry of Education, Special needs education programme who also gave the data about special education programme as well as the details of SCSC in Al-Kharj province of Saudi Arabia
The selected SCSC were grouped according to their medical diagnosis after confirmation with the teachers that their respective parents/guardians did not have any objection by means of a passive consent letter. [Table/Fig-2] describes the various special needs of the SCSC as per the medical diagnosis mentioned against their respective names. Supervised tooth-brushing programme with a powered toothbrush brush and commercially available fluoridated (1450 ppm), Colgate Dental Cream®, tooth paste was provided by the research team for once daily use at home and once at the school through parents and teachers of SCSC. The parents were instructed about the use of powered tooth brush and were advised to assist the child to brush once daily before sleep. The teachers were given training about the use of powered tooth brushes as well and instructed how to assist the SCSC for tooth brushing once daily at the school at any convenient time before the school was over. Both the teachers and parents were trained in specifically making modifications according to the disability and the special health care need of the SCSC. After baseline examination and recording, the SCSC were examined again after 3 months and finally at 6 months. The supervised tooth brushing with a fluoridated toothpaste twice daily; once at home and once at school, was recommended as an evidence based method for effective plaque control and caries reduction [21].
SCSC with their baseline assessment for Plaque and Caries exposure.
| Associated disability | Baseline assessment |
|---|
| N (%) | | Plaque score (baseline) | Caries prevalence DMFT | Caries severity DMFS | Decayed (D) component |
|---|
| Visually impaired | 8 (4.9) | Mean | 1.5 | 3 | 4.5 | 3 |
| Std. deviation | 0.756 | 2.268 | 3.891 | 2.268 |
| Hearing impaired | 20 (12.3) | Mean | 1.2 | 2.65 | 4.5 | 2.05 |
| Std. deviation | 0.865 | 3.167 | 5.717 | 3.17 |
| Hearing and speech impairment | 21 (12.9) | Mean | 1.02 | 3.14 | 4.29 | 2.67 |
| Std. deviation | 0.59 | 3.291 | 5.041 | 2.817 |
| Down’s syndrome | 33 (20.2) | Mean | 1.55 | 2.27 | 4.45 | 2.03 |
| Std. deviation | 0.754 | 2.295 | 5.701 | 2.201 |
| Learning disability | 48 (29.4) | Mean | 1.52 | 3.77 | 8.52 | 2.98 |
| Std. deviation | 0.989 | 3.827 | 13.006 | 3.461 |
| Attention deficit hyperactivity disorder | 8 (4.9) | Mean | 1.88 | 3.38 | 7.63 | 3.38 |
| Std. deviation | 0.354 | 3.998 | 9.913 | 3.998 |
| Autism | 20 (12.3) | Mean | 1.85 | 3.5 | 5.5 | 3.3 |
| Std. deviation | 0.988 | 3.154 | 5.145 | 3.063 |
| Multiple disability | 5 (3.1) | Mean | 1.9 | 5.2 | 20.8 | 2.4 |
| Std. deviation | 0.548 | 4.764 | 19.202 | 3.286 |
| Total | 163 (100) | Mean | 1.55 | 3.2 | 6.42 | 2.67 |
| | Std. deviation | 0.932 | 3.3 | 9.458 | 3.018 |
DMFT: Decayed, Missing, and Filled Teeth; DMFS:Decayed, Missing, and Filled Surfaces
World Health Organisation (WHO) basic oral health survey 2013 was used as criteria for the diagnosis of oral health issues [22]. DMFT/dmft and DMFS/dmfs indices were used to measure prevalence and severity of dental caries, respectively. The decayed component of DMFT/dmft index was used to measure the treatment needs of dental caries. The plaque scores were measured by utilising Silness-Loe Plaque index [23]. All the scores were taken at base-line, then at three months interval and finally at six months.
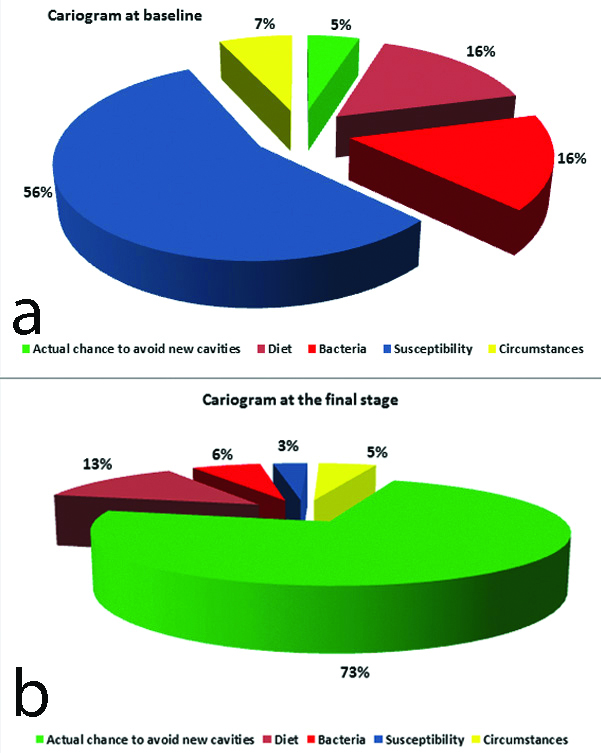
Risk for dental caries was determined by the Cariogram model. The cariogram model is based on Caries Risk Test (CRT) involving estimation of salivary bacterial counts. This model involves diet, circumstances, bacteria and susceptibility of an individual to determine the chances of avoiding new carious lesions or cavities. The changes in these factors effected by preventive oral health measures were estimated using the same model at the completion of the study [24,25]. The average estimated cariogram was compared at six months from the baseline data taken at the initial oral health survey of the groups within the sample.
Training and Calibration of Examiners
Prior to the commencement of the main study, four examiners were standardised and calibrated to ensure uniform interpretations, and application criteria for indices. The selected examiners were labelled as Examiner A, Examiner B, Examiner C and Examiner D. All examiners underwent training about indices and WHO survey methods 2013 [22]. The overall reliability of the examiners was assessed after two weeks. It was found to be 95.5% for dental caries and 98 % for Plaque Index. Furthermore, calibration was done at the third week to seek the intra-examiner and inter-examiner variability. Overall Kappa score of 0.96 was achieved for intra-examiner variability and 0.91 for inter-examiner variability.
Statistical Analysis
The data was entered and analysed using the Statistical Package for Social Sciences (SPSS) version 20 programme. The data were analysed as means of the overall scores. Analysis of variance (ANOVA) and Chi-square tests were used for comparisons. A p-value of less than 0.05 was considered as statistically significant.
Results
A total of 163 SCSC were eventually screened after the sampling process [Table/Fig-1]. The majority among the SCSC was the group with learning disability accounting for nearly 29.4% while as some SCSC had multiple disabilities like Learning disability with a physical disability or Attention Deficit Hyperactivity Disorder (ADHD). These were grouped as ‘Multiple Disability’ group and represented 3.1% of the total SCSC.
[Table/Fig-2] shows the distribution of the group as per their medical diagnoses with plaque scores and dental caries status at the baseline. The dental caries is shown as the mean per each group in terms of prevalence (DMFT/dmft), severity (DMFS/dmfs) and the treatment need (decayed component of DMFT/dmft). The average mean plaque score at base line was 1.55 (SD±0.93) for the whole group. The ‘Hearing and speech Impairment’ group had lower average mean plaque score of 1.02 (SD±0.59) when compared to average plaque score of the overall sample (1.55) [Table/Fig-2]. This was statistically significant (p<0.05) as shown in the [Table/Fig-3] by one-way ANOVA.
Analysis of variance (one way ANOVA)comparing the Associated Disability with Plaque Scores, Caries Prevalence, Caries Severity and Decayed (D) component of the caries indices.
| Overall disabilities Vs | Sum of squares | df | Mean square | F | p-value |
|---|
| Plaque score* (baseline) | 30.822 | 7 | 4.403 | 6.208 | 0.001 |
| Caries prevalence | 72.498 | 7 | 10.357 | 0.949 | 0.471 |
| Caries severity* | 1600.670 | 7 | 228.667 | 2.749 | 0.010 |
| Decayed (D) component | 38.926 | 7 | 5.561 | 0.600 | 0.755 |
*indicates significance level (p<0.05)
Mean DMFT/dmft index was 3.2 (SD±3.3) with no significant difference among the overall sample (p>0.05) as shown in [Table/Fig-2,3]. However, the severity of caries as measured with DMFS/dmfs index was higher among the ‘Multiple Disability’ group or the learning disability group when compared to Down syndrome or the hearing impairment with or without speech impairment group. The overall mean DMFS/dmfs of the group was 6.42 (SD±9.45) [Table/Fig-2]. Similarly, the decayed component of the DMFT/dmft index was not significantly related (p>0.05) to any group with the overall mean score of 2.67 (SD±3.01) [Table/Fig-2,3].
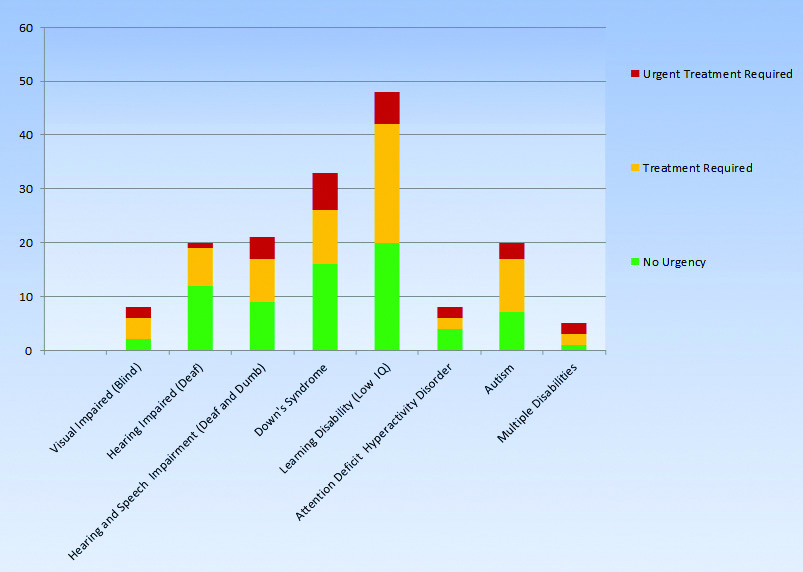
The SCSC were classified on the basis of dental treatment need into three groups as shown in the [Table/Fig-4]. The groups were ‘Urgent Treatment required’ ‘Treatment required’ and ‘No urgency’. This was done after the WHO Oral health survey methods (2013) criteria for treatment urgency [22]. There was a less treatment urgency in physical disabilities when compared to the intellectual disabilities including Down syndrome.
Treatment urgency according to the associated disability among the group of SCSC.
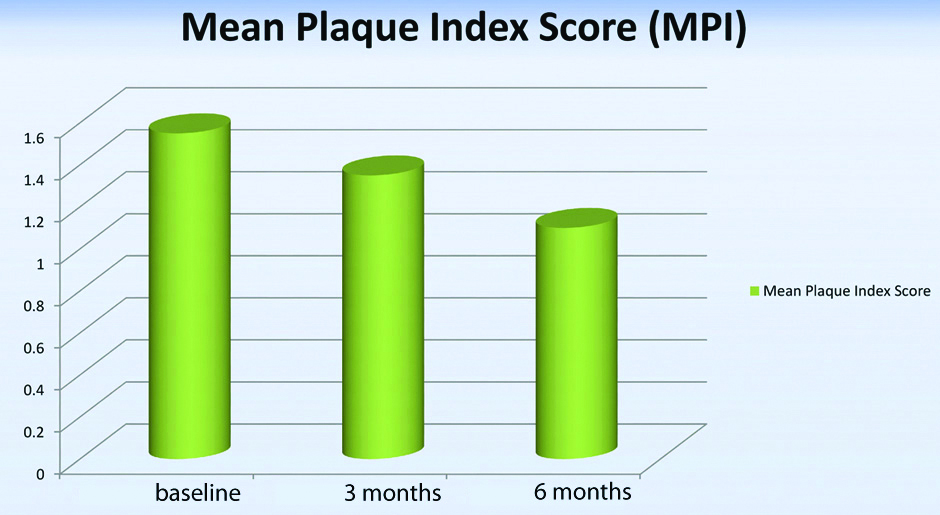
[Table/Fig-5] represents the average plaque scores of the SCSC at baseline, at 3 months and finally at 6 months. There was a gradual but definite decrease in average plaque scores in all groups from an initial average score of 1.55 at baseline to 1.35 after 3 months and finally to 1.1 after 6 months. This was statistically significant (p<0.5). However, there was no significant difference among the various groups of SCSC.
The effect of preventive oral health measures including supervised tooth brushing on mean plaque scores from baseline to three months and finally over the period of six months.
[Table/Fig-6a,b] represent the average cariogram model of the whole SCSC group prior to the campaign involving oral health promotion and finally after the completion at 6 months. The change in circumstances of the group has led to the increase in the green area which represents the chance to avoid new carious lesions from initially 5% to 73%, finally.
The estimated Cariogram representation of the group at the start: (6a) and at the end of six months after incorporation of preventive oral health measures (6b).
Discussion
This study involved the assessment of preventive oral health measures for SCSC boys, over a period of six months. As with this study, other studies have found that the prevalence of oral diseases including dental caries and periodontal conditions are remarkably high in ISHCN, especially in CSHCN [6,7,9,26,27]. SCSC in the present study were at higher risk of developing oral diseases due to various factors based on their medical diagnoses as has been reported by various studies [11,14,28-30].
The mean DMFT score of 3.2 in the study group was less than that reported by some studies in Saudi Arabia [20,31]. However, some studies have also reported lesser mean DMFT score of 2.57 in Gulf countries [32]. Nevertheless, caries is widespread among children in general in Saudi Arabia [33]. Other studies about dental caries with children of similar age group without any disabilities have reported lesser average DMFT of 2 [6,34]. However, the national average DMFT has been reported to be slightly higher at 3.5 [33]. Similarly, for the severity of caries assessed by the DMFS/dmfs index; the findings were lesser than that of a study for a similar population of different age group [20]. However, one study involving children with cerebral palsy of similar age group reported a much higher DMFS average [35]. However, the mean decay component in the study population was 2.67 which is slightly lesser than other study with a similar group of different age in Al-Kharj [20]. The results further indicate a high number of untreated caries in the study population as pointed out by studies in other populations [5,11].
The caries prevalence was not significantly different among various groups and would be comparable to the general population as the risk factors remain the same. In terms of caries severity; which has been assessed by the DMFS/dmfs index, it is a measure of how many tooth surfaces are involved in the carious process. Again, there was a significantly higher mean score for DMFS/dmfs index in the ‘Multiple Disability’ group when compared to Down syndrome group or other physical disability group. It has been known that Down syndrome patients have lesser dental caries as compared to healthy individuals; periodontal problems are of major concern in Down syndrome children [36].
In terms of treatment urgency as is evident from [Table/Fig-4]; the groups with intellectual disability component like Down syndrome need urgent treatment. The urgency of the treatment includes carious teeth forming abscess as well as retained deciduous teeth causing malocclusion and other dental problems. Prevalence of retained teeth in such a group has been reported previously in a similar study [20].
Likewise, higher baseline mean plaque index scores were observed in children with intellectual disability component like the learning disability, Down syndrome and with autism as compared to those with physical disability such as hearing and/or speech impairment. In one study among 14-17-year-old, individuals with physical disability had been shown to have better mean plaque index scores as compared to the ones with intellectual disability [37]. However, children with Autism have been found to maintain better oral hygiene when compared to children with other intellectual disabilities [17]. Yet, in another study comparing Autistic children with their healthy counterpart children in Riyadh city; children with Autism appeared to have higher gingival inflammation and poor oral hygiene with higher mean plaque index score [38]. However, Jain M et al., found that young people with impaired hearing have a high prevalence of dental caries, poor oral hygiene, and extensive unmet needs for dental treatment [39]. Similar findings were reported in Yemen in 6-14-year-old children with disabilities [5]. Although, all groups showed a progressive reduction in mean plaque index scores in the present study, it is assumed that the groups with better intellectual abilities would better sustain such a change and for longer.
In the present study, SCSC were at a higher risk of developing caries according to the cariogram model. This model of assessing the risk for dental caries especially among high risk groups like the SCSC has been used as an educational and motivational tool [40]. It has also been used to assess the effectiveness of preventive oral health measures, especially the change in circumstances that lead to reduced dental caries risk [25]. However, the validity of assessment and prediction using the caries risk assessment has been doubted while suggesting new options for diagnosis and prognosis [41]. In terms of the cariogram model; the medical conditions as well as the circumstances make the group more susceptible for dental caries. Even as it is difficult to control the diet of the group, it is however important to introduce fluoride and effective plaque control for such a group. However, the study group was under an increased risk of getting new carious lesions as they grow older. The estimated cariogram model shows that the chances of avoiding the new carious lesions as shown in the green area of the cariogram increased from 5% to 73%. However, dental caries is a dynamic process with a delicate balance between demineralisation and remineralisation of the tooth structure [42].
Limitation(s)
In spite of the benefits of preventive oral health measures, this programme has difficulties for long term implementation. This programme needs constant motivation and means of encouragement for both parents as well as teachers. This study finding needs longer follow-up and a bigger sample size.
Conclusion(s)
Preventive oral health care programme involving SCSC resulted in significantly lower plaque scores and lesser chance to develop dental caries.
Recommendations: Preventive oral health programmes can be beneficial in prevention of oral diseases and can be developed for SCSC that can be used for similar programmes across Saudi Arabia.
*indicates significance level (p<0.05)
[1]. Crall JJ, Improving oral health for individuals with special health care needsPediatr Dent 2007 29(2):98-104.10.1016/j.cden.2016.02.00427264858 [Google Scholar] [CrossRef] [PubMed]
[2]. Espinoza KM, Heaton LJ, Communicating with patients with special health care needsDent Clin North Am 2016 60(3):693-705. [Google Scholar]
[3]. Bright Futures Steering Committee, & Medical Home Initiatives for Children with Special Needs Project Advisory CommitteeIdentifying infants and young children with developmental disorders in the medical home: An algorithm for developmental surveillance and screeningPediatrics 2006 118(1):405-20.10.1542/peds.2006-123116818591 [Google Scholar] [CrossRef] [PubMed]
[4]. Van Cleave J, Davis MM, Preventive care utilization among children with and without special health care needs: Associations with unmet needAmbul Pediatr 2008 8(5):305-11.10.1016/j.ambp.2008.04.00318922504 [Google Scholar] [CrossRef] [PubMed]
[5]. Al-Maweri S, Zimmer S, Oral health survey of 6-14-year-old children with disabilities attending special schools YemenJ Clin Pediatr Dent 2015 39(3):272-76.10.17796/1053-4628-39.3.27226208074 [Google Scholar] [CrossRef] [PubMed]
[6]. Purohit BM, Acharya S, Bhat M, Oral health status and treatment needs of children attending special schools in South India: A comparative studySpec Care Dentist 2010 30(6):235-41.10.1111/j.1754-4505.2010.00160.x21044103 [Google Scholar] [CrossRef] [PubMed]
[7]. Gardens SJ, Krishna M, Vellappally S, Alzoman H, Halawany HS, Abraham NB, Oral health survey of 6-12-year-old children with disabilities attending special schools in Chennai, IndiaJ Clin Pediatr Dent 2014 24(6):424-33.10.1111/ipd.1208824372860 [Google Scholar] [CrossRef] [PubMed]
[8]. Mitsea A, Karidis A, Donta-Bakoyianni C, Spyropoulos N, Oral health status in Greek children and teenagers, with disabilitiesJ Clin Pediatr Dent 2002 26(1):111-18.10.17796/jcpd.26.1.705x15693372k1g711688807 [Google Scholar] [CrossRef] [PubMed]
[9]. Yashoda R, Puranik MP, Oral health status and parental perception of child oral health related quality-of-life of children with autism in Bangalore, IndiaJ Indian Soc Pedod Prev Dent 2014 32(2):13510.4103/0970-4388.13096724739913 [Google Scholar] [CrossRef] [PubMed]
[10]. Edelstein BL, Chinn CH, Update on disparities in oral health and access to dental care for America’s childrenAcad Pediatr 2009 9(6):415-19.10.1016/j.acap.2009.09.01019945076 [Google Scholar] [CrossRef] [PubMed]
[11]. Nelson LP, Getzin A, Graham D, Zhou J, Wagle EM, McQuiston J, Unmet dental needs and barriers to care for children with significant special health care needsPediatr Dent 2011 33(1):29-36. [Google Scholar]
[12]. Hennequin M, Moysan V, Jourdan D, Dorin M, Nicolas E, Inequalities in oral health for children with disabilities: A French national survey in special schoolsPLoS One 2008 3(6):e256410.1371/journal.pone.000256418575600 [Google Scholar] [CrossRef] [PubMed]
[13]. El-Meligy O, Maashi M, Al-Mushayt A, Al-Nowaiser A, Al-Mubark S, The effect of full-mouth rehabilitation on oral health-related quality of life for children with special health care needsJ Clin Pediatr Dent 2016 40(1):53-61.10.17796/1053-4628-40.1.5326696108 [Google Scholar] [CrossRef] [PubMed]
[14]. Naseem M, Shah AH, Khiyani MF, Khurshid Z, Zafar MS, Gulzar S, Access to oral health care services among adults with learning disabilities: A scoping reviewAnn Stomatol (Roma) 2017 7(3):52-59. [Google Scholar]
[15]. McPherson M, Weissman G, Strickland BB, van Dyck PC, Blumberg SJ, Newacheck PW, Implementing community-based systems of services for children and youths with special health care needs: How well are we doing?Pediatrics 2004 113(Supplement 4):1538-44. [Google Scholar]
[16]. Lee FLM, Yeung AS, Tracey D, Barker K, Inclusion of children with special needs in early childhood education: What teacher characteristics matterTopics in Early Childhood Special Education 2015 35(2):79-88.10.1177/0271121414566014 [Google Scholar] [CrossRef]
[17]. Altun C, Guven G, Akgun OM, Akkurt MD, Basak F, Akbulut E, Oral Health Status of Disabled Individuals Oral Health Status of Disabled Individuals Attending Special SchoolsEur J Dent 2010 4(04):361-66.10.1055/s-0039-169785420922154 [Google Scholar] [CrossRef] [PubMed]
[18]. Cruz S, Chi DL, Huebner CE, Oral health services within community-based organisations for young children with special health care needsSpec Care Dentist 2016 36(5):243-53.10.1111/scd.1217427028954 [Google Scholar] [CrossRef] [PubMed]
[19]. Huebner CE, Chi DL, Masterson E, Milgrom P, Preventive dental health care experiences of preschool-age children with special health care needsSpec Care Dentist 2015 35(2):68-77.10.1111/scd.1208425082666 [Google Scholar] [CrossRef] [PubMed]
[20]. Shah A, Bindayel N, AlOlaywi F, Sheehan S, AlQahtani H, AlShalwi A, Oral health status of a group at a special needs centre in Al-Kharj, Saudi ArabiaJournal of Disability and Oral Health 2015 16(3):79-85. [Google Scholar]
[21]. Curnow MM, Pine CM, Burnside G, Nicholson JA, Chesters RK, Huntington E, A randomised controlled trial of the efficacy of supervised toothbrushing in high-caries-risk childrenCaries Res 2002 36(4):294-300.10.1159/00006392512218280 [Google Scholar] [CrossRef] [PubMed]
[22]. World Health Organisation. Oral health surveys: basic methods: World Health Organisation; 2013 [Google Scholar]
[23]. Fischman SL, Current status of indices of plaqueJ Clin Periodontol 1986 13(5):371-74.10.1111/j.1600-051X.1986.tb01475.x3013947 [Google Scholar] [CrossRef] [PubMed]
[24]. Daryani H, Nagarajappa R, Sharda AJ, Asawa K, Tak M, Sanadhya S, Cariogram model in assessment of dental caries among mentally challenged and visually impaired individuals of Udaipur, IndiaJ Clin Diagn Res 2014 8(1):206-10. [Google Scholar]
[25]. Patil Y, Hegde-Shetiya S, Kakodkar P, Shirahatti R, Evaluation of a preventive program based on caries risk among mentally challenged using the Cariogram modelCommunity Dent Health 2011 20:1-6. [Google Scholar]
[26]. Gaçe E, Kelmendi M, Fusha E, Oral health status of children with disability living in AlbaniaMateria Socio-Medica 2014 26(6):39210.5455/msm.2014.26.392-39425685085 [Google Scholar] [CrossRef] [PubMed]
[27]. Rao D, Amitha H, Munshi AK, Oral hygiene status of disabled children and adolescents attending special schools of South Canara, IndiaHong Kong Dent J 2005 2(2):107-13. [Google Scholar]
[28]. Jain M, Mathur A, Sawla L, Choudhary G, Kabra K, Duraiswamy P, Oral health status of mentally disabled subjects in IndiaJournal of Oral Science 2009 51(3):333-40.10.2334/josnusd.51.33319776499 [Google Scholar] [CrossRef] [PubMed]
[29]. De Jongh A, Van Houtem C, Van Der Schoof M, Resida G, Broers D, Oral health status, treatment needs, and obstacles to dental care among noninstitutionalized children with severe mental disabilities in The NetherlandsSpec Care Dentist 2008 28(3):111-15.10.1111/j.1754-4505.2008.00022.x18489659 [Google Scholar] [CrossRef] [PubMed]
[30]. Shivakumar K, Patil S, Kadashetti V, Raje V, Oral health status and dental treatment needs of 5-12-year-old children with disabilities attending special schools in Western Maharashtra, IndiaInt J Appl Basic Med Res 2018 8(1):2410.4103/ijabmr.IJABMR_57_1729552531 [Google Scholar] [CrossRef] [PubMed]
[31]. Khan SQ, Khan NB, ArRejaie AS, Dental cariesSaudi Med J 2013 34(7):744-49. [Google Scholar]
[32]. Alayyan W, Al Halabi M, Hussein I, Khamis A, Kowash M, A Systematic Review and Meta-analysis of School Children’s Caries Studies in Gulf Cooperation Council StatesJ Int Soc Prev Community Dent 2017 7(5):234-41. [Google Scholar]
[33]. Al Agili DE, A systematic review of population-based dental caries studies among children in Saudi ArabiaSaudi Dent J 2013 25(1):03-11.10.1016/j.sdentj.2012.10.00223960549 [Google Scholar] [CrossRef] [PubMed]
[34]. Al-Banyan R, Echeverri E, Narendran S, Keene H, Oral health survey of 5-12-year-old children of National Guard employees in Riyadh, Saudi ArabiaInt J Paediatr Dent 2000 10(1):39-45.10.1046/j.1365-263x.2000.00166.x11310125 [Google Scholar] [CrossRef] [PubMed]
[35]. Alhammad NS, Wyne AH, Caries experience and oral hygiene status of cerebral palsy children in RiyadhOdontostomatol Trop 2010 33(130):5-9. [Google Scholar]
[36]. Deps TD, Angelo GL, Martins CC, Paiva SM, Pordeus IA, Borges-Oliveira AC, Association between Dental Caries and Down Syndrome: A Systematic Review and Meta-AnalysisPLoS One 2015 10(6):e012748410.1371/journal.pone.012748426086498 [Google Scholar] [CrossRef] [PubMed]
[37]. Ameer N, Palaparthi R, Neerudu M, Palakuru SK, Singam HR, Durvasula S, Oral hygiene and periodontal status of teenagers with special needs in the district of Nalgonda, IndiaJ Indian Soc Periodontol 2012 16(3):421-25.10.4103/0972-124X.10092323162340 [Google Scholar] [CrossRef] [PubMed]
[38]. Diab HM, Motlaq SS, Alsharare A, Alshammery A, Alshammery N, Khawja SG, Comparison of gingival health and salivary parameters among autistic and non-autistic school children in RiyadhJ Clin Diagn Res 2016 10(10):ZC11010.7860/JCDR/2016/23373.869227891471 [Google Scholar] [CrossRef] [PubMed]
[39]. Jain M, Mathur A, Kumar S, Dagli RJ, Duraiswamy P, Kulkarni S, Dentition status and treatment needs among children with impaired hearing attending a special school for the deaf and mute in Udaipur, IndiaJ Oral Sci 2008 50(2):161-65.10.2334/josnusd.50.16118587205 [Google Scholar] [CrossRef] [PubMed]
[40]. Bratthall D, Hänsel Petersson G, Cariogram-A multifactorial risk assessment model for a multifactorial diseaseCommunity Dent Oral Epidemiol 2005 33(4):256-64.10.1111/j.1600-0528.2005.00233.x16008632 [Google Scholar] [CrossRef] [PubMed]
[41]. Cagetti MG, Bontà G, Cocco F, Lingstrom P, Strohmenger L, Campus G, Are standardized caries risk assessment models effective in assessing actual caries status and future caries increment? A systematic reviewBMC Oral Health 2018 18(1):12310.1186/s12903-018-0585-430012136 [Google Scholar] [CrossRef] [PubMed]
[42]. González-Cabezas C, The chemistry of caries: Remineralisation and demineralisation events with direct clinical relevanceDent Clin North Am 2010 54(3):469-78.10.1016/j.cden.2010.03.00420630190 [Google Scholar] [CrossRef] [PubMed]