A Case of Unilateral Hyperlucency on Chest X-Ray- A Diagnostic Dilemma
Nafees Ahmad Khan1, Mohammad Arif2, Rakesh Bhargava3, Mohammad Shameem4, Sadaf Sultana5
1 Assistant Professor, Department of Pulmonary Medicine, Jawaharlal Nehru Medical College and Hospital, AMU, Aligarh, Uttar Pradesh, India.
2 Senior Resident, Department of Pulmonary Medicine, Jawaharlal Nehru Medical College and Hospital, AMU, Aligarh, Uttar Pradesh, India.
3 Professor, Department of Pulmonary Medicine, Jawaharlal Nehru Medical College and Hospital, AMU, Aligarh, Uttar Pradesh, India.
4 Professor, Department of Pulmonary Medicine, Jawaharlal Nehru Medical College and Hospital, AMU, Aligarh, Uttar Pradesh, India.
5 Junior Resident, Department of Radiodiagnosis, Jawaharlal Nehru Medical College and Hospital, AMU, Aligarh, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Mohammad Arif, Flat No. 305, IT Grand Apartment, Medical Road, Zakariya Market, Aligarh, Uttar Pradesh, India.
E-mail: arif2k10@gmail.com
Unilateral hyperlucency of the lung is not an uncommon finding which arises from a variety of conditions, like technical, congenital and acquired. Here, the author presents a case of diaphragmatic hernia which presented as unilateral hyperlucency on chest radiography. A 45-year-old female, presented with complaint of shortness of breath for 2-3 years, increased since 15 days and pain in abdomen for 2-3 years. She consulted a doctor where a chest X-ray was done and was advised Intercostal tube insertion with the diagnosis of left-sided pneumothorax and was referred to us for further management. Instead of her vitals were stable on examination. On auscultation, breath sounds were of decreased intensity. A chest X-ray was then done which showed unilateral hyperlucency of the left side with the presence of air fluid level. The CECT thorax showed a large diaphragmatic hernia through which the large intestine and stomach were occupying the left hemithorax. Therefore, a thorough evaluation should be done before reaching a definitive diagnosis in such patients.
Diaphragmatic hernia, Hyperlucent chest X-ray, Pneumothorax
Case Report
A 45-year-old female, housewife, without any known co-morbidity, reported with the complaints of breathlessness for the last 2-3 years which has increased in the last 15 days. It was mild in intensity, New York Heart Association (NYHA) grade 2, not associated with diaphoresis, chest pain, cough, haemoptysis and fever. There was no postural variation. The patient was also complaining of pain in abdomen since 2-3 years, on and off which was mild in intensity, dull aching in character, non-radiating and had no association with the timing of meals. No other associated gastrointestinal complaints were there. There was no history of thoracic or abdominal trauma of any kind.
For these complaints, the patient visited a local physician two years back where she was advised Anti Tubercular Treatment (ATT) based on her chest X-ray findings which was followed for nine months, but even after completing the course around six months back, there was no relief in symptoms. The patient then complained of increasing breathlessness for the past 15 days and visited some physician, where chest X-ray was done and was advised ICTD Insertion with a diagnosis of left-sided pneumothorax and was referred to us for further management. On examination, her vitals were stable except for mild tachypnea (RR-25/minute). There were no significant findings on the general examination.
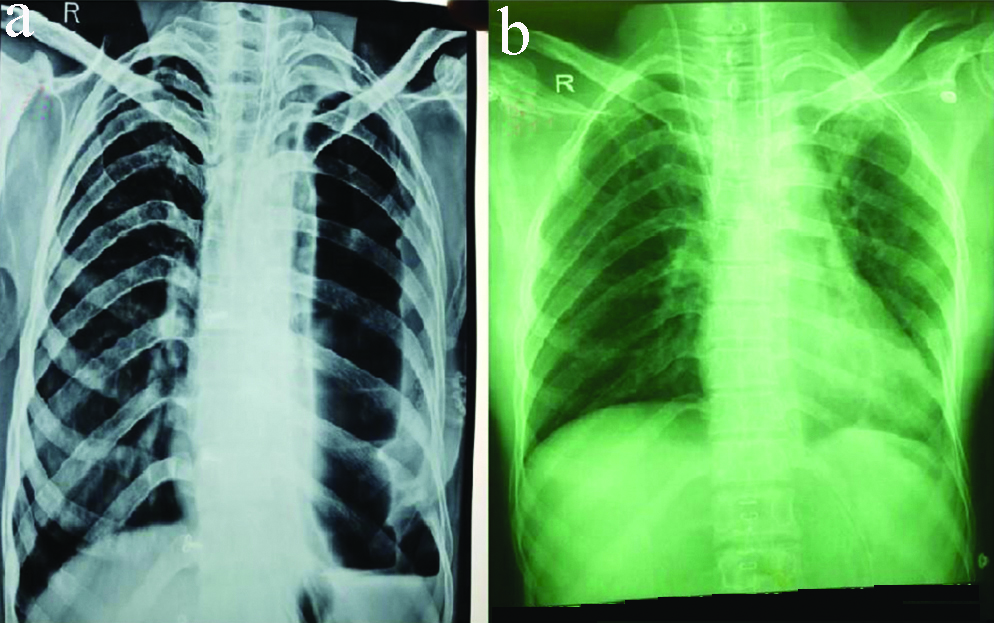
On examining her respiratory system, it was found that there was decreased movement on respiration on the left side compared to the right, vocal fremitus decreased on the left side, tympanic note heard on percussion on the left side in all areas, breath sounds were of decreased intensity on the left side compared to right with no added sounds. The examination of other systems was normal. Routine laboratory investigations were also normal. The instead of her chest X-ray showed right anterior rotation with increased hyperlucency covering almost the whole of the left hemithorax with air fluid level with the mediastinum slightly shifted towards the right side [Table/Fig-1].
Chest X-ray of the patient at presentation showing hyperlucent left hemithorax with air fluid level.

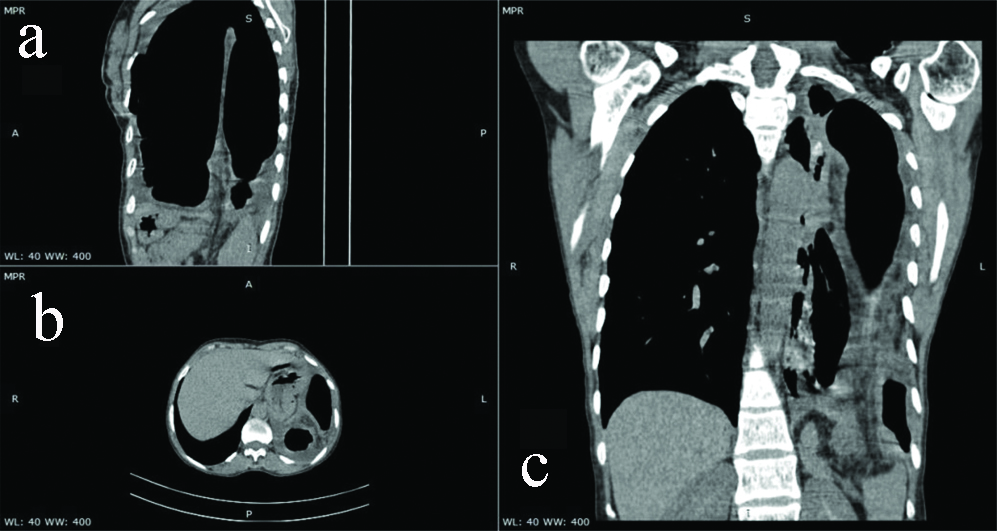
Based on the history, examination and chest X-ray, the differential diagnosis was left-sided hydro-pneumothorax due to chronic and left-sided big cavity with fluid level. But since there was a disparity between clinical findings and chest X-ray and the patient did not require any urgent interventions as was stable, an HRCT thorax with abdominal cuts was advised. On HRCT, there was a large posterolateral defect of 12×14 cm in the left diaphragm through which stomach and loops of the large intestine were herniating into the left hemithorax [Table/Fig-2], thus a diagnosis of left Bochdalek diaphragmatic hernia was made. The patient was then referred to the surgical unit for further management.
HRCT thorax showing a large defect in the left hemithorax of approximately 12×14 cm through which the stomach and large bowel loops are herniating and reaching upto the apex seen in para sagittal (a), axial (b) and coronal view (c).
Laparotomy was done, which confirmed the presence of a large defect of approximately 12×14 cm in the left diaphragm. The stomach and colon were reduced in the peritoneal cavity. There was no associated necrosis or strangulation of herniated bowel contents. The primary defect was closed with interrupted, non-absorbable suture. A post surgery chest X-ray in which the normal, fully expanded left lung parenchyma can be appreciated is shown in [Table/Fig-3]. Follow-up of the patient was uneventful and she was discharged one week after the procedure.
At the time of presentation (pre) (a) and post (b) surgery chest X-ray of the patient showing normal, fully expanded, left lung parenchyma compared to the hyperlucent left lung field.
Discussion
Unilateral hyperlucency of the lung is not an uncommon finding which arises from a variety of conditions, both congenital and acquired. The causes are multiple and can involve various structures like chest wall, blood vessels, pleura, etc. The various causes have been summarised in [Table/Fig-4] [1]. Technical factors, like right or left anterior rotation, which is unrelated to lung disease, can cause false-positive results and therefore, must also be considered.
Various causes of Unilateral hyperlucency of the lungs.
| Site of Pathology | Causes |
|---|
| Chest wall | Scoliosis, Poland syndrome, Mastectomy |
| Blood vessels | Pulmonary embolism, Pulmonary agenesis, Pulmonary hypoplasia, Scimitar syndrome |
| Lung parenchyma | Atelectasis, Emphysema, Pneumonectomy, Swyer-James syndrome |
| Airway | Foreign body aspiration, Bronchial atresia, Endobronchial mass, External bronchial compression, Congenital lobar emphysema |
| Mediastinal and pleural space | Benign mediastinal masses, Mediastinal lymphadenopathy, Pneumothorax, Pleural effusion, Diaphragmatic hernia |
| External/technical factors | Rotation |
Diaphragmatic hernias can be both congenital and acquired, with congenital being more common than acquired. Four different types of congenital Diaphragmatic hernia have been described in the literature. They include: posterolateral hernia of Bochdalek, which is the most common type, parasternal hernia of Morgagni-Larrey, eventration of the diaphragm and peritoneal-pericardial hernia [2]. Adult-onset diaphragmatic hernia is rare and mainly acquired in nature secondary to blunt trauma to the thorax or abdomen [3]. Congenital diaphragmatic hernia is usually diagnosed prenatally or during the early postnatal period. But in around 5-25% of the cases, they are diagnosed in adulthood either during a routine examination or because of various gastrointestinal and respiratory complaints [4]. Bochdalek hernias, which results due to failure of closure of the pleuroperitoneal canal during development, primarily manifests in children. Adult-onset Bochdalek hernia is extremely rare and it constitutes just 0.17%-6% of all diaphragmatic hernias reported in adults [5]. Various case reports from India of patients presenting with adults onset congenital diaphragmatic hernia is summarised in [Table/Fig-5] [6-10]. The clinical presentation in adults and the paediatric age group is also different. In neonates and infants, it usually presents with respiratory distress and cyanosis while in adults, it often presents with chest pain, difficulty in breathing, abdominal pain and even features of intestinal obstruction [5]. It is believed that the delay or absence of symptoms may result from the closure of the diaphragmatic defect by the intra-abdominal viscus [11]. A chest X-ray is usually the first investigation done in these patients which in typical cases, shows abdominal organs in the thoracic cavity with haustrations and air fluid levels [11]. But misdiagnosis, especially in adult patients is very common. they are commonly misdiagnosed as pleural effusion, empyema, lung cyst and pneumothorax when a Computed Tomography (CT) scan is not done [2]. It is extremely rare for the intestines to reach almost to the apex of the lung without any visible haustrations and occupying almost whole of the hemithorax as was the case with our patient. Therefore, many a time, these patients are mismanaged with chest tube insertion based on misdiagnosis and correct diagnosis and management is significantly delayed. CT scan is the imaging modality of choice for the diagnosis and evaluation of diaphragmatic hernia. On CT scan, they can be diagnosed by the discontinuity of diaphragm or non recognition of a part of the diaphragm, or by intrathoracic herniation of abdominal contents. Various signs, like “Dangling diaphragm” sign, “Dependent viscera” sign and “Collar sign” have also been described [12]. In this case, the discontinuity of diaphragm and dependent viscera sign was present.
Similar reported cases of congenital non-traumatic diaphragmatic hernia presenting in adults from India [6-10].
| S. No. | Author | Year | Age/Gender | Complaints | Side involved | Surgical approch | Hernia orifice | Closure |
|---|
| 1. | Gujar A et al., [6] | 2013 | 27 years/female | Pain abdomen and breathlessness | Right | Laparotomy | 8×8 cm | Suture |
| 2. | Singh TC et al., [7] | 2015 | 43 years/male | Pain abdomen, vomiting and acute onset respiratory distress | Left | Thoraco-abdominal | 5×8 cm | Mesh |
| 3. | Luther A and Mahajan A [8] | 2015 | 25 years/female | Peri umbilical pain, left lower chest discomfort and breathlessnes | Left | Laprotomy | 6×8 cm | Suture |
| 4. | Pillai SA and Chinnappan S [9] | 2016 | 42 years/female | Epigastric pain and breathlessness on exertion | Right | Laparotomy | 6×4cm | Suture |
| 5. | Agrawal MM et al., [10] | 2018 | 41 years/female | Pain abdomen | Left | Laproscopy | 10×8 cm | Suture |
| 6 | Present case | 2020 | 45 years/female | Shortness of breath and pain abdomen | Left | Laprotomy | 12×14 cm | Suture |
Bochdalek hernia is always managed by surgical repair even in asymptomatic individuals because of the risk of intestinal obstruction and strangulation [2]. The basic principle of management is the repair of the diaphragmatic defect following the reduction of the herniated contents in the peritoneal cavity. Different approaches have been described like laparotomy, laparoscopy, or thoraco-abdominal, each having their own set of advantages and disadvantages. The defect in the diaphragm is managed by suture closure, prosthetic mesh implantation, or by using muscle flap [13].
Conclusion(s)
Congenital diaphragmatic hernia can rarely present in adults mimicking pneumothorax or hydropneumothorax. Therefore, a thorough clinical history and examination should be undertaken before proceeding with definitive treatment to avoid wrong diagnosis and corresponding mismanagement of the patient.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Apr 20, 2020
Manual Googling: Jul 04, 2020
iThenticate Software: Jul 28, 2020 (15%)
[1]. Vancamp T, Van Cauwenberghe T, Bellinck P, Mulkens T, Salgado R, Termote JL, How to approach unilateral hyperlucency of the lung?European Society of Radiology 2013 :01-17.Available at: http://pdf.posterng.netkey.at/download/index.php?module=get_pdf_by_id&poster_id=117660 [Google Scholar]
[2]. Navakishore K, Sharma D, Gondu GR, Thumma VM, Gunturi SV, Reddy JM, Surgical management of adult diaphragmatic hernia- An instituitional experienceIJCMSR [Internet] 2018 3(2):B54-57.Available from: https://www.ijcmsr.com/uploads/1/0/2/7/102704056/ijcmsr__3_2__81_v2.pdf10.21276/ijcmsr.2018.3.2.13 [Google Scholar] [CrossRef]
[3]. Yang GPC, Tang CN, Siu WT, Ha JPY, Tai YP, Li MK, Diaphragmatic hernia: An uncommon cause of dyspepsiaJSLS 2005 9(3):352-55. [Google Scholar]
[4]. Yagmur Y, Yiğit E, Babur M, Gumuş S, Bochdalek hernia: A rare case report of adult ageAnn Med Surg (Lond) 2016 5:72-75.10.1016/j.amsu.2015.11.01226865978 [Google Scholar] [CrossRef] [PubMed]
[5]. Alam A, Chander B, Adult bochdalek herniaMed J Armed Forces India 2005 61(3):284-86.10.1016/S0377-1237(05)80177-7 [Google Scholar] [CrossRef]
[6]. Gujar A, Rodrigues DD, Patil K, Tambe U, Sinha S, Bhushan A, Rare case report-Congenital diaphragmatic hernia presentation in adultIndian Journal of Surgery 2013 75(1):44-46.10.1007/s12262-011-0321-724426509 [Google Scholar] [CrossRef] [PubMed]
[7]. Singh TC, Singh CG, Lamare KN, Babitha N, Kharnaior A, Congenital diaphragmatic hernia in adult presenting with obstruction: A rare caseInt J Sci Stud 2015 2(10):142-45. [Google Scholar]
[8]. Luther A, Mahajan A, Left-sided bochdalek hernia in an adult: A case report with review of literatureJournal of International Medical Sciences Academy 2015 28(1):33-34. [Google Scholar]
[9]. Pillai SA, Chinnappan S, Congenital right Morgagni hernia presenting in an adult-A case reportIndian Journal of Surgery 2016 78(3):238-40.10.1007/s12262-015-1400-y27358522 [Google Scholar] [CrossRef] [PubMed]
[10]. Agrawal MM, Bhagwat S, Sali P, Rao P, (2018) Laparoscopic repair of diaphragmatic hernia in the adult: A case report & review of literatureJ Surg: JSUR-113310.29011/2575-9760 [Google Scholar] [CrossRef]
[11]. Vega MT, Maldonado RH, Vega GT, Vega AT, Liévano EA, Velázquez PM, Late-onset congenital diaphragmatic hernia: A case reportInternational Journal of Surgery Case Reports 2013 4(11):952-54.10.1016/j.ijscr.2013.07.03424055915 [Google Scholar] [CrossRef] [PubMed]
[12]. Ladumo S, Case report: Non-traumatic diaphragmatic hernia in adultOAJS [Internet] 2017 Oct 2 [cited 2019 Nov 25] 6(2)Available from: https://juniperpublishers.com/oajs/OAJS.MS.ID.555682.php10.19080/OAJS.2017.06.555682 [Google Scholar] [CrossRef]
[13]. Moro K, Kawahara M, Muneoka Y, Sato Y, Kitami C, Makino S, Right-sided Bochdalek hernia in an elderly adult: A case report with a review of surgical managementSurg Case Rep [Internet] 2017 [cited 2020 Jun 18] 3Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5640563/10.1186/s40792-017-0385-029030793 [Google Scholar] [CrossRef] [PubMed]