Introduction
Chronic Kidney Disease (CKD) has been recognised as a worldwide health threat and understanding its complex patho-physiological mechanisms could go a long way in taking care of patients with CKD. One of the most important causes for mortality in End Stage Renal Disease (ESRD) patients is Cardiovascular Disease (CVD). ESRD is a low grade chronic inflammatory state, suspected to promote atherosclerosis.
Aim
To determine, if there is any association between elevated High-sensitivity C-Reactive Protein (hs-CRP) and development of future cardiovascular events in stage-5 CKD patients.
Materials and Methods
Forty-five CKD stage-5 patients were included in the study, after ruling out patients with established CVD. According to categorisation proposed by the American Heart Association for the cut-off value of hs-CRP-value (3 mg/L), patients were divided into two groups. Those who had hs-CRP more than 3 mg/L were considered to have ‘elevated hs-CRP’ and those who had a value 3 mg/L and below were considered to have ‘normal hs-CRP’ levels. These patients were followed-up monthly, for a period of one year to record any occurrence of cardiovascular events (coronary events/cerebrovascular accidents/peripheral occlusive vascular disease). Statistical Package for the Social Sciences (SPSS) 16.0 was used for analysis. Chi-square test and Mann-Whitney U-test were used for statistical comparison between the groups and a p-value of 0.05 or less was considered to be statistically significant. Receiver Operating Characteristic (ROC) curve was also plotted to determine the cut-off value for hs-CRP based on the occurrence of any cardiovascular event.
Results
Baseline hs-CRP level was more than 3 mg/L in 42% of patients. Among those who had elevated hs-CRP, 78.9% of patients developed cardiovascular events during the follow-up period. This signifies a strong association between elevated hs-CRP and CVD in ESRD patients. The hs-CRP cut-off point of 3 mg/L was obtained from ROC curve.
Conclusion
There was a significant association between elevated hs-CRP and development of cardiovascular events in ESRD patients. Hence, hs-CRP can be used as a marker of future cardiovascular events in CKD stage-5 patients.
Atherosclerosis, End stage renal disease, Inflammatory marker, Renal failure
Introduction
CKD is considered as a global health threat and understanding the complex mechanisms underlying would help in improving the quality of life in these patients [1,2]. Even with the latest interventions in dialysis technology, the morbidity as well as mortality in these patients continues to remain very high [3]. CVD is an important cause of mortality in CKD stage-5 patients [4]. In addition to the conventional risk factors like diabetes, hypertension and dyslipidemia [5] other factors associated with uremic milieu also play an important role in the development of CVD [6]. These days, chronic inflammation is often thought to be a “secret killer” which may promote atherosclerosis [7,8].
The association between inflammation and CVD is best described in ESRD patients [9]. The haemodialysis (HD) procedure itself contributes to the inflammatory state, which in turn leads to the formation of Acute Phase Response (APR) proteins and pro-inflammatory cytokines [10] like interleukin (IL)-1, oxidised Low-Density Lipoproteins (LDL), Tumour Necrosis Factor-α (TNF-α), intercellular adhesion molecule-1 and selectins [11]. Most of these biomarkers including C-Reactive Protein (CRP), IL-6, or White Blood Cell (WBC) count are key predictors of the outcome in patients with ESRD [12].
Of the multitude of circulatory markers, CRP is the best studied marker [13]. CRP is an acute phase protein which is synthesised by hepatocytes in response to pro-inflammatory cytokines, particularly IL-6 [14]. Now, it has been proven that this hepatic-derived protein is not only a marker, but also a mediator of vascular disease [15]. CRP has a definite role in complement pathway activation, uptake of lipids by macrophages, cytokine release, expression of tissue factor in monocytes, endothelial dysfunction and inhibition of nitric oxide production [14]. Accumulating data from prospective cohort studies in CKD patients have proved an association between CRP levels and cardiovascular mortality [16,17]. Even though the association between vascular disease and CRP has been accepted for several decades [18], the concept of micro-inflammation is relatively new. Chronic renal disease being a chronic low grade inflammatory condition, warrants a highly sensitive technique for the detection of low levels of CRP and hence hs-CRP is considered here [16,19]. The use of CRP for assessing micro-inflammation requires hs-CRP assays with detection limits less than 0.3 mg/L [20]. hs-CRP can accurately measure even minimal levels of CRP in the cardiovascular risk assessment range (0.20-10.0 mg/L) [21]. Hence, it is reasonable to limit current assays of inflammatory markers to hs-CRP as it’s assays are comparatively cheaper and easily available [22]. The close association between hs-CRP and cardiovascular risk has been established in many studies [23]. But there is paucity of literature determining the association between elevated hs-CRP and development of future cardiovascular events in CKD stage- 5 patients in India, hence this study was undertaken to determine if there is any association between elevated hs-CRP and development of future cardiovascular events in CKD patients.
Materials and Methods
This was a prospective observational study done in Nephrology Department of Government Medical College, Kottayam, Kerala, India, from 1st January 2013 to 31st December 2013. The study was initiated after obtaining approval of the Institutional Review Board (IEC clearance certificate number: 127/2012). All the patients who matched the inclusion criteria and who gave consent were recruited for the study until the required sample size of 45 was obtained.
Sample size calculation: Sample size=Z2×pq/d2, Value of Z for alpha at 5% level of significance=1.96, p (average prevalence of cardiovascular events in CKD stage V patients) =70%, q=100-p=30%, d (absolute precision) =20% of p. The calculated sample size=41, so, rounded-off to 45.
Inclusion criteria: CKD Stage-5 patients (Glomerular Filtration Rate (GFR) <15 mL/min/1.73 m2) who were clinically stable (vitals normal) were included in the study. GFR was calculated as Ccr (clearance of creatinine) by the Cockroft-Gault (CG) equation: Creatinine clearance (mL/min) ={(140-Age) × (weight) × (0.85 if female)}/{(72) × (serum creatinine)} [24].
Exclusion criteria: Those patients showing evidence of infection (such as fever, raised total and differential WBC count and positive blood culture and those with established CVD (previous history of coronary artery disease, stroke, peripheral artery disease, thromboembolic diseases) were excluded from the study.
After obtaining written informed consent from the patients, baseline details such as age and gender were collected. Blood samples were collected from the venous end of an Arteriovenous (AV) fistula at the beginning of the haemodialysis session, centrifuged within two hours and the serum was transferred to micro-centrifuge tubes and analysed for hs-CRP using particle enhanced immuno-turbidimetric assay [25]. A second blood sample was drawn two weeks later (from each patient) and repeat hs-CRP estimation was done. The average of these two results of hs-CRP estimation was considered for analysis in the study. The patients were categorised into two groups based on their average hs-CRP-values >3 mg/L (elevated hs-CRP) and <3 mg/L (normal hs-CRP) according to categorisation proposed by the American Heart Association [26]. Both these groups were followed-up for a period of one year for the occurrence of cardiovascular events (coronary events/cerebrovascular accidents/peripheral occlusive vascular disease). Follow-up of cardiovascular events was done monthly by personnel interview in Nephrology Ward or telephonically interviewed. At the end of one year, the patient’s medical records were thoroughly searched for the occurrence of cardiovascular events.
Statistical Analysis
Statistical analysis was performed using SPSS 16.0. The hs-CRP-values were analysed and compared between the groups (normal hs-CRP and elevated hs-CRP) using Chi-square test and Mann-Whitney U-test. Significance was assessed at 5% level and a p-value of 0.05 or less was considered to be statistically significant test result. ROC curve was plotted based on hs-CRP values and occurrence of adverse cardiovascular event, and 3mg/L was obtained as the cut-off value that is predictive of increased risk of adverse cardiovascular event.
Results
Most of the study participants belonged to the age group of >40 years (69%) and majority were males (64%) [Table/Fig-1]. Of the 45 participants, 17 (37.8%) developed cardiovascular events and 28 (62.2%) did not and those who succumbed to death comprised of 49% (22 people) [Table/Fig-2]. According to categorisation proposed by the American Heart Association for the cut-off value of hs-CRP-value (3mg/L), patients were divided into two groups: hs-CRP ≤3 mg/L (n=26) i.e., 57.7% and hs-CRP >3 mg/L (n=19) i.e., 42.2%. Chi-square test was done to detect the difference in proportions between those with high and normal hs-CRP-values associated cardiovascular event (p-value <0.001**) and mortality (p-value=0.026*). Since p-value was found to be <0.05, there was significant association between hs-CRP and occurence of cardiovascular event and mortality [Table/Fig-3].
Age gender distribution of study subjects.
| Variables | n (%) |
|---|
| Age distribution (in years) |
| 10-40 | 14 (31%) |
| >40 | 31 (69%) |
| Gender |
| Males | 29 (64%) |
| Females | 16 (36%) |
Distribution of participants based on occurence of adverse cardiovascular event and mortality.
| Cardiovascular event |
|---|
| Event occurred | 17 (37.8%) |
| No event | 28 (62.2%) |
| Mortality |
| Expired | 22 (49%) |
| Alive | 23 (51%) |
Association of cardiovascular events and mortality based on hs-CRP-values.
| Factors | hs-CRP ≤3 mg/L (n=26) | hs-CRP >3 mg/L (n=19) | Chi-square | p-value |
|---|
| Cardiovascular events |
| Event occurred | 2 (7.7%) | 15 (78.9%) | 23.7 | <0.001** |
| No event | 24 (92.3%) | 4 (21.1%) |
| Mortality |
| Expired | 9 (34.6%) | 13 (68.4%) | 5.021 | 0.026* |
| Alive | 17 (65.4%) | 6 (31.6%) |
*p<0.05-statistically significant **p<0.001 statistically highly significant; hs-CRP: High-sensitivity C-Reactive Protein
Mann-Whitney U test was also done to test the difference in hs-CRP among those with occurrence of cardiovascular event and those without. Similarly, hs-CRP level was compared with those with mortality and without. The mean rank was higher for those who developed cardiovascular event compared to the other group with Mann-Whitney U value=33.5 and p-value <0.001, implying a significant difference in hs-CRP levels between the two groups. Similarly, mean rank was higher for those who have expired compared to those who were alive with a Mann-Whitney U value=131.5 and p-value <0.001, implying a significantly higher hs-CRP-value among those who expired [Table/Fig-4].
Comparison of hs-CRP-values.
| Variables | Mean rank | Mann-Whitney U test value | p-value |
|---|
| Cardiovascular events |
| Event occurred | 35.03 | 33.5 | <0.001** |
| No event | 15.70 |
| Mortality |
| Expired | 28.52 | 131.5 | <0.001** |
| Alive | 17.72 |
**p<0.001 statistically highly significant
Receiver Operating Characteristic (ROC) curve
ROC plot was used for assessing the accuracy of prediction of cardiovascular event based on hs-CRP values. The area under ROC curve was 0.930, which was found to be statistically significant (p-value=0.001). The hs-CRP cut-off value where the sensitivity and specificity were highest was 3 mg/L [Table/Fig-5].
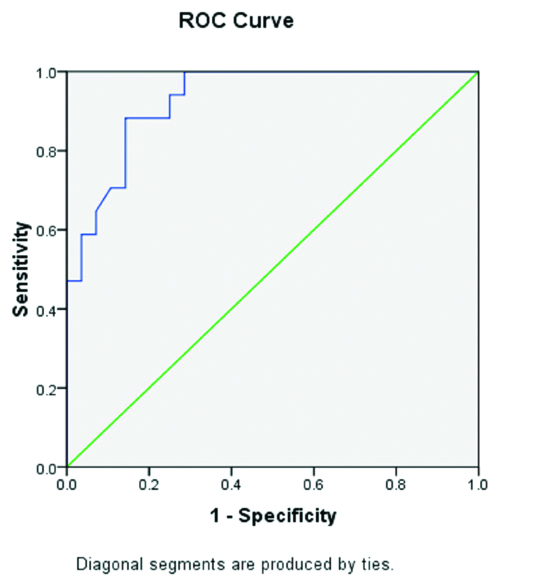 |
|---|
| Area | Std. error | Asymptotic Sig. | Asymptotic 95% Confidence interval |
|---|
| Lower bound | Upper bound |
|---|
| 0.930 | 0.035 | 0.001* | 0.860 | 0.999 |
*p<0.05-statistically significant
Discussion
The present study was done to determine if there was any association between elevated hs-CRP and future cardiovascular events in CKD stage-5 patients. Majority of the patients were males in the age group >40 years. According to categorisation proposed by the American Heart Association for the cut-off value of hs-CRP-value (3 mg/L), patients were divided into two groups: elevated hs-CRP and normal hs-CRP.
More than two-thirds of the patients who developed cardiovascular events during the follow-up period had an elevated hs-CRP (>3 mg/L). This was significantly significant as compared to those without any occurrence of cardiovascular event (p-value <0.001). This signifies a strong association between inflammation and CVD in CKD. This was in accordance with the study done by Jalal D et al., which showed an increased risk of cardiovascular events after four years of follow-up in CKD patients with increased hs-CRP [27]. Another study done by Lestariningsih L et al., also supported present study findings, in which hs-CRP was found to be a significant predictive of Intima-Media Thickness (IMT) progression in haemodialysis subjects [28]. Also, recently, Kalkman DN et al., estimated, in a retrospective registry study of 7026 patients undergoing Percutaneous Coronary Intervention (PCI) that although, 38% had persistently hs-CRP ≥2 mg/L, 10% more increased their hs-CRP over a four week period [29]. Inflammation can promote vascular injury via different mechanisms- changes in structure and function of lipoproteins, alteration in the composition of plasma proteins, vascular endothelial changes and alterations in the expression of specific ligands on the surfaces of platelets, neutrophils and mononuclear cells [30,31]. The distribution of mortality was also studied according to the hs-CRP levels and a significant association was observed between hs-CRP and mortality (p-value: 0.026). This suggests that individuals with CKD are more likely to die of CVD. This was in accordance with the study done by Khunte SK et al., which showed that cardiovascular mortality was the major cause of death among CKD patients [32].
From ROC curve, hs-CRP-value- 3 mg/L was obtained as the cut-off value that is predictive of increased risk of adverse cardiovascular event. Various studies have shown different cut-off points of CRP that were predictive of cardiovascular mortality. The cut-off points used by Chauveau P et al., Tellingen A et al., and Iseki K et al., were 5 mg/L, 8 mg/L and 10 mg/L, respectively [33-35]. Elevated risk of overall and cardiovascular mortality was observed in patients with elevated CRP-values in all of these studies.
Limitation(s)
The follow-up period of the present study was limited to one year and also the details of cardiac event was not enquired into.
Conclusion(s)
This study shows that low-grade inflammation, as measured by a hs-CRP can predict future cardiovascular events and mortality in CKD stage-5 patients in India. hs-CRP-value- 3 mg/L can be used as a cut-off for categorisation of patients and predicting adverse outcomes. Since strong association between accelerated atherogenesis and hs-CRP was appreciated from present study, early effective preventive measures could be adopted to prevent future adverse cardiac events in CKD patients.
*p<0.05-statistically significant **p<0.001 statistically highly significant; hs-CRP: High-sensitivity C-Reactive Protein
**p<0.001 statistically highly significant
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Apr 20, 2020
Manual Googling: Jun 23, 2020
iThenticate Software: Jul 28, 2020 (20%)
[1]. Nugent RA, Fathima SF, Feigl AB, Chyung D, The burden of chronic kidney disease on developing nations: A 21st century challenge in global healthNephron Clinical Practice 2011 118(3):c269-77.10.1159/00032138221212690 [Google Scholar] [CrossRef] [PubMed]
[2]. Braun L, Sood V, Hogue S, Lieberman B, Copley MC, High burden and unmet patient needs in chronic kidney diseaseInt J Nephrol Renovasc Dis 2012 5:151-63.10.2147/IJNRD.S3776623293534 [Google Scholar] [CrossRef] [PubMed]
[3]. Eknoyan G, The importance of early treatment of the anaemia of chronic kidney diseaseNephrology Dialysis Transplantation 2001 16(5):45-49.10.1093/ndt/16.suppl_5.4511509684 [Google Scholar] [CrossRef] [PubMed]
[4]. Levin A, Clinical epidemiology of cardiovascular disease in chronic kidney disease prior to dialysisSemin Dial 2003 16(2):101-05.10.1046/j.1525-139X.2003.16025.x12641872 [Google Scholar] [CrossRef] [PubMed]
[5]. Cheung AK, Sarnak MJ, Guofen Y, Dwyer JT, Heyka RJ, Rocco MV, Atherosclerotic cardiovascular disease risks in chronic hemodialysis patientsKidney Int 2000 58(1):353-62.10.1046/j.1523-1755.2000.00173.x10886582 [Google Scholar] [CrossRef] [PubMed]
[6]. Racki S, Zaputovic L, Vujicic B, Mavric Z, Grzetic M, Ravlic-Gulan J, Cardiovascular risk factors and diseases strongly predict hemodialyis treatment outcome in maintenance hemodialysis patientsCroat Med J 2005 46(6):936-41. [Google Scholar]
[7]. Gomez D, Baylis RA, Durgin BG, Newman AAC, Alencar GF, Mahan S, Interleukin-1beta has atheroprotective effects in advanced atherosclerotic lesions of miceNat Med 2018 24(9):1418-29.10.1038/s41591-018-0124-530038218 [Google Scholar] [CrossRef] [PubMed]
[8]. Tunon J, Back M, Badimon L, Bochaton-Piallat ML, Cariou B, Daemen MJ, Interplay between hypercholesterolemia and inflammation in atherosclerosis: Translating experimental targets into clinical practiceEur J Prev Cardiol 2018 25(9):948-55.10.1177/204748731877338429759006 [Google Scholar] [CrossRef] [PubMed]
[9]. Kendrick J, Chonchol MB, Nontraditional risk factors for cardiovascular disease in patients with chronic kidney diseaseNat Clin Pract Nephrol 2008 4(12):672-81.10.1038/ncpneph095418825155 [Google Scholar] [CrossRef] [PubMed]
[10]. Yao Q, Lindholm B, Stenvinkel P, Inflammation as a cause of malnutrition, atherosclerotic cardiovascular disease, and poor outcome in hemodialysis patientsHemodialysis Int 2004 8(2):118-29.10.1111/j.1492-7535.2004.01085.x19379407 [Google Scholar] [CrossRef] [PubMed]
[11]. Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannan RO, Fadl YY, Markers of inflammation and cardiovascular disease: Application to clinical and public health practise. A statement for healthcare professionals from the Centre for Disease Control and Prevention and the American Heart AssociationCirculation 2003 107(3):499-511.10.1161/01.CIR.0000052939.59093.4512551878 [Google Scholar] [CrossRef] [PubMed]
[12]. Stenvinkel P, Alvestrand P, Inflammation in end-stage renal disease: Sources, consequences and therapySemin Dial 2002 15(5):329-37.10.1046/j.1525-139X.2002.00083.x12358637 [Google Scholar] [CrossRef] [PubMed]
[13]. Nilsson J, CRP-marker or maker of cardiovascular disease?Arteriosclerosis, Thrombosis, and Vascular Biology 2005 25(8):1527-28.10.1161/01.ATV.0000174796.81443.3f16055753 [Google Scholar] [CrossRef] [PubMed]
[14]. Shrivastava AK, Singh HV, Raizada A, Singh SK, C-reactive protein, inflammation and coronary heart diseaseThe Egyptian Heart Journal 2015 67(2):89-97.10.1016/j.ehj.2014.11.005 [Google Scholar] [CrossRef]
[15]. Jialal I, Devaraj S, Venugopal SK, C-reactive protein: Risk marker or mediator in atherothrombosis?Hypertension 2004 44(1):06-11.10.1161/01.HYP.0000130484.20501.df15148294 [Google Scholar] [CrossRef] [PubMed]
[16]. Zimmermann J, Herrlinger S, Pruy A, Metzger T, Wanner C, Inflammation enhances cardiovascular risk and mortality in hemodialysis patientsKidney Int 1999 55(2):648-58.10.1046/j.1523-1755.1999.00273.x9987089 [Google Scholar] [CrossRef] [PubMed]
[17]. Yeun JY, Levine RA, Mantadilok V, Kaysen GA, C-reactive protein predicts all-cause and cardiovascular mortality in hemodialysis patientsAm J Kidney Dis 2000 35(3):469-76.10.1016/S0272-6386(00)70200-9 [Google Scholar] [CrossRef]
[18]. Pepys MB, CRP or not CRP? That is the questionArterioscler Thromb Vasc Biol 2005 25(6):1091-94.0.1161/01.ATV.0000169644.88847.2815923540 [Google Scholar] [CrossRef] [PubMed]
[19]. Mora S, Musunuruand K, Blumenthal RS, The clinical utility of high sensitivity C-reactive protein in cardiovascular disease and the potential implication of Jupiter on current practice guidelinesClinical Chemistry 2009 55:219-28.10.1373/clinchem.2008.10972819095730 [Google Scholar] [CrossRef] [PubMed]
[20]. Burtis CA, Ashwood ER, Bruns DE, Teitz Textbook of Clinical Chemistry 2012 5th editionUSAElsevier:21 [Google Scholar]
[21]. Windgassen EB, Funtowicz L, Lunsford TN, Harris LA, Mulvagh SL, C-reactive protein and high-sensitivity C-reactive protein: An update for cliniciansPostgraduate Medicine 2001 123(1):114-19.10.3810/pgm.2011.01.225221293091 [Google Scholar] [CrossRef] [PubMed]
[22]. Helal I, Zerelli L, Krid M, El Younsi F, Maiz HB, Zouari B, Comparison of C-reactive protein and high-sensitivity C-reactive protein levels in patients on hemodialysisSaudi Journal of Kidney Diseases and Transplantation 2012 23(3):477-83. [Google Scholar]
[23]. Ortega O, Rodriguez I, Gallar P, Carreno A, Ortiz M, Oliet A, Significance of high sensitivity C-reactive protein levels in pre-dialysis patientsNephrol Dial Transplant 2002 17(6):1105-09.10.1093/ndt/17.6.110512032204 [Google Scholar] [CrossRef] [PubMed]
[24]. Cockcroft DW, Gault MH, Prediction of creatinine clearance from serum creatinineNephron 1976 16(1):31-41.10.1159/0001805801244564 [Google Scholar] [CrossRef] [PubMed]
[25]. Eda S, Kaufmann J, Molwitz M, Vorberg E, A new method of measuring C-reactive protein, with a low limit of detection, suitable for risk assessment of coronary heart diseaseScand J Clin Lab Invest 1999 59(suppl 230):32-35.10.1080/00365519909168324 [Google Scholar] [CrossRef]
[26]. Andreas Pfützner A, Forst T, High-sensitivity C-reactive protein as cardiovascular risk marker in patients with diabetes mellitusDiabetes Technol Ther 2006 8(1):28-36.10.1089/dia.2006.8.2816472048 [Google Scholar] [CrossRef] [PubMed]
[27]. Jalal D, Chonchol M, Etgen T, Sander D, C-reactive protein as a predictor of cardiovascular events in elderly patients with chronic kidney diseaseJ Nephrol 2012 25(5):719-25.10.5301/jn.500004722038335 [Google Scholar] [CrossRef] [PubMed]
[28]. Lestariningsih L, Hardisaputro S, Nurani A, Santosa D, Santoso G, High sensitivity C-reactive protein as a predictive of intima-media thickness in patients with end-stage renal disease on regular hemodialysisInt J Gen Med 2019 12:219-24.10.2147/IJGM.S20550631354332 [Google Scholar] [CrossRef] [PubMed]
[29]. Kalkman DN, Aquino M, Claessen BE, Baber U, Guedeney P, Sorrentino S, Residual inflammatory risk and the impact on clinical outcomes in patients after percutaneous coronary interventionsEur Heart J 2018 39(46):4101-08.10.1093/eurheartj/ehy63330358832 [Google Scholar] [CrossRef] [PubMed]
[30]. Shlipak MG, Fried LF, Crump C, Bleyer AJ, Manolio TA, Tracy RP, Elevations of inflammatory and procoagulant biomarkers in elderly persons with renal insufficiencyCirculation 2003 107(1):87-92.10.1161/01.CIR.0000042700.48769.5912515748 [Google Scholar] [CrossRef] [PubMed]
[31]. National Kidney Foundation: K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification and stratificationAm J Kidney Dis 2002 39(suppl 1):S1-266. [Google Scholar]
[32]. Khunte SK, Kumar J, Khunte P, Role of high sensitivity C-reactive protein as a marker of inflammation and its prognostic significance in chronic kidney disease patientsInt J Adv Med 2019 6(2):335-34.10.18203/2349-3933.ijam20191137 [Google Scholar] [CrossRef]
[33]. Chauveau P, Level C, Lasseur C, Bonarek H, Combe C, Peuchant E, C-reactive protein and procalcitonin as markers of mortality in hemodialysis patients: A two-year prospective studyJ Ren Nutr 2003 13:137-43.10.1053/jren.2003.5001712671838 [Google Scholar] [CrossRef] [PubMed]
[34]. Tellingen A, Grooteman MPC, Schoorl M, Bartels PCM, Wee PMT, Nube MJ, Intercurrent clinical events are predictive of plasma C-reactive protein levels in hemodialysis patientsKidney Int 2002 62(2):632-38.10.1046/j.1523-1755.2002.00470.x12110028 [Google Scholar] [CrossRef] [PubMed]
[35]. Iseki K, Tozawa M, Yoshi S, Fukiyama K, Serum C-reactive (CRP) and risk of death in chronic dialysis patientsNephrol Dial Transplant 1999 14(8):1956-60.10.1093/ndt/14.8.195610462277 [Google Scholar] [CrossRef] [PubMed]