TAP block is a widely used modality of postoperative analgesia after abdominal and gynecological surgeries in which a local anaesthetic solution is injected into a plane between internal-oblique muscle and transversus-abdominis muscle [1,2]. It can somewhat avoid the use of intravenous opioid analgesics and hence avoid its complications like respiratory depression [3].
USG-guided TAP block is recommended due to its safety and reliability. With the help of USG imaging techniques, it is now possible to accurately position the needle and determine the distribution of a local anaesthetic in real time, which can improve the quality of nerve block, shorten its latency and reduce the minimum volume required to secure its success [4,5]. However, there are some limitations of USG which are well established, like inability to detect intravascular injection, failure to capture images of structures acoustically sheltered by bone or air and insufficient needle visibility, especially during deep injections with a sharp angle.
When in-plane technique is used, the shaft of needle is visualised as it passes parallel to the long axis of the scanning head directly under the USG beam [6]. However, the tip may be extremely difficult to visualise sonographically, especially with the in-plane approach [7]. Several methods for improving needle visibility have been introduced in the last 10 years, such as image-enhancement software, biopsy guides and the echogenic pattern of the needles themselves. Development of echogenic needles was one of the best methods to address this problem [8,9]. Very few studies have been done till date for comparison of echogenic needles with non echogenic needles and most of these studies involved needles designed for USG-guided tissue biopsy and not for regional anaesthesia [10,11]. Also, none of them have studied the impact of echogenic needles on postoperative analgesia.
So, this study was designed to compare visibilty and block characteristics (including improvement in postoperative analgesia) of echogenic vs. non echogenic needle for USG-guided TAP block. The visibility of block needles at the time of reaching TAP was primarily studied. The time taken for performance of block; number of needle redirections and skin punctures; block success rate/postoperative analgesia (postop VAS scores and total rescue analgesia required) and incidence of vascular punctures were also studied.
Materials and Methods
This randomised double-blind study was carried out at the Department of Anaesthesiology in collaboration with General Surgery and Surgical Gastroenterology at King George’s Medical University, Lucknow over a period of one year from November 2018 to October 2019 after Institutional Ethics Committee approval (No. 830/Ethics/18; Ref. code: 92nd ECM II B-Thesis/P26), Clinical Trials Registry- India (CTRI) registration (CTRI/2019/07/020423) and obtaining written/Informed consent from all the patients.
Sample size was calculated on the basis of proportion of single attempts in the two groups in a previous study by Brookes J et al., using the following formula [12]:
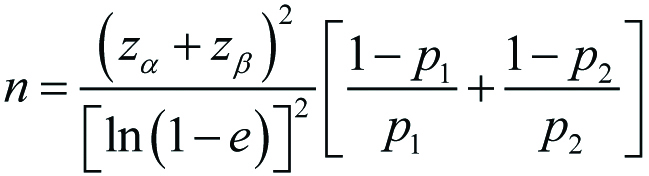
Where, p1=0.857 (85.7%; proportion of single attempt in first group), p2=0.763 (76.3%; proportion of single attempt in second group) and proportion difference e=0.25 considered to be clinically significant. Keeping an α-error of 5% and power of study 90%, the sample size came out to be 35 in each group.
Inclusion criteria: Seventy patients aged between 18-60 years, of either sex and American Society of Anaesthesiologists (ASA) status I and II, undergoing abdominal surgeries were enrolled in this study.
Exclusion criteria: Patients with a history of cardiac, respiratory, renal or hepatic disease; local infection at the site of block; psychological disorders; history of allergy to study medications; coagulation disorders and any other contraindication for general or regional anaesthesia were excluded from this study. Patients were randomly allocated to one of the two groups using a computer-generated list.
Group-E (n=35): Echogenic needle (SonoTAP needle; Pajunk©, Germany)
Group-NE (n=35): Non echogenic needle (Quincke’s needle)
Surgery was conducted under general/spinal anaesthesia as applicable. After completion of surgery, TAP block was performed bilaterally in all the patients using assigned needle as per group allocation and 20 mL of 0.25% Bupivacaine was deposited on each side.
All blocks were performed or directly supervised by a consultant anaesthetist with extensive experience in TAP block and was not involved in data collection for the study. The start and finish times of the block procedure were documented by research assistant. The number of attempts and redirections were also documented based on predetermined criteria (Every movement that followed a needle withdrawal of >2 cm was considered a redirection). The research assistant also documented the analgesia as measured by VAS score at 1 hour, 3 hours, 6 hours, 12 hours and 24 hours after TAP block. The scores of VAS ranged from 0-10, where 0 indicated no pain while 10 indicated worst imaginable pain. Rescue analgesia (IV paracetamol 1 g) was given whenever VAS score was found to be more than 5. Time of first rescue analgesia requirement and number of times rescue analgesia was required in 24 hours were also noted.
Recorded video clips were de-identified and sent along with the data collection form to a co-investigator who was blinded to group allocation. The observer was required to grade the visibility of the needle tip and shaft on initially reaching the TAP on a 3-point scale [12], as follows:
Poor: Needle tip and shaft barely distinguishable from the surrounding parenchyma;
Noticeable: Visualisation difficult but noticeably more echogenic than surrounding tissues;
Clear: Clearly visible with strong echogenicity compared with surrounding tissues.
The observer recorded the visibility of the needle tip and shaft once again after saline injection to confirm needle tip location. Parameters such as time from first needle contact with skin to reach the TAP plane, time from first needle contact with skin to complete deposition of drug (total procedure time), number of needle redirections, number of skin punctures made and incidence of vascular punctures were noted.
Statistical Analysis
Statistical analysis was done using SPSS Version 21.0. Data were presented as number (%) and mean±SD. Student t-test was used to test the significance of difference between two means. Other tests used were chi-square test and Mann-Whitney U test. Confidence level of the study was kept at 95%; hence p<0.05 indicated a statistically significant association.
Results
The two groups {Group-E (n=35) and Group-NE (n=35)} were comparable with respect to mean age (p=0.579), weight (p=0.273), height (p=0.877), ASA grade (p=0.501) and gender distribution (p=0.771) [Table/Fig-1]. There was no significant difference between two groups in terms of various comorbidities (anaemia, diabetes, hypertension, asthma, hypothyroidism) and drug-histories (insulin, metformin, amlodipine, telmisartan, thyronorm). All cases were conducted under general anaesthesia except five cases (14.3%) in Group-E and four cases (11.4%) in Group-NE which were conducted under spinal anaesthesia. There was no significant difference in the proportion of cases conducted under spinal anaesthesia between the groups (p=0.721) [Table/Fig-1].
Demographic profile (Age, Weight, Height, Gender and ASA Grade).
| Variables | Group-E | Group-NE | t-value* | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Age (years) | 38.63±9.44 | 40.17±13.38 | -0.56 | 0.579 |
| Weight (kg) | 57.34±7.84 | 59.29±6.83 | -1.11 | 0.273 |
| Height (cm) | 153.69±7.12 | 153.94±6.67 | -0.16 | 0.877 |
| No. (%) | No. (%) | Chi-sq† | p-value |
| Gender | Female | 27 (77.1%) | 28 (80.0%) | 0.09 | 0.771 |
| Male | 8 (22.9%) | 7 (20.0%) |
| ASA grade | I | 23 (65.7%) | 26 (74.3%) | 1.38 | 0.501 |
| II | 12 (34.3%) | 9 (25.7%) |
| Type of anaesthesia | Spinal | 5 (14.3%) | 4 (11.4%) | 0.13 | 0.721 |
| General | 30 (85.7%) | 31 (88.6%) |
*Independent t-test used; †Non-parametric chi-square test used; p-value <0.05 was significant; SD: Standard deviation; ASA: American Society of Anesthesiologists
Echogenic needle was found to be clearly visible in 29 out of 35 cases (82.9%) whereas non echogenic needle had no clear visibility in any of the 35 cases and poor visibility in 31 cases. Needle visibility on USG was significantly better in Group-E than Group-NE (χ2=57.24, p<0.001) [Table/Fig-2].
Comparison of visibility of block needle between the groups.
| Visibility of block needle | Group-E | Group-NE | Chi-sq* | p-value |
|---|
| No. (%) | No. (%) |
|---|
| Clear | 29 (82.9%) | 0 (0.0%) | 57.24 | <0.001 |
| Noticeable | 5 (14.3%) | 4 (11.4%) |
| Poor | 1 (2.9%) | 31 (88.6%) |
*Non-parametric chi-square test used; p-value <0.05 was significant
The mean time from first needle contact with skin to reach the TAP plane was 11.00±2.16 sec in Group-E which was significantly lesser (t=-16.89, p<0.001) than in Group-NE (24.31±4.14 sec) [Table/Fig-3]. The total procedure time i.e., time of first needle contact with skin to complete deposition of drug was also significantly lesser (t=-15.76, p<0.001) in Group-E than in Group-NE (26.94±4.59 sec vs. 46.66±5.81 sec) [Table/Fig-3]. There was no incidence of vascular puncture in any of the groups.
Comparison of time taken for performance of block between the groups.
| Time (Sec) | Group-E | Group-NE | t-value* | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| From first needle contact with skin to reach TAP plane | 11.00±2.16 | 24.31±4.14 | -16.89 | <0.001 |
| From first needle contact with skin to complete deposition of drug | 26.94±4.59 | 46.66±5.81 | -15.76 | <0.001 |
*Independent t-test used; p-value <0.05 was significant; SD: Standard deviation; TAP: Transversus-Abdominis-Plane
The mean number of needle redirections was 2.11±1.02 in Group-E which was significantly lesser (t=-11.21, p<0.001) than Group-NE (4.91±1.07) [Table/Fig-4]. Mean number of skin punctures was also lesser in group-E as compared to Group-NE (1.17±0.45 vs. 1.46±0.66) and the difference was statistically significant (t=-2.12, p=0.038) [Table/Fig-4].
Comparison of needle redirection and skin punctures between the groups.
| Group | Group-E | Group-NE | t-value* | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| No. of needle redirections | 2.11±1.02 | 4.91±1.07 | -11.21 | <0.001 |
| No. of skin punctures | 1.17±0.45 | 1.46±0.66 | -2.12 | 0.038 |
*Independent t-test used; p-value <0.05 was significant; SD: Standard deviation
VAS score for pain was found to be less in group-E as compared to group-NE throughout the study and the differences were statistically significant at all points of time i.e., after 1 hour (p=0.001), 3 hours (p=0.010), 6 hours (p=0.039), 12 hours (p<0.001) and 24 hours (p<0.001) after TAP block [Table/Fig-5].
Comparison of VAS score between the groups.
| VAS score | Group-E | Group-NE | Mann-Whitney test |
|---|
| Mean±SD | Mean±SD | z-value* | p-value |
|---|
| 1 hour of TAP block. | 3.60±0.85 | 4.31±0.87 | -3.35 | 0.001 |
| 3 hour of TAP block. | 3.89±0.76 | 4.49±1.04 | -2.58 | 0.010 |
| 6 hour of TAP block. | 3.83±0.89 | 4.43±1.20 | -2.06 | 0.039 |
| 12 hour of TAP block. | 4.17±1.18 | 5.86±1.06 | -5.06 | <0.001 |
| 24 hour of TAP block. | 3.71±1.43 | 5.00±1.08 | -3.58 | <0.001 |
*Mann-Whitney U test used; p-value <0.05 was significant; SD: Standard deviation; TAP: Transversus-Abdominis-Plane
Postoperative analgesia required in 24 hour was lesser in group-E as compared to group-NE and the difference was statistically significant (p<0.001). Time of first rescue analgesia required was earlier in group-NE as compared to group-E and the difference was statistically significant (p<0.001) [Table/Fig-6].
Comparison of rescue analgesia requirement between the groups.
| Rescue analgesia | Group-E | Group-NE | t-value* | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Total number of doses required in 24 hours | 1.77±0.69 | 3.26±0.66 | -9.23 | <0.001 |
| Time (hours) of first rescue analgesia required | 10.03±1.64 | 8.43±1.65 | 4.07 | <0.001 |
*Independent t-test used; p-value <0.05 was significant
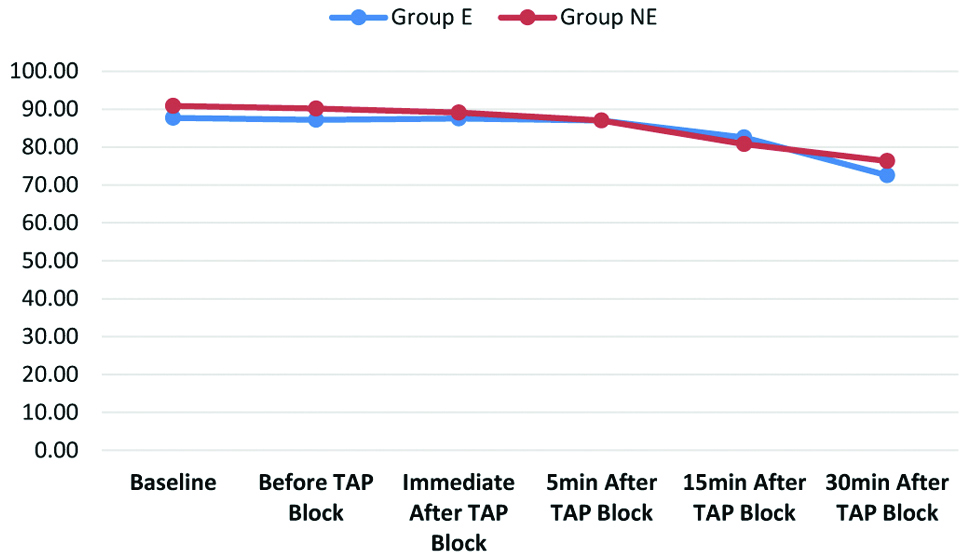
On comparing the Heart Rate (HR) between the groups, no significant differences were found at baseline, before and after TAP block except at 30 minutes after TAP block when the mean HR of group-NE was much more than the group-E (p=0.044), [Table/Fig-7] (Student’s t-test).
Comparison of heart rate between the groups.
TAP: Transversus-Abdominis-Plane
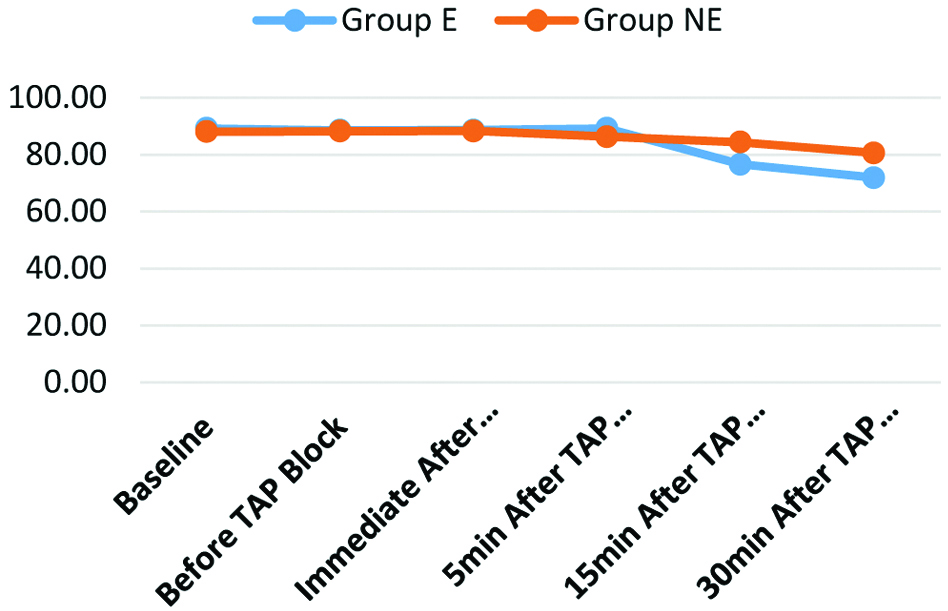
No significant difference was found in SBP at all times but DBP showed fluctuation at 30 minutes after TAP block (p=0.007), where the mean DBP of group NE was much more than group E. On comparing the Mean Arterial Pressure (MAP) between the groups, no significant difference was found between the groups except at 15 minutes after TAP block (p<0.001) and 30 minutes after TAP block (p<0.001), where the mean MAP of group-NE was much more than group-E [Table/Fig-8] (Student’s t-test).
Comparison of MAP between the Groups.
TAP: Transversus-Abdominis-Plane
Discussion
Potent postoperative analgesia is very important as it helps patients to bear the surgical stress. It also allows early ambulation and limits many complications like deep vein thrombosis and lung atelectasis [13,14]. Various methods are used for postoperative analgesia which includes parenteral opioids and NSAIDS, infiltration of local anaesthetic agents, dermal patches, patient controlled analgesia, epidural catheters etc.
TAP block is a widely used modality of postoperative analgesia providing significant analgesic effect, especially between T8 to L1 level; hence, is perfectly suited for abdominal and gynecological surgeries [1]. It was first introduced by Rafi AN in 2001 when it was performed using landmark guided technique via the triangle of Petit in order to achieve a field block [15]. They injected a local anaesthetic solution between the internal-oblique and transversus-abdominis muscle planes so as to block the afferents of thoracolumbar nerves originating from the T6 to L1 spinal roots which run into this plane. This provides analgesia to the anterolateral abdominal wall, where midline incision causes severe postoperative pain [2].
USG-guided TAP block is recommended due to its safety and reliability. USG-guidance improves the outcome of TAP block as it provides better localisation of the plane for blockade. The needle can be visualised when it passes parallel to the long axis of the scanning head directly under the USG beam in the in-plane technique; however, its tip may be extremely difficult to visualise sonographically. Several methods for improving needle visibility have been introduced in the last 10 years, such as image-enhancement software, biopsy guides and the echogenic pattern of the needles themselves.
There are various other factors which affect needle visibility. Acuteness of insertion angle and presence of kerfs and grooves have been reported to improve needle visibility whereas conical tips are known to have poor echogenic performance [9,16]. Other factors that may interact with echogenicity, include a miniature air gap between the needle stylet and cannula or the presence of any lubrication layers or coatings [17].
Schafhalter-Zoppoth II et al., had done a study in 2004 to assess factors that influence USG visibility of needles used in regional anaesthesia [18]. In their study, best USG visibility was exhibited by Hustead tip needles. Insertion of a medium size guide wire also increased USG visibility of the needle tip. Imaging in long axis provided better USG visibility when the needle was inserted at shallow angles (<30 degrees) whereas short-axis imaging provided best results at steeper needle insertion angles (>60 degrees). They suggested many factors that can enhance USG visibility of regional block needles which may be considered to improve safety and success of USG-guided regional blocks.
A new ‘texturing method’ developed in an attempt to improve the ultrasonic image of the nerve block needles were studied by Deam RK et al., [10]. They found improved visibility with this needle and suggested this type of needle to assist in performance of USG-guided regional anaesthesia by the anaesthetist. The need to optimise the echogenicity of needles used for USG guided nerve blocks was also suggested by Maecken T et al., [19].
For safe and successful USG-guided peripheral nerve block, it is important to visualise the needle. However, there are several factors which hamper accurate and consistent needle tip visualisation, the difficulty of needle-beam alignment being one of them. Chin KJ et al., suggested maintenance of a large needle-beam angle where possible, in addition to the use of surrogate markers of tip location like hydrolocation and tissue movement [8]. They suggested future directions for research and development to improve visualisation including development of more echogenic needles, and advances in USG imaging technology, such as 3-dimensional USG, and the use of colour Doppler to identify a moving needle tip. Rominger MB et al., had done a study in 2017 to evaluate needle visibility in USG under contrast mode conditions. Besides other factors, they also found the use of echogenic tip to improve the visibility of needle [20].
Use of echogenic needles seems to be the best method to increase needle visibility during USG-guided blocks. Echogenic needles are engineered to increase the reflection of US wave back towards the transducer thus increasing visibility [8,9].
In the present study, bilateral TAP-block using echogenic needle in group-E and non echogenic needle in group-NE was given after completion of surgery. The study used 20 mL of 0.25% bupivacaine on each side in both the groups which was based on previous study conducted by Hutchins J et al., [21]. Schafhalter-Zoppoth II et al., had indicated that the most important variable influencing needle visibility is the anaesthetist’s skill in using and placing the USG probe and needle [18]. Therefore in the present study, all blocks were performed by the same experienced anaesthetist, in order to gain most reliable results across the groups.
In the present study, needle visibility on USG was significantly better in Group-E than Group-NE (p<0.001). Echogenic needle was found to be clearly visible in 29 out of 35 cases (82.9%) whereas non echogenic needle had poor visibility in 31 out of 35 cases (88.6%).
A similar study was done by Guo S et al., in 2012 to compare the visibility of two new echogenic needles (Pajunk and Braun) with a standard non echogenic needle in a Thiel cadaver model [22]. The Pajunk echogenic needle was more visible than Braun standard needle in-plane (p=0.04) and as compared to Braun echogenic and Braun standard needles out-of-plane (p=0.02). The Pajunk echogenic needle was concluded to offer the best visibility for USG-guided regional anaesthesia. Uppal V et al., in their study, had also found pajunk echogenic needle to have better visibility when compared with the non echogenic needle when inserted at 60° and 70° angles, with or without beam steering [23].
Results of the present study also supported the study of Abbal B et al., who had found improved physician comfort, image quality, needle visibility and visualisation time with the use of needles with enhanced echogenicity during USG-guided procedures in phantoms and axillary nerve blocks using insertion angles of 30-45° and ≥45° [24].
Similar to the present study, Nakagawa K et al., had also conducted a study to compare the visibility of a non echogenic needle with three different echogenic needles (Hakko (HK), Unisis (UN) and B. Braun) inserting each of them 10 times at 45° and 30° into an USG phantom. At each insertion angle, objective visibilities of shaft of all the echogenic needles were higher than the non echogenic needle. According to their results, they concluded that the echogenic needles, particularly the BB and UN needles, can maintain high visibility when used with older ultrasonic devices. They strongly recommended combination with electrical stimulation for older devices to maintain the safety and certainty of USG-guided nerve blocks [25].
In the present study, the mean time of first needle contact with skin to reach the TAP and time of first needle contact with skin to complete deposition of drug in group-E were much lesser than in group-NE and the difference was highly significant (p<0.001). These findings of the present study are in agreement with that of the study by Duger C et al., in which they demonstrated shorter block performing times, shorter sensory and motor block onset times, a longer sensory and motor block duration and a higher patient and surgeon satisfaction score when compared to non echogenic needles in USG guided axillary brachial plexus block [26].
Brookes J et al., had done a study to compare the visibility of echogenic and non echogenic block needles and catheters in proximal sciatic blocks in patients undergoing total knee joint arthroplasty [12]. They found Echogenic group required shorter procedure time {274 s vs. 344 s (p=0.016)}. They concluded that the procedure time and patient discomfort when using echogenic needles and catheters are much lesser than the use of a stimulating catheter system. This finding is similar to the finding of the present study.
In the present study, the mean number of needle redirection and the mean number of skin punctures were significantly lower in group-E than group-NE (p<0.001). Brookes J et al., in his study concluded that the echogenic group required less needle redirections (p=0.009) and lesser patient discomfort (p=0.012) [12].
Previous studies on comparison of echogenic vs. non echogenic needles have not focussed much on comparison of postoperative analgesia. However, in the present study we also noted VAS scores and requirement of rescue analgesia in postoperative period and found these to be significantly lesser in Group-E as compared to Group-NE at all times. This comparison was not done in earlier studies on USG-guided TAP block. However, in the study on USG-guided axillary brachial plexus block, Duger C et al., did not find any significant improvement in postoperative analgesia (VAS) score at 12 hour with the use of Echogenic needles [26].
Patients in both the groups in the present study were haemodynamically stable throughout study except for a little higher HR, DBP and MAP in group-NE as compared to group-E which was significant only at certain points of time. However, there was no incidence of hypotension or bradycardia, requiring intervention in any of the patients.
Limitation(s)
In the present study, sample size was not large enough to represent population from which it was obtained. Another limitation was the use of VAS score for assessing pain which is a subjective parameter for evaluating outcomes and varies from person to person. This could have caused some bias in assessment of postoperative analgesia in the study. Thirdly, the echogenic needle used in the study was relatively expensive as compared to non echogenic needle. So it cannot be advocated in all the settings especially in patients from economically weaker sections.
Conclusion(s)
From this study, it was concluded that the use of echogenic needle for USG guided TAP block provides much better visibility of the needle tip resulting in less time for performance of blocks, less needle redirections, better block characteristics and better safety profile as compared to non echogenic needle. Besides these, it also resulted in better analgesia in the study as evident by lesser VAS scores and lesser requirement of rescue analgesia postoperatively. So, the use of echogenic needles for performance of USG guided TAP block is advocated in all the patients provided there are no financial constraints.
*Independent t-test used; †Non-parametric chi-square test used; p-value <0.05 was significant; SD: Standard deviation; ASA: American Society of Anesthesiologists
*Non-parametric chi-square test used; p-value <0.05 was significant
*Independent t-test used; p-value <0.05 was significant; SD: Standard deviation; TAP: Transversus-Abdominis-Plane
*Independent t-test used; p-value <0.05 was significant; SD: Standard deviation
*Mann-Whitney U test used; p-value <0.05 was significant; SD: Standard deviation; TAP: Transversus-Abdominis-Plane
*Independent t-test used; p-value <0.05 was significant