Pterygium is a degenerative, fibro-vascular, sub-epithelial connective tissue overgrowth of bulbar conjunctiva on to the cornea, commonly prevalent in hot dry climate [1]. Quiescent pterygium is harmless but active pterygium causes many discomforts such as foreign body sensation, ocular redness, irritation, astigmatism and restriction of ocular motility. Indications for pterygium excision are threatened visual axis, discomfort or cosmesis. Major limitation of pterygium excision is high recurrence rate, which can go up to 89% if no adjuvant treatment is done along with bare sclera excision. Operating on a recurrent pterygium is more difficult because of corneal thinning and scarring of the tissue [2]. Various adjuvant therapies are being used for prevention of its recurrence, however reported success rates vary widely [2,3]. MMC and limbal CAG are most commonly used adjunctive modalities to reduce the recurrence. Due to the antimitotic property radiomimetic action, MMC damages cells by cross linking DNA and inhibits synthesis of DNA, RNA and protein. In past it has been used intraoperatively or postoperatively in various concentrations ranging from 0.02% to 2% [4]. The optimal dosage and duration of administration should be titrated as increased exposure of MMC is associated with higher risk of complications [5].
CAG is a safe method as an adjunct to pterygium excision. Limbal stem cells act as a barrier to the conjunctival cells migrating on to the corneal surface [6,7]. CAG covers the injury site of sclera and replenishes limbal stem cells that have a definite role in the pathogenesis of pterygium [8]. Graft can be secured in place with the help of sutures, but it is a time taking procedure and also associated with suture related complications like infection, foreign body sensation, chronic inflammation or granuloma formation [9]. Currently, usage of plasma derived fibrin glue is favoured above suture as it is less time consuming, comfortable to the patient and have decreased complications but is sometimes associated with prior disease transmission and anaphylaxis in susceptible individuals [10]. So, suture and glue both have their own pros and cons. Hence, CAG using patient’s own oozing blood as tissue adhesive after pterygium excision is a novel approach to resurface the exposed sclera.
This study was conducted to compare MMC 0.01% topical drops BD for five days with CAG using oozing blood as the adhesive after bare sclera pterygium excision, in terms of recurrence and complications associated with them. Any comparative study between these two methods has not been conducted so far to the best of our knowledge.
Materials and Methods
This was a prospective longitudinal cohort conducted in the Department of Ophthalmology, Muzaffarnagar Medical College, Muzaffarnagar, Uttar Pradesh, India, from January 2018 to January 2019. Initially, 112 eyes of 100 patients with primary nasal pterygium were enrolled for this study. Permission from the ethical committee (MMC/PO/2018/46) and signed informed consent from all the patients were taken.
Inclusion criteria: Primary nasal pterygium causing diminution of vision either because of induced astigmatism or encroachment of pterygium onto the papillary area, cosmetic deformity, restricted ocular motility and irritation unrelieved by medical management.
Exclusion criteria: Patients having recurrent pterygium, previous ocular surgery and active ocular infection were not included in the study as re-surgery is usually accompanied by excessive scarring and may lead to increased intra or postoperative complications.
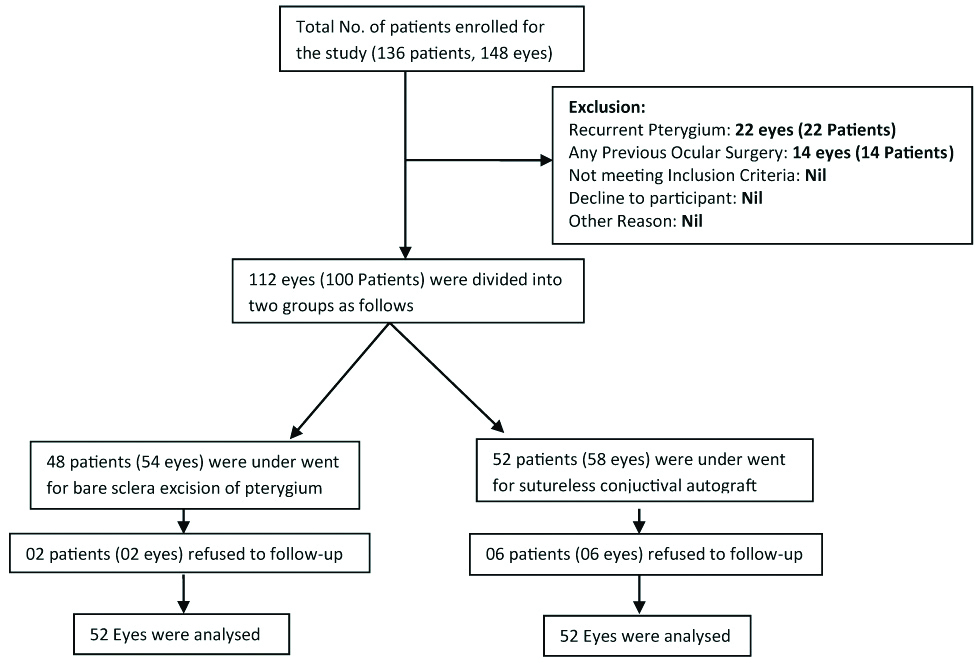
The prevalence rate of pterygium in Western UP is around 7.3% (taking as reference) [11] in the age group of 39-51 years, so the sample size was around 103.98 i.e., 104. Out of 100 (112 eyes) patients eight patients (8 eyes) did not turn up for follow-up till the end, so were also excluded from the study. A total of 104 eyes of 92 patients were divided into two groups (A and B) of 52 each on the basis of simple random technique as shown in the flow chart [Table/Fig-1]. Group A patients were prescribed 0.01% MMC drops BD for five days and Group B patients had CAG using autologous blood for fixation after pterygium excision.
Flow chart of the study participants.
Surgical Steps
All surgeries were performed in the major operation theatre by using peribulbar injection of 2% xylocaine with 1:200,000 epinephrine. Peribulbar injection provided excellent co-operation from the patients with respect to graft harvesting and its placement especially in sutureless cases. Head, neck and the body of pterygium were dissected and excised along with the thickened portion of conjunctiva and tenon’s capsule showing tortuous vasculature.
In the first group, minimal cautery was applied on the sclera to stop bleeding. Topical antibiotic ointment and steroid drops were instilled, followed by the eye patching. In the second group after pterygium excision, thin CAG including the limbal stem cells was dissected 0.5 mm oversized, from the supero-temporal quadrant after measuring the bare area of sclera with castroviejo calipers. Haemostasis was allowed to occur spontaneously without the use of cautery and any active bleeding was stopped by using direct tamponade. If no blood was available over bare sclera, small veins or capillaries were purposely pierced to encourage a thin layer of fresh blood to cover the bare sclera. The conjunctiva was fashioned over the oozing blood in the bare area, taking care of its placement limbal edge towards the limbus. Point to point apposition was affected by holding the edges with forceps for adequate duration to fix the graft followed by topical antibiotic ointment, steroid drops instillation and eye patching.
Postoperative Regimen
On the day of surgery all patients were prescribed oral Ibuprofen 400 mg twice daily, Vitamin C and B complex for five days. Vitamin C promotes wound healing and Ibuprofen reduces pain and inflammation. On the 1st postoperative day the eye dressing was removed. Patients with autograft were advised not to rub the eyes to prevent the dislodgement of the graft. Topical Fluorometholone six times per day and Moxifloxacin four times per day were given to all the patients for two weeks. Along with the above treatment, patients of the first group were also prescribed freshly prepared 0.01% MMC eye drops twice daily for five days. Fluorometholone was tapered over six weeks and Moxifloxacin was discontinued after two weeks. The patients were followed-up postoperatively on day 1, day 3, day 7, one month, three months, six months and one year.
Statistical Analysis
Statistical analysis was done by using SPSS software version 16. Data were expressed as mean+SD. Student’s t-test were applied wherever applicable. A p-value <0.05 were considered statistically significant.
Results
A total of 104 eyes of 92 patients attending the Ophthalmology OPD were included in this study. Eyes were randomised into two groups of 52 each (A and B). Group A was surgically treated with bare sclera excision of pterygium, followed by 0.01% MMC eye drops BD for five days and group B underwent CAG fixed with the help of autologous blood.
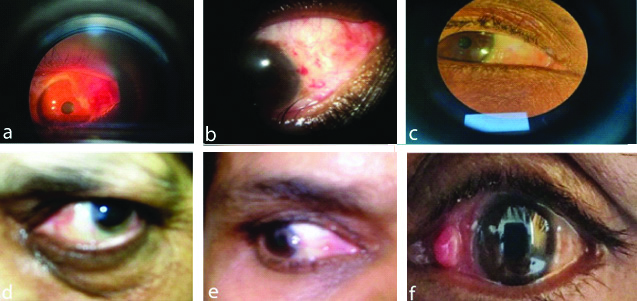
In group A [Table/Fig-2a-f], along with the recurrence [Table/Fig-2e], 1 (1.92%) patient presented with corneal thinning, 1 (1.92%) with scleral thinning and 2 (3.85%) with avascular sclera [Table/Fig-2d] at the 7th day of follow-up but these complications spontaneously resolved till the end of the month. Only 1 (1.92%) patient appeared with granuloma [Table/Fig-2f] on the 90th day of evaluation and it resolved with the use of antibiotic steroid combination eye drops in next three weeks. No long term or persistent complication was found in any of the patients with this treatment regime [Table/Fig-3].
Images of Group A. a) Preoperative image; b) One week postoperative image; c) Four weeks postoperative image; d) Avascular sclera; e) Recurrent; f) Granuloma.
Complications in group A.
| Complications | Patients | Percentage |
|---|
| Corneal thinning | 1 | 1.92% |
| Scleral thinning | 1 | 1.92% |
| Avascular sclera | 2 | 3.85% |
| Granuloma | 1 | 1.92% |
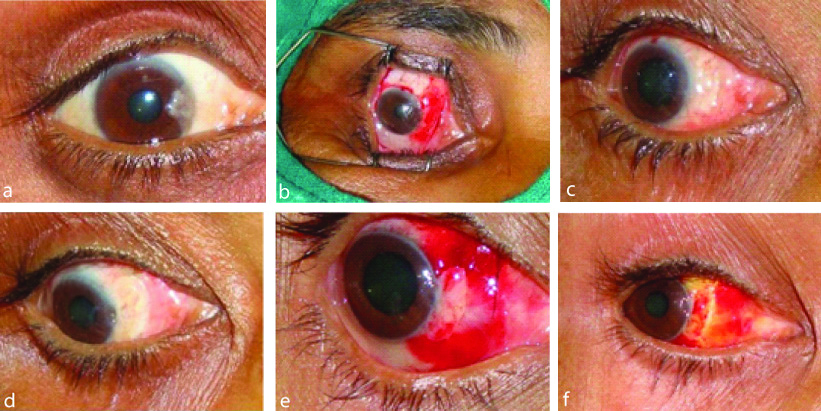
In group B [Table/Fig-4a-f] medial edge graft retraction [Table/Fig-4f], graft oedema, sub-conjunctival graft haemorrhage [Table/Fig-4e] and granuloma were observed in 18 (34.62%), 8 (15.38%), 5 (9.62%) and 1 (1.92%) patients, respectively. Graft retraction was seen in all the 18 (34.62%) patients within one week postoperatively. The graft oedema was observed on 1st or 3rd day and disappeared by the 7th postoperative day. None of the patients developed button hole of conjunctival graft, injury to medial rectus, excessive bleeding, dellen, pyogenic granuloma, symblepharon formation or scleral necrosis [Table/Fig-5].
Images of a group B. a) Preoperative pterygium; b) Intraoperative; c) One week postoperative; d) Four weeks postoperative; e) Graft oedema and haemorrhage; f) Graft retraction.
Complications in group B.
| Complications | Patients | Percentage |
|---|
| Graft retraction | 18 | 34.62% |
| Graft oedema | 8 | 15.38% |
| Sub-conjunctival graft haemorrhage | 5 | 9.62% |
| Granuloma | 1 | 1.92% |
As shown in the [Table/Fig-6], mean age of the patients was 45 years and 43 years in group A and B, respectively and the difference was statistically non-significant. In both the groups male preponderance was found. Duration of surgery was more in group B as autograft was taken and placed on the bare sclera as compared to group A.
Patient profile and surgery duration in group A and B.
| Variables | Group A | Group B | p-value |
|---|
| Age (Years) | 45±5.63 | 43±5.34 | 0.066 |
| Male: Female ratio | 60:40 | 58:42 | 0.84 |
| Mean Surgical time (minutes) | 10±5 | 20±5 | 0.0001 |
Total 3 patients had recurrence in one year of follow-up in group A, out of which first case appeared before the end of 1st month, second before the completion of 3rd month and the third case at the last follow-up. In group B only one case presented with recurrence at 6th month follow-up. The difference between recurrences in both the groups was statistically non-significant (p=1.04) [Table/Fig-7].
Comparison of recurrence in group A and B.
| Recurrence rate |
|---|
| Follow-up duration | Group A | Group B |
|---|
| 01 month | 1 (1.92%) | 0 (0%) |
| 03 months | 1 (1.92%) | 0 (0%) |
| 06 months | 0 (0%) | 1 (1.92%) |
| 01 year | 1(1.92%) | 0 (0%) |
| Total recurrences | 3 (5.77%) | 1 (1.92%) |
There were no intraoperative or postoperative complications requiring further treatment. Most of the patients complained of mild pain on bandage removal and this pain got subsided on subsequent visits. Postoperative best corrected visual acuity was not affected in any patient and cosmetically all the patients were satisfied after the final outcome.
Discussion
Recurrence of pterygium is the most common problem with the surgeons, after its excision. So, various adjunctive measures have been devised to prevent the recurrence of pterygium after surgical excision, among which administration of MMC eye drop has been reported to be an effective adjunct to surgical excision [12]. Multiple side-effects have been reported after the use of 0.1% and 0.04% MMC eye drops. A study by Singh G et al., reported corneal oedema, corneal perforation, scleral calcification, correctopia, iritis, sudden onset mature cataract, severe secondary glaucoma, incapacitating photophobia and pain in their study but were not seen in present study because low strength (0.01%) of MMC was used [13]. Two studies done with 0.02% MMC eye drops postoperatively BD for five days which was double the strength of present study have concluded that MMC should be used judiciously because of the potential long term risk of sight threatening complications [14,15]. Scleral ulceration was reported in some studies where MMC was used in a concentration of 0.02% BD for five days [16], QID (four times a day) for seven days [17] and 0.04% TDS (thrice times a day) for seven days [18] after pterygium excision but none of the patient came up with sclera ulceration in present study with 0.01% MMC drops. Corneal dellen or iritis was not encountered in any of the patients but was found with postoperative use of MMC 0.02% QID for seven days in a study conducted by Qguz H et al., [18]. Few studies have also concluded increased risk of scleral thinning with higher concentration of MMC usage [19,20] and it was found in 1 (1.92%) patient in present study too. This shows that if lower dose of MMC is used for a smaller duration, chances of complications are minimised. Usually recurrence of pterygium is seen most commonly within first six months after surgery and the same pattern was followed in present study also [21].
To fixate the conjunctiva using autologous blood as tissue adhesive after pterygium excision, was found to be technically more difficult but can be mastered with time. It bypasses the need of sutures and glue. It was observed that apposition of the lids to the bulbar conjunctiva provides a natural biological dressing and confers a unique wound healing environment. Graft retraction, was seen in 18 eyes (34.62%) in present study and was nearly same as seen with synthetic glue or other series with autologous blood [22]. As the chemosis resolved the retraction also disappeared automatically, there was no change in the final position of the graft. Tan D advocated that risk of graft retraction could be minimised with meticulous dissection of sub epithelial graft tissue [23]. Wit D et al., postulated that sutureless and glue free graft resulted in an even tension across the whole of the graft interface and no direct tension on the free graft edges resulting in reduced stimulus for the formation of subconjunctival scar [22]. A 0.5 mm oversized and as thin as possible conjunctival graft was taken to prevent the risk of graft retraction as described by Tan D [23].
This study has proved that 0.01% MMC BD for five days can be considered as a good option for pterygium management and also it has a comparable efficacy with CAG. Without using suture or fibrin glue, autograft can be successfully secured in place with excellent results and it can be recommended as the future treatment of pterygium.
Limitation(s)
Short duration and a small sample size can be seen as the limitation of this study because a larger sample size or longer follow-up might have brought some more recurrences in the patients.
Conclusion(s)
On the basis of this study it can be concluded that both, MMC 0.01% eye drops BD for five days after bare sclera pterygium excision and glue free or sutureless CAG adhered with the help of oozing blood are safe and effective in management of pterygium.