Neuroleptic Malignant Syndrome (NMS) is an emergency condition produced as an ill effect of certain drugs. Tetrad of symptoms includes fever, muscle rigidity, autonomic features and altered mental status. Pathophysiology underlying this condition is dopamine receptor blockade or depletion of dopamine. Author presented a case of 45-year-old female, alcoholic with symptoms of self-mutilating behaviour such as finger biting and tongue bites, elevated Creatine Phosphokinase (CPK) levels and no signs of autonomic dysfunction. Differential diagnosis included was malignant hyperthermia, neuroleptic malignant syndrome, serotonin syndrome, lethal catatonia, meningitis/encephalitis, heat stroke and anticholinergic toxicity. Final diagnosis of neuroleptic malignant syndrome was made according to Caroff SN and Mann SC criteria. She was treated with bromocriptine with an improvement in her condition. Clear workup including identification of other systemic and neuropsychiatric conditions with overlapping symptoms is important for accurate diagnosis of this condition.
Antipsychotic drugs, Autonomous condition, Mental disorder, Neural disorder, Self mutilation
Case Report
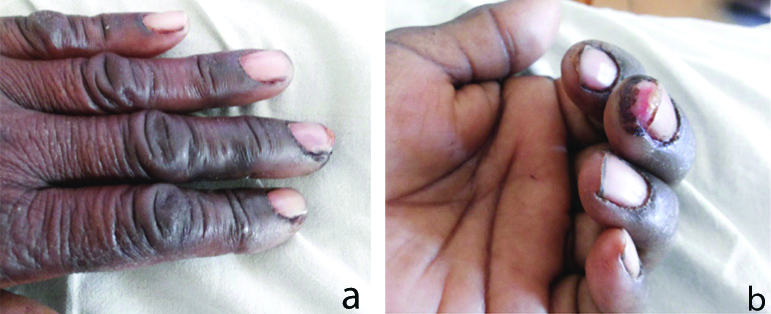
A 45-year-old female, chronic alcoholic presented with acute onset abnormal and self-mutilating behaviour in the form of finger biting [Table/Fig-1a,b] and a tongue bite. This was the first such episode. There was no history of seizure, head injury or drug intake. There were no symptoms of increased tone of limbs, abnormal sweating and involuntary movements.
a) Image showing injuries due to finger biting. b) Image showing self mutilation of fingers.
At the time of admission, the patient was conscious but not oriented. The patient was irritable and often agitated followed by period of somnolence. There was mild fever and dark urine after catheterisation. There were no features of autonomic dysfunction. There was no history of intake of antipsychotic medication. Patient was an alcoholic with no significant family history. The patient was accompanied by the son. The personal hygiene was good and patient was from a poor socio-economic background.
On examination, patient was conscious, delirious not oriented. There was no gaze restriction and dolls eye movement was intact. Signs and symptoms of chorea athetosis was present, however she was moving all the four limbs with some amount of rigidity. There was no neck stiffness. There were no features suggestive of autonomic dysfunction that was present.
On evaluation, the blood routine and electrolytes including renal parameters were normal but CPK was significantly elevated (35,000 IU/L). The Cerebrospinal fluid (CSF) parameters as well as Electroencephalogram (EEG) and Computed Tomography (CT) head were within normal limits. Iron levels were 85.3 microgram/dL. Diagnosis of Neuroleptic Malignant Syndrome (like) was made, according to the Caroff SN and Mann SC criteria, despite the absent of dysautonomic features and absence of history of intake of anti psychotic medications as the patient had fever, mild rigidity, encephalopathy and elevated CPK [1]. Differential diagnosis considered at this point was malignant hyperthermia, serotonin syndrome and neuroleptic malignant syndrome. Final diagnosis of neuroleptic malignant syndrome was made according to Caroff SN and Mann SC criteria [1].
The patient was shifted to ICU, started on supportive treatments. The initial treatment included cooling by keeping her in an air conditioned room with fan, hydration and use of bromocriptine, even though the patient has not received any antipsychotics. She was treated with tablet bromocriptine 2.5 mg thrice daily. Patient’s condition gradually improved, fever subsided, rigidity resolved and sensorium returned to normal after one week. The serial CPK levels showed decreasing trend from 35,000 IU/L to 10,000 IU/L to 3000 IU/L, then 900 IU/L and resolved to normal, 180 IU/L after one week.
The patient was conscious, completely oriented, showed no symptoms of Self-Injurious Behaviour Syndrome (SIBS) in the hospital and at the time of discharge. The rigidity resolved completely. Patient did not come back for a follow-up to the hospital and therefore, no records of CPK and symptom review after complete recovery are available. Hence, consent could not be obtained from the patient and careful selection of images were done, so that the patient anonymity is maintained. However, reporting the case is important for the benefit of medical literature.
Discussion
Neuroleptic malignant syndrome is a medical emergency. It is caused due to an idiosyncratic reaction, mainly to antipsychotic drugs. Change in dosage, polypharmacy or even stable doses of the prescribed drug have led to the incidence of this syndrome. It takes 2-8 weeks after initiation of the drug for symptoms to manifest [2]. Delay J et al., first published a report on Neuroleptic malignant syndrome in association with Haloperidol [3]. Since then, multiple cases have been brought to notice with respect to other antipsychotic medications, including typical and atypical classes, antiemetic drugs and neuroleptics [2].
The underlying pathophysiology of this condition not only includes D2 receptor blockage by drugs in the central nervous system, but is also contributed to dopamine levels in the brain. Parkinson Hyperpyrexia Syndrome (PHS) is caused due to relative dopamine deficiency and even a single missed dose of syndopa on a patient with parkinsonism can precipitate PHS [4]. This patient did not have parkinsonism and neither had a history of syndopa intake. Decrease in serum iron levels, an acute phase reactant has contributed to the neuroimmunological basis of a rare case of NMS in a patient with Steven Johnson Syndrome induced by carbamazepine [5,6]. In this case, the patient’s iron studies done and was normal, therefore an imbalance in serum iron levels didn’t support the underlying mechanism for onset of NMS like symptoms in the patient. Therefore, the author had to look at other pathophysiological mechanisms and consider other differential diagnosis at this point. Different diagnosis initially considered was malignant hyperthermia, serotonin syndrome, lethal catatonia, meningitis/encephalitis, heat stroke and anticholinergic toxicity [5]. Malignant hyperthermia was ruled out as there was no history of volatile anaesthetic, succinylcholine use and no generalised rigidity. Serotonin syndrome was ruled out as there was no inciting factor and no gastrointestinal manifestations. Lethal catatonia was ruled out in the patient due to absent of characteristic features such as immobility, waxy flexibility and mutism. Meningitis was ruled out due to normal CSF analysis on lumbar puncture. There were no risk factors or skin changes and headache to make a diagnosis of heat stroke. There was no history of inciting factors such as drugs with anticholinergic properties to cause anticholinergic toxicity.
There are multiple diagnostic criteria put forth for timely recognition of this condition including Caroff SN and Mann SC, Levenson JL criteria and the DSM V criteria [1,7,8]. Defining symptoms of this syndrome include fever, muscle rigidity, autonomic features and altered mental status. This condition may have overlapping symptoms with other condition such as malignant hyperthermia, serotonin syndrome, PHS and central cholinergic crisis. Diagnosis of neuroleptic malignant syndrome in this patient was made according to Caroff SN and Mann SC criteria [1].
SIBS synonymous with Deliberate Self-Harm (DSH) accounts for behavioural patterns due to various aetiologies that result in tissue damage that is self-inflicted without the intensions of suicide. It can be classified into different types based on severity and timing into: a) mild and isolated; b) moderate and repetitive; c) very severe and isolated forms [9]. Most cases of SIBS are caused due to some underlying psychiatric condition as reported by Rao KN et al., [9]. Neurological disorders presenting with self-mutilating symptoms are metabolic conditions like lesch-Nyhan syndrome [10] presenting with biting of lips, hands and fingers, head banging; core Neuroacanthocytosis syndrome like Chorea-Acanthocytosis presenting with characteristic feeding dystonia, tongue and lip biting and exceptional cases of McLeod Neuroacanthoctosis syndrome [11].
There are multiple risk factors and predisposing conditions that play a triggering role in the development of NMS. These include environmental causes, other co-existing medical conditions and family history of the patient [1]. Alcohol is one such important risk factor to be borne in mind. Muscle toxicity and sensitivity is another proposed aetiopathogenesis that is involved in NMS, and alcohol is known to cause effect on the muscle directly due to ethanol toxicity and indirectly due to underlying malnutrition in such patients. Sensitivity to neuroleptic drugs is seen to be higher in alcoholic patients [12]. Panagariya A et al., reported one such case of NMS in an alcoholic patient [13]. Farooq H et al., reported a case of alcohol withdrawal mimicking NMS in which the patient presented with elevated body temperature, autonomic dysfunction, altered consciousness, rigidity, elevated creatine kinase (401 IU/L), electrolyte imbalance and myoglobinuria with normal imaging studies [13,14]. History of last alcohol intake 2 days ago and drastic improvement on starting benzodiazepines was seen. Therefore, diagnosis of alcohol withdrawal presenting as a rare case of severe adrenergic surge was made. Another case of NMS was reported by Minamisawa S et al., in a patient with history of chronic alcoholism and liver cirrhosis [15]. Use of neuroleptic drug (Haloperidol) in this patient, precipitated NMS features within a short span of time.
Pharmacotherapy for reversal of symptoms most commonly includes dopamine agonist like bromocriptine, dantrolene and amantadine [2]. In this case, the patient with bromocriptine showed quick symptom relief and reversal to normal physiology.
This case of neuroleptic syndrome presenting with SIBS was a unique finding. What made this case even more interesting that, it was NMS with SIBS in an alcoholic patient with no history of antipsychotic drug. No such case has been reported so far.
Conclusion(s)
NMS is lethal emergency most commonly associated with intake of antipsychotic medications. NMS without intake of antipsychotic medications is a rare finding. Alcoholics are predisposed to NMS even at small doses of Antipsychotics and rarely even without the history of any antipsychotic drug intake. Authors have reported a case of NMS presenting as SIBS which was a unique finding and this case was the first of its kind. It was hypothesised that probably immunological cascade contributed to the development of NMS in this patient with no history of drug intake.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? NA
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jan 18, 2020
Manual Googling: Jun 30, 2020
iThenticate Software: Jul 28, 2020 (14%)
[1]. Caroff SN, Mann SC, Neuroleptic malignant syndromeMed Clin North Am 1993 77(1):185-202.10.1016/S0025-7125(16)30278-4 [Google Scholar] [CrossRef]
[2]. Tse L, Barr A, Scarapicchia V, Vila-Rodriguez F, Neuroleptic malignant syndrome: A review from a clinically oriented perspectiveCurrent Neuropharmacology 2015 13(3):395-406.10.2174/1570159X13999150424113345 [Google Scholar] [CrossRef]
[3]. Delay J, Pichot P, Lempiere T, Blissalde B, Peigne F, A nonphenothiazine and non-reserpine major neuroleptic, haloperidol, in the treatment of psychosesAnn Med Psychology (Paris) 1960 118:145-52. [Google Scholar]
[4]. Mohammed NB, Sannegowda RB, Hejamadi MI, Sharma B, Dubey P, Single Dose Does Matter! An interesting case of parkinsons hyperpyrexia syndromeJ Neurol Disord 2014 2(6):191 [Google Scholar]
[5]. Sharma B, Sannegowda RB, Gandhi P, Dubey P, Panagariya A, Combination of Steven-Johnson Syndrome and neuroleptic malignant syndrome following carbamazepine therapy: A rare occurrenceBMJ Case Report 2013. June 11 10.1136/bcr-2013-00890823761563 [Google Scholar] [CrossRef] [PubMed]
[6]. Anglin RE, Rosebush PI, Mazurek MF, Neuroleptic malignant syndrome: A neuroimmunologic hypothesisCan Med Assoc J 2010 (182):834-38.10.1503/cmaj.09144220696799 [Google Scholar] [CrossRef] [PubMed]
[7]. Levenson JL, Neuroleptic malignant syndromeAm J Psychiatry 1985 142(10):1137-45.10.1176/ajp.142.10.11372863986 [Google Scholar] [CrossRef] [PubMed]
[8]. American Psychiatric AssociationDiagnostic and Statistical Manual of Mental Disorders 2013 5th EdArlingtone, VAAmerican Psychiatric Publishing10.1176/appi.books.9780890425596 [Google Scholar] [CrossRef]
[9]. Rao KN, Sudarshan CY, Begum S, Self-injurious behaviour: A clinical appraisalIndian J Psychiatry 2008 50(4):288-97.10.4103/0019-5545.4475419823617 [Google Scholar] [CrossRef] [PubMed]
[10]. Jathar P, Panse AM, Jathar M, Gawali PN, Lesch-Nyhan Syndrome: Disorder of self-mutilating behaviourInt J Clin Pediatr Dent 2016 9(2):139-42.10.5005/jp-journals-10005-135027365935 [Google Scholar] [CrossRef] [PubMed]
[11]. Jung HH, Danek A, Walker RH, Neuroacanthocytosis SyndromesOrphanet J Rare Dis 2011 6(1):6810.1186/1750-1172-6-6822027213 [Google Scholar] [CrossRef] [PubMed]
[12]. Adnet P, Lestavel P, Krivosic-Horber R, Neuroleptic malignant syndromeBr J Anaesth 2000 85(1):129-35.10.1093/bja/85.1.12910928001 [Google Scholar] [CrossRef] [PubMed]
[13]. Panagariya A, Sharma B, Singh R, Agarwal V, Dev A, The neuroleptic malignant syndrome: A report of 14 cases from North IndiaNeurology India 2007 55:166-69.10.4103/0028-3886.3279317558126 [Google Scholar] [CrossRef] [PubMed]
[14]. Farooq H, Mohammad T, Farooq A, Mohammad Q, Alcohol withdrawal mimicking neuroleptic malignant syndromeCureus 2019 11(5):e469710.7759/cureus.4697 [Google Scholar] [CrossRef]
[15]. Minamisawa S, Tezuka T, Enomoto K, Nozaki Y, Funatomi H, Hatta Y, A case of neuroleptic malignant syndrome developed in liver cirrhosis patient addicted to alcoholJapanese Journal of Alcohol Studies and Drug Dependence 1991 26(5):367-72. [Google Scholar]