Primary Hyperparathyroidism (PHPT) is characterised by autonomously hyperactive parathyroid glands, usually resulting in hypercalcaemia that may or may not be symptomatic. The commonest cause of PHPT is parathyroid adenoma (80-85%). Other causes are parathyroid hyperplasia (5-15%) and carcinoma (<1%) [1-3]. Most parathyroid neoplasms are benign (i.e., adenomas) with inferior glands being relatively more frequently affected than superior glands [4,5]. Parathyroid adenomas are known to arise in ectopic sites in about 10% of all cases, including mediastinum (70%), within thyroid (20%), para- and retro-oesophageal soft tissue, carotid sheath and para-aortic regions [4]. Rarely, they may also be seen in oesophageal wall, pericardium, vagus and hypoglossal nerves or adjacent to angle of jaw [6]. Ectopic location of parathyroid glands results from aberrations during embryological migration of parathyroid glands from their sites of origin (3rd and 4th branchial clefts) to their definitive positions in neck and is more likely to occur in inferior parathyroids that migrate over longer distances [7]. Ectopic ITPAs are rare [8,9]. Preoperative diagnosis of this entity by ultrasound is possible [10,11] along with inputs from Sestamibi scintigraphy [12,13]; however its distinction from a thyroid nodule is difficult [14,15] and sensitivity is decreased in smaller adenomas and with co-existent thyroid disease.
Other factors such as operator experience and patient’s body habitus also play a role in imaging results [16,17]. ITPAs may be discovered sometimes only intraoperatively, on palpating the thyroid lobe on the side suspected by imaging studies to harbour the parathyroid adenoma. Smaller ITPAs may be missed, resulting in unsuccessful surgery. Hemi-thyroidectomy of the thyroid lobe with the intrathyroid adenoma is the preferred surgery. However, co-existent thyroid disease, diagnosed during preoperative imaging, also determines the extent of surgery. Although diagnostic challenges in ITPAs have been documented by various studies, there is a paucity of literature on the common histopathological features seen in these entities. The present study was done with the primary objective to estimate the proportion of ITPAs among all parathyroid adenomas diagnosed at a referral hospital in South India, and to summarise their histopathological features. The secondary objective was to assess their preoperative and intraoperative diagnostic rates, to depict the difficulties involved in their diagnoses.
Materials and Methods
This was a cross-sectional study of ITPAs, among all parathyroid adenomas diagnosed at the Department of General Pathology of Christian Medical College and Hospital, Vellore, Tamil Nadu, from January 2012 to December 2019, done with the approval of the Institutional Ethics Committee {IRB: 11890 (Retro) dated 27th February, 2019}.
ITPAs are defined as parathyroid adenomas situated within thyroid parenchyma. Adenomas completely embedded in thyroid tissue and thereby not distinctly evident on inspection were regarded completely intrathyroid. Adenomas embedded partly in thyroid were considered partially intrathyroid. Adenomas just adherent to thyroid surface were excluded [8]. Only conclusive adenomas, with postoperative normalisation of serum calcium and parathormone levels, were included in the study. The demography, presenting symptoms including neck swelling, details of imaging reports, serum calcium (corrected for albumin), phosphorus and parathormone levels, and intraoperative findings in all cases were reviewed and tabulated. Preoperative imaging included ultrasound of neck and Technetium-99m scintigraphy in all patients. In one patient (P4), who had preoperative work-up elsewhere, only final imaging impression (without details) and a few biochemistry assay results were available. The slides and available paraffin embedded tissue blocks were retrieved from archives to review the histological findings and tabulated with gross findings obtained from pathology reports.
Statistical Analysis
Descriptive statistics such as mean, standard deviation, median and inter-quartile range were used for age, biochemistry assays and maximum dimensions of ITPAs. Numbers and percentages were used for gender, symptoms, ITPA types and presence of concomitant thyroid disease. Fisher’s-exact test/Yates’ correction was used to assess the association between ITPA groups and presence of concomitant thyroid disease/neck swelling and gender. To compare age, biochemistry assay values and maximum dimensions across the ITPA groups, if the data followed normal distribution, Independent t-test was used, else Mann-Whitney U test was employed. The p-value <0.05 was considered as statistically significant. SPSS 21.0 version (SPSS Inc, Chicago, IL) was used for analysis.
Results
In the study period, there were 409 parathyroid adenomas, with 28 in ectopic locations (6.8%), including ten (35.7%) intrathyroidal ones (i.e., ITPAs), seven in mediastinal locations (25%; including five intra-thymic adenomas), four (14.3%) in right para-oesophageal region, two behind right carotid sheath (7.1%), two adjacent to left common carotid artery (7.1%) and one each in right retro-oesophageal (3.6%), supra-sternal (3.6%) and retrosternal (3.6%) regions. ITPAs occurred in seven females and three males, with a mean age of 44.1±10.9 years. Eight patients (80%) had hypercalcaemia manifestations, most commonly renal stones (75%). Four patients (40%) had neck swellings at presentation (all of whom had concomitant thyroid disease, on histopathological evaluation). The various characteristics of ITPA patients were summarised [Table/Fig-1,2].
Demography, Clinical features and preoperative biochemistry of ITPAs.
| Pat. No. | Age/Sex | Clinical features | Ca2+ mg/dL | PO42- mg/dL | PTH pg/mL |
|---|
| P1 | 48/M | R, N | 12.4 | 1.7 | 721.8 |
| P2 | 28/F | M | 12 | 1.8 | 1032.9 |
| P3 | 38/F | R, P | 12.8 | 1.2 | 579.8 |
| P4* | 50/F | R, N | 11.2 | N/A | 323 |
| P5$ | 47/M | R, N | 13.2 | 3.8 | >1900 |
| P6 | 46/F | R, M, P | 10.8 | 1.9 | 306.8 |
| P7# | 44/F | N | 10.4 | 2.7 | 136.6 |
| P8 | 28/M | P | 13.2 | 1.8 | 618.2 |
| P9 | 47/F | R | 11 | 2.2 | 374.5 |
| P10 | 65/F | No symptoms | 11.5 | 3.4 | 186.8 |
R: Renal disease; M: Musculoskeletal symptoms; P: Pancreatitis; N: Neck swelling
Grey-shaded Rows- Partial ITPAs, Unshaded rows- Complete ITPAs
*Patient (specimen) referred from another hospital
$Clinically suspected as parathyroid carcinoma
#Patient with neck swelling and osteopenia detected by DEXA scan
Ca2+- Serum calcium (corrected for albumin), PO42- Serum Phosphorus, PTH-Serum Parathormone levels
Summary of characteristics of ITPA patients. (n=10)
| Variables | n (%) |
|---|
| Age (yrs) | Mean: 44.10±10.87Median: 46.50 (35.5, 48.5) |
| Type |
| pITPA | 6 (60.0) |
| cITPA | 4 (40.0) |
| Gender |
| Male | 3 (30.0) |
| Female | 7 (70.0) |
| Neck swelling |
| Present | 4 (40.0) |
| Absent | 6 (60.0) |
| Serum Calcium | Mean: 11.85±1.02Median: 11.75 (10.95,12.90) |
| Sr. Parathormone | Mean: 618.04±525.86Median: 477.15 (276.80, 799.57) |
| Sr. Phosphorus | Mean: 2.28±0.86Median: 1.90 (1.75, 3.05) |
| Maximum size (cm) | Mean: 1.95±1.00Median: 1.70 (1.15, 2.82) |
| Thyroid disease |
| Present | 4 (40.0) |
| Absent | 6 (60.0) |
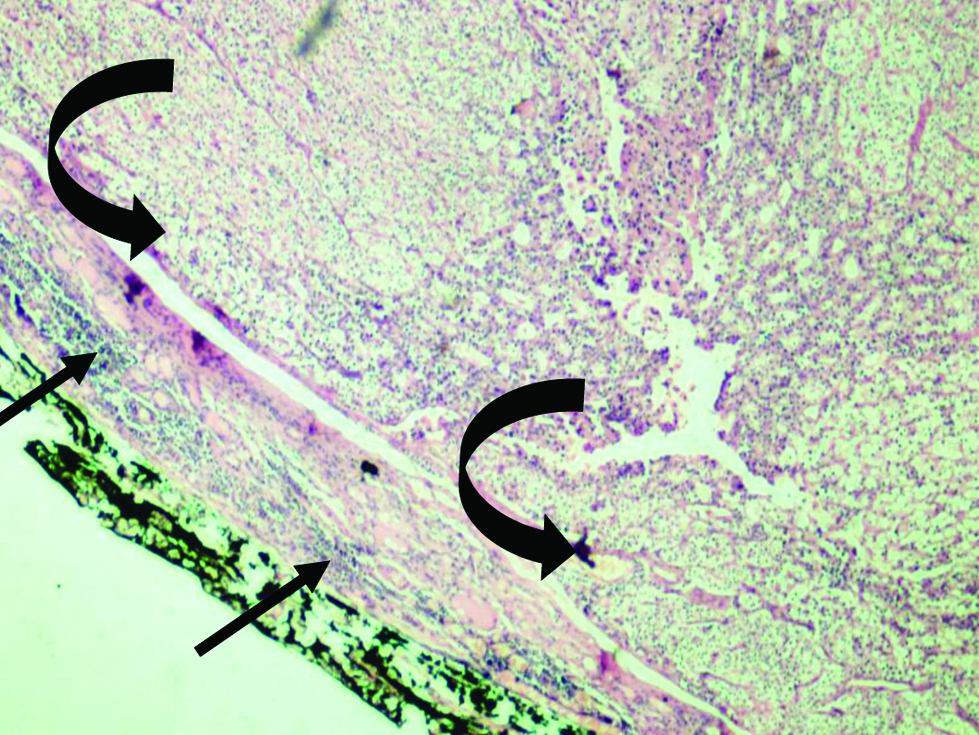
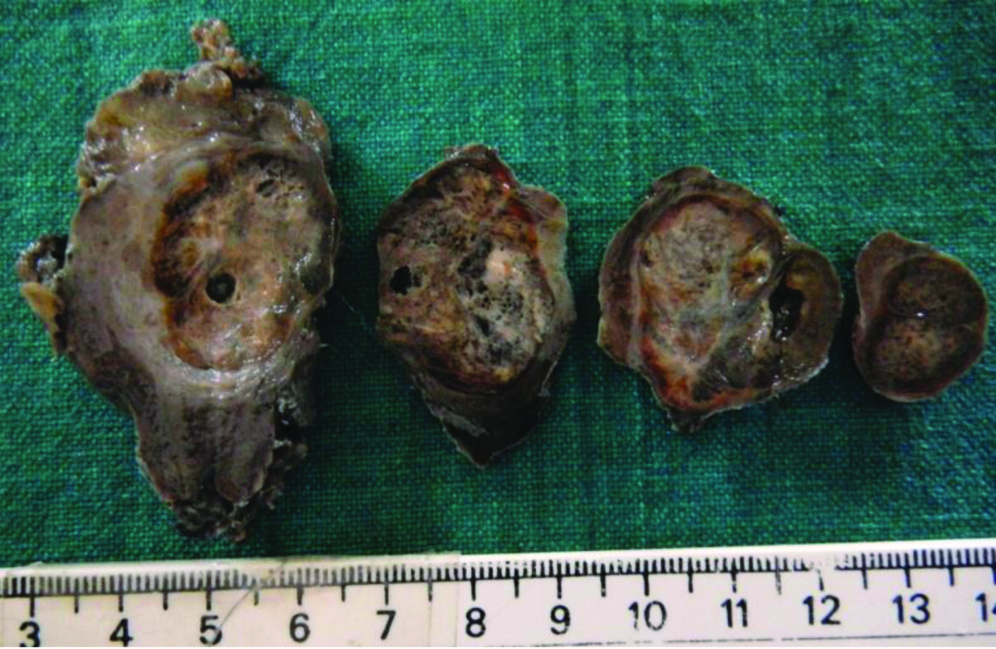
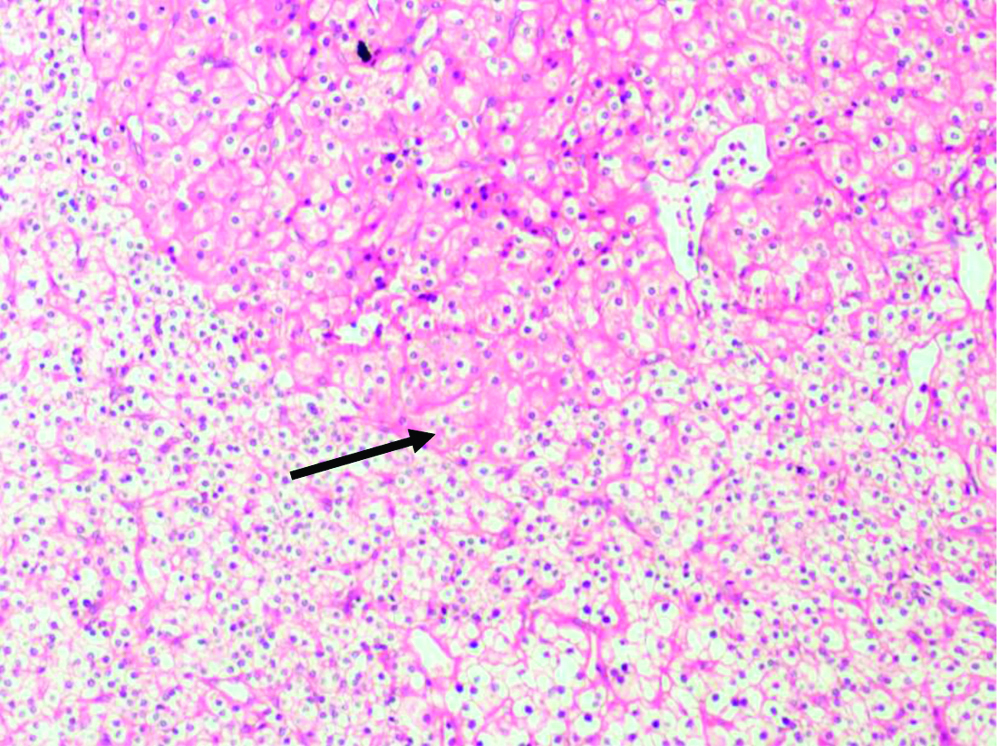
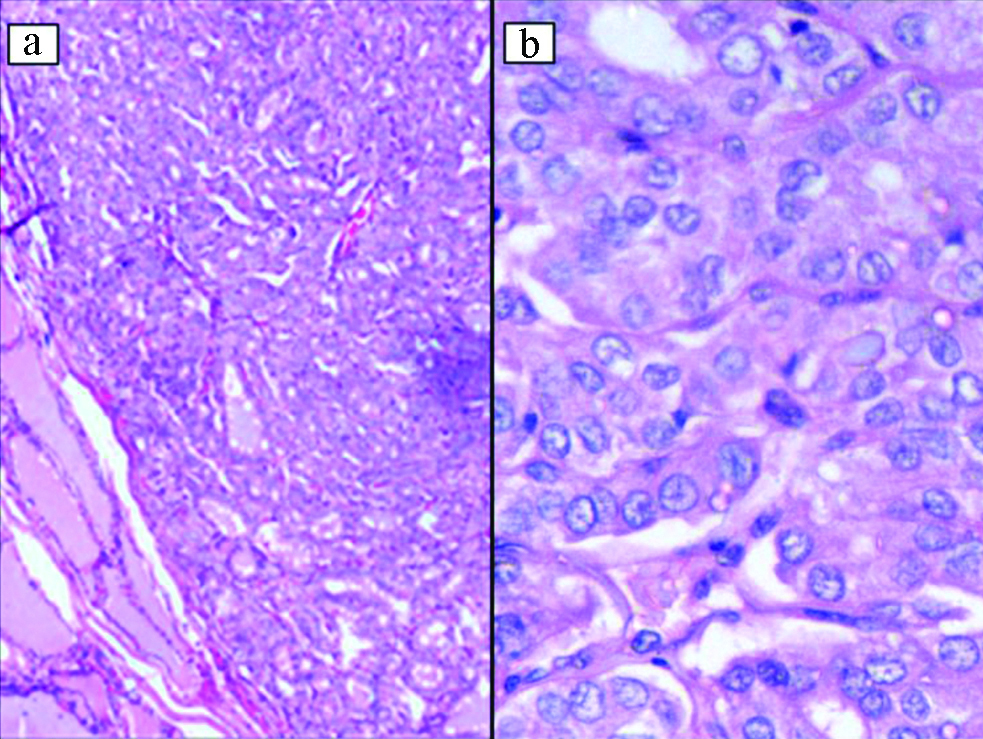
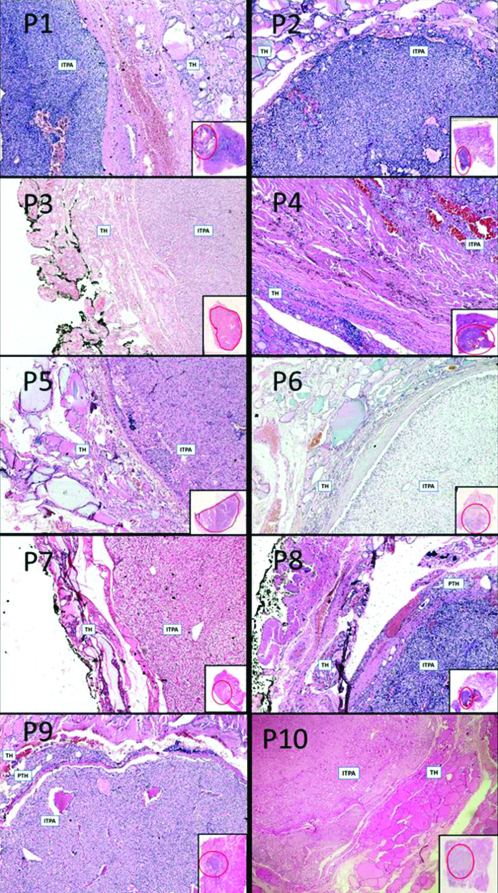
The histopathological features of ITPAs are summarised in [Table/Fig-3]. Four ITPAs (40%) were completely intrathyroidal (c-ITPA) [Table/Fig-4], averaging 1.4±0.4 cm in maximum dimension. Other six (60%) were partially intrathyroidal (p-ITPA), with variable proportions (50-80%) embedded in thyroid, and averaging 2.3 cm±1.1 cm in maximum dimension. Intrathyroid location precluded weighing of the adenomas. The largest p-ITPA (P1) was a cystic parathyroid adenoma. Two large p-ITPAs (P4 and P5) showed variable cystic change, haemorrhage, patchy hyalinisation, thick capsules, and microscopically oxyphil and transitional cells (~20-50%); one of these was diagnosed as Parathyroid adenoma with atypical features (P4) and had a light brown to golden yellow cut surface grossly, suggesting recent and old haemorrhage [Table/Fig-5]. Two p-ITPAs (P5, P6) showed moderate nuclear pleomorphism with occasional bizarre nuclei (endocrine atypia); the latter with a significant proportion of water clear cells (~50%). Two c-ITPAs (P7 and P10) showed few focal oxyphil cells and water clear cells (~5-10%) [Table/Fig-6]. All cases displayed conventional histological features of parathyroid adenomas with chief cells arranged in trabeculae and cords and interspersed delicate vasculature. Definitive features of malignancy were absent. Immunohistochemistry was not necessary for diagnosis in any case. Four cases (40%) had concomitant thyroid disease, including a papillary micro-carcinoma (10%) [Table/Fig-7]; three occurring in p-ITPA patients; and one in a c-ITPA patient. Hashimoto’s thyroiditis was the most frequent diagnosis, occurring in two patients (50%). There were no statistically significant differences between patients with c-ITPAs and p-ITPAs, with respect to age, gender, presence of neck swelling, biochemistry parameters, maximum size and concomitant thyroid disease [Table/Fig-8]. Histopathological images of all ten cases are represented in [Table/Fig-9].
| Pat. no. | Size (cm) | Site | Contour | Cut surface | Capsule | Cells |
|---|
| P1 | 4 | RI | Lobulated | Firm-Cystic Tan-brown | Thick | Chief cells |
| P2 | 1.2 | RS | Circumscribed | Firm, Grey- Tan | Thin | Chief cells |
| P3 | 2 | LI | Lobulated | Firm, Grey | Thin | Chief cells |
| P4 | 2.8 | RI | Irregularly circumscribed | Firm-spongy, light brown- golden yellow | Thick | Chief cells, Oxyphil cells, Transitional cells |
| P5 | 2.9 | RI | Nodular | Soft to firm, Tan to Grey | Thick | Chief cells, Oxyphil cells, Transitional cells |
| P6 | 1 | RI | Lobulated | Firm, Grey | Thin | Chief cells, Clear cells |
| P7 | 1 | LI | Circumscribed | Firm, grey-yellow | Thin | Chief cells with a few oxyphil cells and clear cells |
| P8 | 1.2 | RS | Circumscribed | Firm, tan | Thin | Chief cells |
| P9 | 2 | RI | Circumscribed | Firm, Tan- Yellow | Thin | Chief cells |
| P10 | 1.5 | RI | Circumscribed | Soft to firm, Yellow | Thin | Chief cells with a few oxyphil cells and clear cells |
Grey-shaded Rows- Partial ITPAs, Unshaded rows- Complete ITPAs; RI: Right Inferior, RS: Right Superior, LI: Left Inferior
Case P7- Intrathyroid parathyroid adenoma (curved arrow) with surrounding thyroid parenchyma with focal lymphoid aggregates (thin arrow). (H&E, X40).
Case P4- Gross picture of thyroid specimen showing a circumscribed nodule with light brown to golden yellow spongy cut surface. There is a rim of grey white thick fibrous capsule surrounding the nodule.
Case P7- Clear cells and oxyphil cells (arrow) (H&E, X100).
Case P5- Papillary micro-carcinoma with classic nuclear features such as nuclear enlargement, crowding, overlap, chromatin clearing, and frequent grooves. (a) H&E, X100, b) H&E, X400).
Statistical analysis comparing ITPA groups.
| Variables | Group | p-value |
|---|
| pITPA N (%)/Mean±SD, Median (IQR) | cITPA N (%)/Mean±SD, Median (IQR) |
|---|
| Age (yr) | 42.8±8.3546.5 (35.5, 48.5) | 46.0±15.1745.5 (32.0, 60.5) | 0.678* |
| Gender |
| Male | 2 (33.3) | 1 (25.0) | 1.000# |
| Female | 4 (66.7) | 3 (75.0) |
| Neck swelling |
| Present | 3 (50.0) | 1 (25.0) | 0.571# |
| Absent | 3 (50.0) | 3 (75.0) |
| Maximum size (cm) | 2.30±1.15 cm2.35 (1.15, 3.17) | 1.42±0.43 cm1.35 (1.05, 1.87) | 0.189* |
| Biochemistry parameters |
| Sr. Calcium (mg/dL) | 12.07±0.9312.20 (11.10, 12.90) | 11.52±1.2011.25 (10.55, 12.77) | 0.443* |
| Sr. PTH (pg/mL) | 810.72±598.15650.80 (318.95, 1249.67) | 329.02±218.28280.65 (149.15, 557.27) | 0.171$ |
| Sr. Phosphorus (mg/dL) | 2.08±1.001.80 (1.45, 2.85) | 2.52±0.692.45 (1.90, 3.22) | 0.475* |
| Thyroid disease |
| Present | 3 (50.0) | 1 (25.0) | 0.571# |
| Absent | 3 (50.0) | 3 (75.0) |
#Fisher-exact test; *Independent t-test; $Mann-Whitney U test
All ten cases of ITPA (illustrated with Case numbers on top left).
Cases P1-P10 (H&E, X40 with inset panoramic view highlighting the ITPA position within red circle)
TH: Thyroid; ITPA: Intrathyroid parathyroid adenoma; PTH: Normal Parathyroid
Preoperative ultrasound correctly anticipated eight patients (80%) to have parathyroid adenomas but intrathyroid location was suspected in only four (40%; P3, P5, P8, P10). Concomitant thyroid pathology was suggested appropriately in two (P5, P7) of three cases. Intraoperatively, ITPAs were recognised correctly in eight instances (80%). Radiological, intraoperative and histopathology reports were compiled together [Table/Fig-10]. Combined imaging, intraoperative and histopathological analysis verified eight ITPAs (80%) to be ectopic inferior parathyroids (Right-6, Left-2). The other two were right superior parathyroids (20%). Mean follow-up duration was 23 months, with three defaulters (P4, P5 and P9). All other patients were asymptomatic and eucalcaemic at their last visit.
Radiology intra-operative and pathology findings.
| No. | Ultrasound Impression | Thyroid disease | MIBI | Intra-Op findings | Final pathology impression |
|---|
| P1 | S/o Cystic right inferior Parathyroid adenoma | Not suspected | RI | Right inferior ITPA. RS-WNL. | Right inferior p-ITPA, Hashimoto thyroiditis |
| P2 | S/o Right superior Parathyroid adenoma | No | RS | Right superior ITPA | Right superior p-ITPA |
| P3 | Left thyroid lobe lower pole embedded ectopic PA (ITPA) and Lower pole TR3 lesion (6 mm) | Yes | LI | Left lobe ITPA | Left lobe p-ITPA (LI). Thyroid – No lesion. |
| P4 | Right thyroid lobe 2.8 cm nodule | Not known | RI | Right lobe ITPA | Right lobe p-ITPA (RI), Hashimoto thyroiditis |
| P5 | Right thyroid- solid cystic nodule TR 4A; Re-screening- Probable ITPA. One TR3 nodule with hypoechoic halo. Left thyroid- TR2 cystic nodule | Yes | RI | Right inferior ITPA | Right lobe p-ITPA (RI), Papillary micro-carcinoma |
| P6 | Right thyroid lobe hypoechoic lesion- TR 4B | Solitary thyroid nodule suspected | Neg | Right lobe 2 cm nodule, ‘Right inferior PA’. RS normal. | Right lobe p-ITPA (RI); Specimen sent as Right Inferior PA –Thyroid tissue only. |
| P7 | Both thyroid lobes –TR 3 nodules and mild thyroiditis. Two small oval postero-inferior lesions- Probable Parathyroid adenoma | Yes | RI | Thyroiditis, Diffuse enlargement, ‘Right inferior PA’. RS, LS glands normal. | Left Inferior ITPA (LI), Nodular hyperplasia, Mild lymphocytic thyroiditis; Right Inferior PA specimen- Reactive node. |
| P8 | Probable Right thyroid lobe ITPA | No | RS | Right ITPA. RI normal. | Right lobe ITPA (RS) |
| P9 | Hypoechoic lesion posterior to right lobe- Probable Parathyroid adenoma | No | RI | Right ITPA. RS normal. | Right lobe ITPA (RI) |
| P10 | Both thyroid lobes with TR3 and TR2 nodules. Re-screening- Possible right lobe ITPA | Yes | RI | Right ITPA.RS normal. | Right lobe ITPA (RI). Thyroid- No lesion |
ITPA: Intrathyroid parathyroid adenoma; p-ITPA: Partial ITPA; PA: Parathyroid adenoma; RS: Right superior parathyroid; RI: Right inferior parathyroid; LS: Left superior parathyroid; LI: Left inferior parathyroid; TR (TIRADS): Thyroid imaging reporting and data system; Neg: Negative, WNL: Within normal limits. MIBI- Technetium-99m Sestamibi scan
P6, P7- Intraoperative mis-judgement and corresponding histological findings mentioned in italics
Grey-shaded Rows- Partial ITPAs, Unshaded rows- Complete ITPAs
Discussion
Parathyroid adenoma is the most common cause of PHPT in ambulant patients [18,19]. Parathyroid glands originate from endoderm of third and fourth branchial pouches and migrate caudally to neck during embryogenesis, disturbance of which can result in their ectopic locations, including an intrathyroid location [7]. ITPAs are rare with varying incidence rates among parathyroidectomies [8,9,20-23], depending on the stringency of criteria to define intrathyroid location [Table/Fig-11]. This study differs from previous ones in obtaining the proportion of ITPAs among all parathyroid adenomas alone. Ten ITPAs in this series constituted only 2.4% of all parathyroid adenomas diagnosed during the eight-year period, of which four (0.97%) were completely intrathyroidal and other six partially intrathyroidal (1.46%). Most ITPAs (eight) were ectopic inferior parathyroids (80%) and only two (20%) were ectopic superior parathyroid glands.
ITPA rate in comparison with previous studies [8,9,20-23].
| Authors (year) | Cases | ITPAs | Location of ITPAs |
|---|
| C type | P type |
|---|
| Feliciano DV, [20] (1992) | 96 PHPT parathyroidectomies | 3 (3.1%) | 1 (1%) | Superior-1 (25%) Inferior-2 (50%) Unknown-1 (25%) |
| McIntyre RC et al., [21] (1997) | 309 HPT parathyroidectomies | 6 (2.7%) (No category) | Not available |
| Bahar G et al., [22] (2006) | 426 PHPT parathyroidectomies | 6 (1.4%) | - | Superior-2 (33%) Inferior-2 (33%) Unknown-2 (33%) |
| Romanchishen AF and Matveeva ZS [23] (2007) | 119 parathyroid tumour surgeries | 43 (22.6%) (No category) | Not available |
| Goodman A et al., [8] (2011) | 10000 PHPT parathyroidectomies | 72 (0.7%) | 120 (1.2%) | Inferior-85% |
| Mazeh H et al., [9] (2012) | 4868 PHPT parathyroidectomies | 48 (~1%) | - | Superior-25% Inferior-75% |
| Present study (2020) | 409 parathyroid adenomas | 4 (0.97%) | 6 (1.5%) | Superior-2 (20%) Inferior-8 (80%) |
HPT: Hyperparathyroidism; PHPT: Primary hyperparathyroidism; C/P: Complete/Partial ITPAs
The three largest p-ITPAs (>2.5 cm) were associated with neck swellings, concomitant thyroid diseases, and variable cystic change; two of these also showed significant degenerative changes and oxyphil cells. Other smaller p-ITPAs did not show these features. The smallest p-ITPA showed a prominent water-clear cell component. The c-ITPAs were on an average smaller compared to p-ITPAs, without cystic/degenerative changes and only one was associated with concomitant thyroid disease and neck swelling. However, these differences were not statistically significant. The power of the study was 63%, with respect to the maximum size of the adenomas. All ITPAs displayed histopathological features of usual parathyroid adenomas enabling morphological distinction from thyroid follicular adenomas. Oxyphil cells were distinguishable from thyroid Hurthle cells by distinct cell membranes, granular chromatin, and indistinct nucleoli. Two large p-ITPAs, one (P5), clinically suspected as parathyroid carcinoma and another (P4) diagnosed as parathyroid adenoma with atypical features of focal small cell clusters within capsule, also showed usual histomorphology (including degenerative features). Lack of conclusive invasive growth and other features such as readily identifiable mitoses, tumour necrosis, sheeting pattern with small cells, diffuse atypia and macronucleoli excluded malignancy in both instances [24,25]. Some immunostains such as Ki-67, Parafibromin, Galectin-3, p27 and Cyclin D1 are suggested to be helpful in distinguishing parathyroid adenoma and carcinoma [24,25]. However, these were not required in any case. Parathormone immunohistochemistry was also not required, as all patients were biochemically cured following surgery, confirming the diagnosis of parathyroid adenoma.
Concomitant thyroid disease is quoted to occur in 20-50% of cases of PHPT, of which malignancies constitute 3-4% [26]. Some studies [27,28] however report higher rates. The commonest thyroid pathology reported in most studies [27-30] is nodular hyperplasia [Table/Fig-12]. In contrast, Hashimoto’s thyroiditis occurred most frequently in this series, in 50% of patients with dual pathology. The lone malignancy (papillary micro-carcinoma) occurred in the patient suspected to have parathyroid carcinoma with severe hypercalcaemia. Hypercalcaemia is thought as a reason for increase in certain malignancies, including thyroid cancers, in PHPT [27,31]. A recent study found association between high parathormone levels and papillary carcinoma in symptomatic PHPT patients [32]. There was no history of cervical irradiation in this patient which is a common risk factor for parathyroid adenoma and papillary thyroid carcinoma [27].
Concomitant thyroid pathologies in comparison with previous studies [27-30].
| Authors (Year) | Total cases | Dual pathology/all cases | Malignancy/all cases | Commonest thyroid pathology/all dual pathologies |
|---|
| Livolsi VA and Feind CR [27] (1976) | 272 parathyroid adenomas with thyroid resection | 168 (61.7%) | 31 (11.4%) | Nodular goiter-64% (n=108) |
| Beus KS and Stack BC [28] (2004) | 101 parathyroidectomies | 17 (17%) | 3 (2.9%) | Nodular hyperplasia-41% (n=7) |
| Kösem M et al., [29] (2004) | 51 PHPT neck explorations | 43 (84.3%) | 9 (17.6%) | Nodular hyperplasia-56% (n=24) |
| Ryan S et al., [30] (2015) | 135 parathyroidectomies | 36 (27%) | 5 (3.7%) | Multinodular goitre-50% (n=18) |
| Present study (2020) | 10 ITPAs | 4 (40%) | 1 (10%) | Hashimoto thyroiditis- 50% (n=2) |
Ultrasound correctly predicted parathyroid adenoma in eight cases (~80%), similar to high diagnostic rates documented in literature [16,33]. Intrathyroid localisation was however possible in only four (P3, P5, P8, P10) resulting in a preoperative diagnostic rate of 40% for ITPAs, unlike high rates reported in a few studies [10,11]. Initially, four ITPAs were mis-interpreted as thyroid nodules, which can happen [14,15]. However, the clinical profile and Sestamibi findings, prompted re-assessment by a specialist radiologist in two patients, resulting in suspicion of ITPA. Ultrasound also identified concomitant thyroid pathology in two of three cases. In one patient (P1) however, Hashimoto’s thyroiditis (confirmed by histopathology), was not identified. The referred patient with Hashimoto’s thyroiditis (P4) did not have complete imaging details for a comment on thyroid assessment.
Intraoperatively, ITPAs were correctly identified in eight patients (Diagnostic rate: 80%), five of whom (including 3 c-ITPAs), had no concomitant thyroid disease. In three other patients who also had thyroid disease, the ITPAs were relatively larger and only partially intrathyroid, possibly enabling their identification during surgery. In the two smallest ITPAs (P6, P7), one with concomitant nodular thyroid disease and another diagnosed as a ‘TIRADS-4 thyroid nodule’ by ultrasound, the collective imaging inputs (including 4D-CT scan in P6) resulted in intraoperative misjudgement of benign thyroid tissue and a reactive lymph node for ‘parathyroid adenomas’, as confirmed subsequently by histopathology. However, simultaneous thyroidectomy done to assess the thyroid enabled their identification by histopathology. The lower sensitivity of preoperative imaging studies in small parathyroid adenomas and in patients with concomitant thyroid disease is known [17]. An enlarged nodular thyroid attenuates sound, and thereby lowers sonological sensitivity [16]. Sestamibi scans also show non-specific uptake in thyroid nodules or are falsely negative in small adenomas [34]. Intraoperative assessment can also be equally challenging in such situations. Considering standard histomorphological appearances of ITPAs, frozen section examination of the thyroid lobe with suspicious nodule(s) may be useful in such scenarios, apart from intraoperative parathormone assessment.
Limitation(s)
The major limitation of this study was the small number of cases, affecting comparison of the two ITPA categories for various clinical or pathological parameters.
Conclusion(s)
ITPAs are rare and can be misinterpreted as thyroid nodules during preoperative imaging, especially with concomitant thyroid disease and in small adenomas. An experienced radiologist re-assessment for this entity when initial preoperative localisation fails may be helpful in such instances. Any suspicious thyroid nodule detected during imaging must affect the extent of surgery, to enable histopathological identification of possible ITPA and/or concomitant thyroid disease including incidental malignancies. In the appropriate clinical setting of PHPT, immunohistochemistry is not routinely necessary for histopathological diagnosis of ITPAs. To the best of our knowledge, this is the first article from India reporting the common clinico-pathological features of these rare tumours.
R: Renal disease; M: Musculoskeletal symptoms; P: Pancreatitis; N: Neck swelling
Grey-shaded Rows- Partial ITPAs, Unshaded rows- Complete ITPAs
*Patient (specimen) referred from another hospital
$Clinically suspected as parathyroid carcinoma
#Patient with neck swelling and osteopenia detected by DEXA scan
Ca2+- Serum calcium (corrected for albumin), PO42- Serum Phosphorus, PTH-Serum Parathormone levels
Grey-shaded Rows- Partial ITPAs, Unshaded rows- Complete ITPAs; RI: Right Inferior, RS: Right Superior, LI: Left Inferior
#Fisher-exact test; *Independent t-test; $Mann-Whitney U test
ITPA: Intrathyroid parathyroid adenoma; p-ITPA: Partial ITPA; PA: Parathyroid adenoma; RS: Right superior parathyroid; RI: Right inferior parathyroid; LS: Left superior parathyroid; LI: Left inferior parathyroid; TR (TIRADS): Thyroid imaging reporting and data system; Neg: Negative, WNL: Within normal limits. MIBI- Technetium-99m Sestamibi scan
P6, P7- Intraoperative mis-judgement and corresponding histological findings mentioned in italics
Grey-shaded Rows- Partial ITPAs, Unshaded rows- Complete ITPAs
HPT: Hyperparathyroidism; PHPT: Primary hyperparathyroidism; C/P: Complete/Partial ITPAs