Spirometry Function after Decortication for Chronic Pleural Empyema: A Retrospective Study
Subhash Minda1, Lata Khatnani Koneru2, Nimish Rai3
1 Assistant Professor, Department of Cardiothoracic and Vascular Surgery, Superspeciality Hospital, NSCB Medical College, Jabalpur, Madhya Pradesh, India.
2 Assistant Professor, Department of Cardiothoracic and Vascular Surgery, Superspeciality Hospital, NSCB Medical College, Jabalpur, Madhya Pradesh, India.
3 Associate Professor, Department of Cardiothoracic and Vascular Surgery, Superspeciality Hospital, NSCB Medical College, Jabalpur, Madhya Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Lata Khatnani Koneru, D Block, House No. 416, Swastik Grand Apartment, Dhanvantri Nagar, Jabalpur, Madhya Pradesh, India.
E-mail: Drlatak84@gmail.com
Introduction
Chronic Pleural Empyema (CPE) is a major medical concern. It gives rise to “trapped lung” due to the thickened pleural peel. This results in impairment of pulmonary function. The treatment of choice for CPE is open thoracotomy decortication.
Aim
To evaluate changes in Pulmonary Function Test (PFT) in an immediate postoperative period of decortication for CPE.
Materials and Methods
A retrospective study was conducted in 25 patients who had undergone decortication for CPE in the last one year (from October 2018 to September 2019) were included. Baseline clinical and demographic data were collected. Duration of ICU stay, hospital stay and complications were reviewed. In Preoperative period Forced Vital Capacity (FVC) and Forced Expiratory Volume In First Second (FEV1) was investigated. It was again repeated after 3 and 6 months of postoperative period. Preoperative and postoperative data at 3rd and 6th month were analysed. Percentage change in PFT was assessed. Repeated measure ANOVA were used for statistical analysis.
Results
Preoperatively the mean FVC was 2.09 L (56.63%) and the mean FEV1 was 1.82 L (60.26%). The mean FVC, 3 months after surgery was 2.27 L (61.52%) and after 6 months was 2.53 L (68.56%). The mean FEV1, 3 months after surgery was 1.92 L (63.58%) and after 6 months was 2.17 L (71.58%). Spirometry values of FEV1 and FVC improved at 3rd and 6th month, postoperatively. Improvement in these Spirometric values after 6 months was quantified statistically significant.
Conclusion
Decortication for CPE resulted in progressive improvement in spirometry values in a follow-up period of 3 and 6 months.
Forced expiratory volume, Lung diseases, Pulmonary function test, Thoracotomy, Tuberculous/surgery, Vital capacity
Introduction
Empyema thoracis is purulent pleural effusion. Most empyemas result from bacterial suppuration of the lungs. Most of the empyemas are associated with bronchiectasis, pulmonary abscess and suppurative pneumonia [1]. Predisposing factors for post pneumonic empyemas are alcoholism, chronic pulmonary disease, inactive pulmonary tuberculosis, diabetes mellitus, long-term steroid therapy and various malignancies. In our country, most of the patients with CPE are attributed to tuberculosis [2].
The American thoracic society has divided progression into 3 distinct stages: exudative, fibrinopurulent and organisation stage. Since many cases of empyema are indolent, the most common presentation is fibrinopurulent or organised stage [3]. In the chronic stage, lung is imprisoned within a thick fibrous peel. The lung is now virtually functionless.
Management strategies depend upon the stage of empyema presentation. Various methods of management, i.e., drainage, antibiotics, intrapleural enzymes and talc, rib resection drainage and open thoracic window, space sterilisation, decortication etc. are available. Video Assisted Thoracoscopic Surgery (VATS) is a common procedure in early stages of fibrinopurulent states [4]. However, in chronic empyema VATS decortication were mostly converted to open decortication [5]. For advanced stages of empyema, open thoracotomy decortication is the treatment of choice [6]. The success rate of decortication depends on intact visceral pleura and space obliteration by pulmonary re-expansion. The outcome of thoracotomy and decortication is better with a success rate of up to 95%, but it has few complications [7]. Retrospective cohort study by Sokouti M et al., has shown that success rates between surgical and nonsurgical treatments were 98.2% and 27.1% and the differences between them was significant (p<0.001) [8]. Advancement in modern antibiotics and preoperative care has made the morbidity and mortality associated with the procedure almost negligible. The aim of this study was to evaluate changes in PFT in an immediate postoperative period of decortication for CPE.
Materials and Methods
This retrospective observational study was conducted in a tertiary level hospital attached to medical college. The study included 25 patients suffering from chronic empyema. The sample size was calculated by using Kelsey JL et al., method, keeping 95% CI and 80% power [8,9]. Age range of these patients was 16-55 years. They were treated with decortication via open thoracotomy at our Thoracic and Vascular Department between October 2018 to September 2019. They were followed after 3 and 6 months, respectively. Chronic empyema due to both tubercular and nontubercular aetiology was included in the study. Trauma and malignancy as an antecedent cause of empyema were excluded from the study. Procedures followed were in accordance with the ethical standards adhered with the Helsinki Declaration and its amendments.
Diagnosis of CPE was established by using chest X-ray, CT lung, USG of lung and pleura and diagnostic thoracocentesis. Preoperatively, FVC and FEV1 were investigated. In all, 25 patients, after establishing diagnosis, thoracotomy with decortication was performed. Most frequently posterolateral thoracotomy was done. The surgery was done under general anaesthesia with single lung ventilation. Affected parietal and visceral pleura were resected and trapped part of the lung was released. Any pathological process in trapped part of the lung (abscess or fibrosis with infection) was dealt with atypical lung resection in healthy tissue. Two drains were put in thoracic cavity at the end of surgery. During ICU stay, any complication (post-op bleeding, air leak, atelectasis, respiratory failure, bronchopleural fistula) was noted. Total ICU and hospital stay was noted. PFT were repeated at 3rd and 6th month of the postoperative period.
Statistical Analysis
Statistical analysis was done with SPSS software version 21. Comparison of preoperative and postoperative value of FEV1 and FVC was done by repeated measures ANOVA. While comparison between tubercular and nontubercular group was done by Mann-Whitney U test. All analysis were two tailed, p-value <0.05 was considered as statistically significant. Confidence interval was set at 95%.
Results
The patients’ age ranged from 16-55 years, with a mean age of 33.68±12.11 years. There were 5 patients (20%) who were smokers, 2 (8%) had diabetes and 18 (72%) patients had tuberculosis [Table/Fig-1].
Baseline clinical parameters of study participants.
| Parameters | Frequency |
|---|
| Age (years) | 33.68±12.11 (16-55) |
| Sex |
| Male | 18 (72%) |
| Female | 7 (28%) |
| Side |
| Right | 13 (52%) |
| Left | 12 (48%) |
| Symptoms |
| Cough | 16 (64%) |
| Shortness of breath | 15 (60%) |
| Fever | 11 (44%) |
| Chest pain | 6 (24%) |
| Haemoptysis | 4 (16%) |
| Weight loss | 7 (28%) |
| Recurrent pleural effusion | 4 (16%) |
| Comorbidities |
| Diabetes | 2 (8%) |
| Pulmonary tuberculosis | 18 (72%) |
| Smoking | 5 (20%) |
| FVC (before surgery) L | 2.09±0.84 |
| FEV1 (before surgery) L | 1.83±0.70 |
| Duration of ICU stay (days) | 2.72 ±0.54 |
| Duration of hospital stay (days) | 9.12±3.56 |
| Complications |
| Air leak | 2/25 (8%) |
| Atelectasis | 2/25 (8%) |
| Wound infection | 1/25 (4%) |
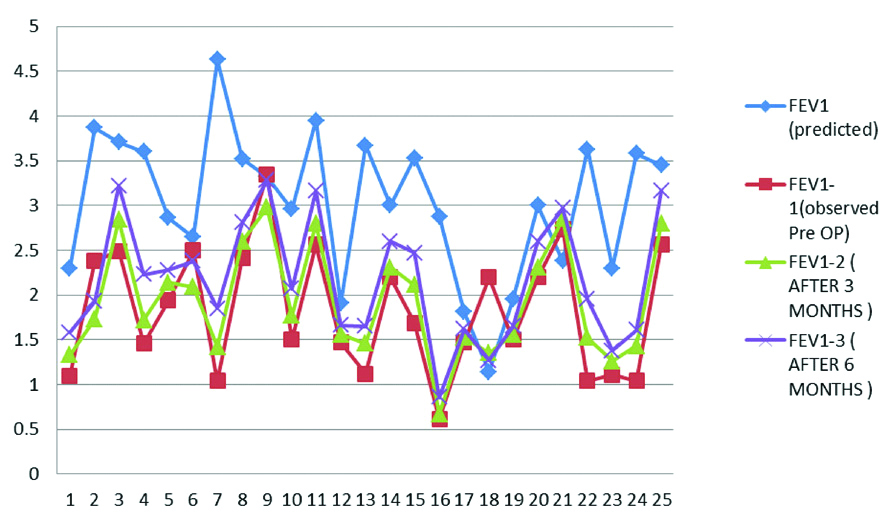
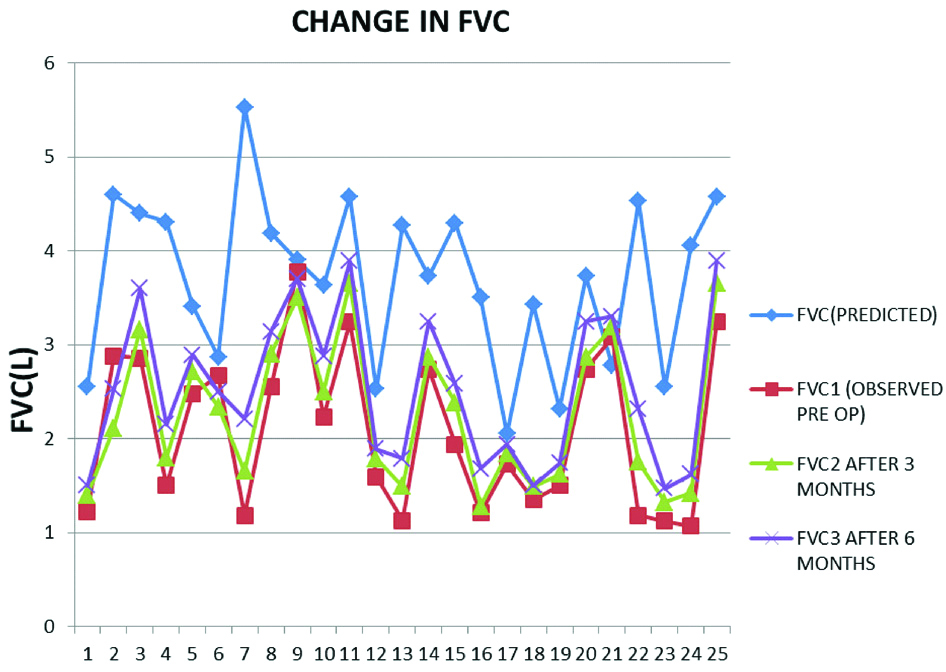
Parameters of PFT, i.e., Forced FEV1 and FVC are presented in [Table/Fig-2,3]. The FVC was increased by 4.8% and 11.93% at 3rd and 6th month in postoperative period respectively while the FEV1 was increased by 3.32% and 11.32% at 3rd and 6th month of the postoperative period, respectively [Table/Fig-4].
Distribution showing alteration in Forced Expiratory Volume In 1 Second (FEV1) in patients with pleural empyema treated with decortication. FEV1- (predicted), FEV1-1 (Observed preoperative), FEV1-2 (after 3 months), FEV1-3 (after 6 month).
Distribution of Forced vital capacity (FVC) in patients with pleural empyema treated with decortication. FVC (Predicted), FVC1 (observed preoperative), FVC2 (after 3 months), FVC3 (after 6 months).
Changes in PFT preoperatively and postoperatively.
| Predicted | Before surgery | After 3 month of surgery | After 6 month of surgery |
|---|
| FVC (L) | 3.69±0.88100% | 2.09 ±0.8456.63% | 2.27±0.7861.52% | 2.53 ±0.8068.56% |
| FEV1 (L) | 3.02±0.81100% | 1.82 ±0.7060.26% | 1.92 ±0.6263.58% | 2.17 ±0.68 71.58% |
(FVC- forced vital capacity and FEV1 – forced expiratory volume in 1s)
Comparison over time by repeated measure ANOVA showed that spirometry variables (FVC and FEV1) after 6 months were significantly raised in comparison to pre op values (p=0.001). The difference between postoperative values of FVC and FEV1 at 3rd and 6th month was also significant (p=<0.001, p<0.001). However, improvement in FEV1 within 3 months was not significant (p=0.45) [Table/Fig-5,6]. On comparing between tubercular and nontubercular group, median percentage improvement in FEV1 at 6 months were 23% and 10%, respectively (p= 0.14). Similarly, in FVC, median percentage improvement between tubercular and nontubercular group at 6 months were 23% and 12%, respectively (p=0.14).
Comparison of preoperative and postoperative value of Forced Vital Capacity (FVC) by repeated measures ANOVA.
| Mean diff | Std error | p-value | 95% CI of diff |
|---|
| FVC1 vs FVC2 | -0.18 | 0.06 | 0.01 | -0.32 to -0.033 |
| FVC1 vs FVC3 | -0.440 | 0.07 | 0.001 | -0.61 to-0.26 |
| FVC2 vs FVC3 | -0.260 | 0.03 | 0.001 | -0.34 to -0.18 |
FVC1 (observed preoperative), FVC2 (after 3 months), FVC3 (after 6 months)
Comparison of preoperative and postoperative value of Forced Expiratory Volume In 1 Second (FEV1) by repeated measures ANOVA.
| Mean diff | Std error | p-value | 95% CI |
|---|
| FEV1-1 vs FEV1-2 | -0.09 | 0.07 | 0.45 | -0.27 to 0.07 |
| FEV1-1 vs FEV1-3 | -0.34 | 0.08 | 0.001 | -0.56 to -0.13 |
| FEV1-2 vs FEV1-3 | -0.24 | 0.03 | 0.001 | -0.31to -0.17 |
FEV1-1 (Observed preoperative), FEV1-2 (after 3 months), FEV1-3 (after 6 months)
Discussion
In CPE both visceral and parietal pleura become thick and fibrotic. This leads to advanced inflammation of lung surface, diaphragm and endothoracic fascia. It results in a significant decrease in pulmonary function [10]. Ventilation, perfusion and oxygen uptake are disturbed. Physiological studies have established that it can be recovered with re-expansion of lung [11]. Decortication helps in improving pulmonary function by freeing the trapped lung, obliterating the pleural space and by regaining mobility of chest wall and diaphragm. The improvement in lung function is usually significant after 6 months of the operation, when the pain has dispersed [12]. Many studies have assessed the impact of decortication on pulmonary function. However, the extent to which pulmonary function is restored varies in different studies [12-14]. Most studies have had significant increase in FVC and FEV1 [12-19]. In a study of 35 patients with 60% tubercular aetiology, Abraham SV et al., had shown that after decortication, spirometric parameters FEV1 and FVC were improved by approximately 14% and 17%, respectively [16]. This improvement was seen in a period of 6 months. Bagheri R et al., had studied 50 patients with 20% tubercular aetiology [15]. After decortication FEV1 and FVC was improved by 14.8% and 17.9%, respectively in a span of one year. In a study of 63 patients with 57% tubercular aetiology, Gorur R et al., had found significant improvement in postoperative period of 6 months in both variables FEV1 & FVC(4.2%, 5.4%) [13]. Choi SS et al., has compared postoperative PFT improvement in 41 tuberculous and 24 nontuberculous patients with empyema [14]. They found a mean increase of 15% in FVC and 10% in FEV1 in tuberculous group, while in nontuberculous group, there was increment of 7% both in FVC and FEV1. In our study, both parameters FVC and FEV1 were significantly improved at the period of 6 months (p=<0.001, p=0.001). We have found that improvement in FEV1 after 3 months of surgery was not significant p=0.45. It could be due to the pain associated with thoracotomy. However, some studies have contradictory findings. Petro W et al., and Toomes H et al., have shown that spirometric parameters after decortication do not improve when tuberculosis and destructive pulmonary diseases are predominant aetiological factors [20,21]. Spirometry itself is effort related task and ineffective effort may give false values. However, all our patients were being operated by single surgical team with single technique i.e., decortication via thoracotomy. It was an advantage of our study.
Limitation(s)
The limitation of this study is a relatively low sample size, the retrospective nature and use of only FVC and FEV1 as measures of pulmonary function.
Conclusion(s)
Decortication via open thoracotomy adequately restores the pulmonary function. The majority of our patients were of tubercular aetiology. Improvement was seen in both tubercular and nontubercular patients. Significant recovery in spirometry parameters (FVC and FEV1) were seen after 6 months of surgery.
(FVC- forced vital capacity and FEV1 – forced expiratory volume in 1s)
FVC1 (observed preoperative), FVC2 (after 3 months), FVC3 (after 6 months)
FEV1-1 (Observed preoperative), FEV1-2 (after 3 months), FEV1-3 (after 6 months)
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 01, 2020
Manual Googling: Jun 27, 2020
iThenticate Software: Jul 24, 2020 (14%)
[1]. Light RW, Parapneumonic effusions and empyemaProc Am Thorac Soc 2006 3(1):75-80.10.1513/pats.200510-113JH16493154 [Google Scholar] [CrossRef] [PubMed]
[2]. Cameron RJ, Management of complicated parapneumonic effusions and thoracic empyemaIntern Med J 2002 32(8):408-14.10.1046/j.1445-5994.2002.00252.x12162398 [Google Scholar] [CrossRef] [PubMed]
[3]. Renner H, Gabor S, Pinter H, Maier A, Friehs G, Smolle-Juettner FM, Is aggressive surgery in pleural empyema justified?Eur J Cardiothorac Surg 1998 14(2):117-22.10.1016/S1010-7940(98)00165-1 [Google Scholar] [CrossRef]
[4]. Ferrer J, Roldán J, Clinical management of the patient with pleural effusionEur J Radiol 2000 34(2):76-86.10.1016/S0720-048X(00)00166-2 [Google Scholar] [CrossRef]
[5]. Scarci M, Abah U, Solli P, Page A, Waller D, van Schil P, EACTS expert consensus statement for surgical management of pleural empyemaEur J Cardiothorac Surg 2015 48(5):642-53.10.1093/ejcts/ezv27226254467 [Google Scholar] [CrossRef] [PubMed]
[6]. Molnar TF, Current surgical treatment of thoracic empyema in adultsEur J Cardiothorac Surg 2007 32(3):422-30.10.1016/j.ejcts.2007.05.02817646107 [Google Scholar] [CrossRef] [PubMed]
[7]. Melloni G, Carretta A, Ciriaco P, Negri G, Voci C, Augello G, Decortication for chronic parapneumonic empyema: Results of a prospective studyWorld J Surg 2004 28(5):488-93.10.1007/s00268-004-7213-y15085395 [Google Scholar] [CrossRef] [PubMed]
[8]. Sokouti M, Ghojazadeh M, Sokouti M, Sokouti B, Surgical and nonsurgical outcomes for treating a cohort of empyema thoracis patients: A monocenteric retrospective cohort studyAnn Med Surg (Lond) 2017 24:19-24.Published 2017 Oct 13. doi:10.1016/j.amsu.2017.10.0010.1016/j.amsu.2017.10.00229062481 [Google Scholar] [CrossRef] [PubMed]
[9]. Kelsey JL, Whittemore AS, Evans AS, Thompson WD, Methods in observational epidemiologyMonographs in Epidemiology and Biostatistics 1996 [Google Scholar]
[10]. Thourani VH, Brady KM, Mansour K, Miller JI, Lee RB, Evaluation of treatment modalities for thoracic empyema: Cost effective analysisAnn Thoracic Surg 1998 66:1121-27.10.1016/S0003-4975(98)00767-X [Google Scholar] [CrossRef]
[11]. Morton JR, Boushy SF, Guinn GA, Physiological evaluation of results of pulmonary decorticationAnn Thorac Surg 1970 9(4):321-26.10.1016/S0003-4975(10)65513-0 [Google Scholar] [CrossRef]
[12]. Gokce M, Okur E, Baysungur V, Ergene G, Sevilgen G, Halezeroglu S, Lung decortication for chronic empyaema: Effects on pulmonary function and thoracic asymmetry in the late periodEur J Cardiothorac Surg 2009 36(4):754-58.10.1016/j.ejcts.2009.04.04319535260 [Google Scholar] [CrossRef] [PubMed]
[13]. Gorur R, Yildizhan A, Yiyit N, Kutlu A, Sonmez G, Isitmangil T, Spirometric changes after pleural decortication in young adultsANZ J Surg 2007 77(5):344-46.10.1111/j.1445-2197.2007.04056.x17497972 [Google Scholar] [CrossRef] [PubMed]
[14]. Choi SS, Kim DJ, Kim KD, Chung KY, Change in pulmonary function following empyemectomy and decortication in tuberculous and non-tuberculous chronic empyemathoracisYonsei Med J 2004 45(4):643-48.10.3349/ymj.2004.45.4.64315344205 [Google Scholar] [CrossRef] [PubMed]
[15]. Bagheri R, Haghi SZ, Dalouee MN, Rajabnejad A, Basiri R, Hajian T, Effect of decortication and pleurectomy in chronic empyema patientsAsian Cardiovasc Thorac Ann 2016 24(3):245-49.10.1177/021849231662928126787536 [Google Scholar] [CrossRef] [PubMed]
[16]. Abraham SV, Chikkahonnaiah P, Change in pulmonary function following decortication for chronic pleural empyemaTurk Thorac J 2020 21(1):27-31.10.5152/TurkThoracJ.2019.18014632163360 [Google Scholar] [CrossRef] [PubMed]
[17]. Rzyman W, Skokowski J, Romanowicz G, Lass P, Dziadziuszko R, Decortication in chronic pleural empyema- Effect on lung functionEur J Cardiothorac Surg 2002 21(3):502-07.10.1016/S1010-7940(01)01167-8 [Google Scholar] [CrossRef]
[18]. Rai SP, Kaul SK, Tripathi RK, Bhattacharya D, Kashyap M, Decortication in chronic pleural empyemaLung India 2006 23:100-02.10.4103/0970-2113.44399 [Google Scholar] [CrossRef]
[19]. Özer KB, Tükel M, Özdemir A, Cesur EE, Demirhan R, The effects of pleural decortication on respiratory functions of the patients withpleural empyemaSouth Clin Ist Euras 2018 29(2):99-104.10.14744/scie.2018.85866 [Google Scholar] [CrossRef]
[20]. Petro W, Maassen W, Greschuchna D, Steinberg U, Konietzko N, Regional and global lung function in unilateral fibrothorax after conservative therapy and decorticationThorac Cardiovasc Surg 1982 30(3):137-41.10.1055/s-2007-10222316180506 [Google Scholar] [CrossRef] [PubMed]
[21]. Toomes H, Vogt-Moykopf I, Ahrendt J, Decortication of the lungThorac Cardiovasc Surg 1983 31(6):338-41.10.1055/s-2007-10220146198752 [Google Scholar] [CrossRef] [PubMed]