Introduction
The financing part is an important aspect of a program to be implemented with a certain degree of success. Financial commitment of any government is considered as the highest form of commitment for successful outcomes. Without sufficient fiscal provision, no program can be transformed into the desired levels [1-3]. This is equally applicable to the health sector development. Health sector in India has had much less achievement due to poor financing of various healthcare programs and creation of healthcare infrastructure for provision of services [4]. There has not been much fiscal provision in the health sector to transform the situation at ground level by governments over the time. Evidence shows that unequal distribution of healthcare resources and low priority in budgeting for healthcare leads to major challenges in achievement of Universal Health Coverage (UHC) in India [4,5].
In many sectors, India has achieved success in the world and is able to deliver world-class products and services by making committed budgetary provision and stewardship at the highest level [6]. In scientific sectors like space, atomic energy, defence preparedness, aviation, science, and technology, the achievements are landmark developments for India in the global arena [7]. Whereas, in the social sector, there is little evidence of transformation in pilot mode or regional developments by committed financial resources for development of society. In health sector, the achievements are not that great. In terms of healthcare ranking, India trails behind many developing countries due to poor health indicators. Even our neighbours like Bangladesh and Sri Lanka perform better in many aspects [8,9]. The World Health Report in 2010 emphasised on generation of fiscal space to boost healthcare in developing countries [10]. Out of the total health expenditure, which is nearly 5% of total GDP, only 1.2% is public spending through various mechanisms of financing [11]. Whereas, the remaining amount is contributed by individuals, private players and the employers in India. In 2014, the National Health Assurance Mission (NHAM) focused on spending of USD 6.5 billion per year during the period 2014-2019 to achieve UHC in India [11]. This amount is equivalent to 0.28% of the USD 2.25 trillion GDP estimation by the World Bank in 2016 for India, which seems achievable budget for financing the health sector in the country [12,13].
Later on, National Health Policy 2017 regarding UHC promised many things in line with the international discourse on emerging trends of healthcare [14-16]. Contrary to this, the lack of stewardship to energise health system in the country is not found for such an ambitious plan. The government plan gives hope for achievement of the UHC through Prime Ministers’ Jan Arogya Yojna (PMJAY) [17]. The NITI Aayog tries to make accessible health care with strong provisions in various schemes governed by health sector in India. Ever-increasing cost of health care can be arrested by fixing package rates in advance, providing a protocol for treatment and collection of perception of patients regarding services. The PMJAY has no user’s fee collection from patients and is being implemented with the existing healthcare providers and network of state government institutions [6]. Services of private hospital are usually available to rich people having sufficient economic well-being in India. Rich people have better access to private hospitals requiring high cost of treatment. Moreover, they have coverage of insurance schemes [4]. The real challenges like adverse selection, moral hazards, and fraudulent claims happen in such cases. These are causes for increase of prices of private medical services in India [2].
No doubt, money is not the only concern for program implementation in health sector. However, it is a very important component in addition to other components. The human resources, infrastructure, technology and work culture can be enhanced by infusing funds in healthcare system. Overall, projects in health sector need sufficient funds for the development of health systems in any country [4]. Any attempt for progress needs basically a strong political will and highly committed financial resources to accomplish a project [3]. If the project is of a very large scale, then there is a requirement of a massive amount of funding with a very strong mechanism for monitoring and evaluation.
Many a time, some government officials and pseudo-committed leaders argue in favour of bleeding money without provision of basic resources for committed work. However, they should know importance of resources in creating a committed basic structure. Usually, healthcare workforce and capacity development can only be achieved by provision of resources for long period [1]. In other words, to develop doctors, paramedics and technicians for a functional health system, there is a need of a long incubation period. Whereas hard and soft infrastructure can be developed within a shorter period by provision of sufficient resources. There is certain aspect of healthcare can be created or procured with just availability of resources which require very less time. So, the basic requirement of health financing should be provision of sufficient funding for transformation of health care structure [1]. It will be naïve to conclude that financial provision cannot create a good health infrastructure in a short period. Many south-east Asian countries achieved this in miraculous time by infusing resources to their ailing healthcare systems [9]. However, there are very few countries like the United States of America (USA), despite spending about 16% of GDP, the provision of universal health care is not achieved. This may have strength and limitations in their health sector [9]. In Indian context, the under-performance in health sector can be attributed to a lack of commitment of financial resources over last seven decades. That’s why, we are still grappling with Bhore committee recommendations as a standard yet to be achieved in India. Had there been sufficient provision of funding for infrastructural development, the Bhore committee recommendation would have been studied as any historical facts in the textbook or milestone in the policy documents of a nation. Even today, the Bhore committee report is discussed widely in national and international conferences, symposiums and public debates on healthcare. India, as a nation still stuck with the recommendations of the Bhore committee for achievement of primary care and universal health care [15].
Had India spent 6% of the GDP for 4-5 decades, our health infrastructure might have been quite different. By now, healthcare challenges may not be of rudimentary which is very similar to many African nations. This is evident from the fact that the same donor organisations and implementing agencies are working in Africa, Latin America, and India in addition to some South Asian countries like Afghanistan, Pakistan, Myanmar, Vietnam, and Cambodia. In healthcare distresses, India is approaching the international NGOs and the United Nation’s bodies for funds and technical supports for solving many healthcare problems similar to underdeveloped nations on communicable diseases [4,9]. In other words, India is competing for the same resources designated (provided) by OECD countries, philanthropists and the United Nations (UN) agencies for the underdeveloped countries in the world. Despite modern cutting edge technology, India suffers in provision of healthcare due to a lack of sufficient financial resources for the health sector [1]. Though there is a generalised mocking of India by some countries for desperate funding from international agencies and donors, still India have a similar approach in health sector for the fund to run some programs.
Many a time, the burgeoning population of India is squarely blamed for the awful condition of health sector. However, to curb population growth, sufficient provision of resources and awareness is not provided by the governments. Population control needs a very integrated approach that is not done by the governments [4,15]. Whatever may be the scene, currently, the southern states in India are not facing any problem of population growth, which is evident from the replacement level of Total Fertility Rate (TFR). The southern states are either approaching the ideal TFR of replacement level of 2.1 or below that whereas the northern states are affected by high TFR with evidence of a reduction in recent decades [15]. Indirectly, we cannot argue that the healthcare problem in India is not only due to population explosion; rather, the low financing should be blamed for.
Often, Social Determinants in Health (SDH) are argued vehemently for the low output of the healthcare achievement. Evidence also found that SDH factors really need to be addressed. Because healthcare remains out of reach for masses despite provision of standard care in the locality [15]. However, SDH can also be addressed by making awareness in the community and additional investment in related sectors for sufficient reform in community [3]. All these things again need committed resources than mere lip services. Hence, it is argued that except for some inherent natural problems, many of the factors can be intervened by provision of funds, creating awareness and behavioural changes for achievement of health care to a certain extent.
Literature Search
The paper adopted a literature search to find out different facts, figures and narratives of health financing. A literature search was done according to the objective of the paper. The role of health financing in provision of healthcare and UHC was inquired by focusing on various factors of health financing and their implications. The search engines like PubMed, Scopus, Web of Sciences and jstor have been consulted to unearth the mechanism of health financing and its importance. The search strategy used keywords like health financing, India, healthcare budget, out-of-pocket, health expenditure, health outcomes, donors, health insurance, fiscal structure, private sector, government sector, NGO sector, health sector performance and universal health care. Many of the words were searched in combined form to know the association of those factors. Manual searching was done to find out relevant authoritative sources about healthcare budgeting in India. Most of the articles considered for analysis in the paper were from 2010 onwards. Some of the landmark older papers were included due to the theoretical importance of those papers.
The details of phenomenon were arranged in various themes and sub-themes according to their importance and financial implication on the health structure of India. Issues like health financing and UHC in India have been discussed. The need for efficient health financing was also highlighted based on authentic sources. Health financing was discussed in length and breadth in Indian context which was collected from authoritative sources. The role of health financing by central government, international donor agencies, state governments and local bodies has been gathered, and arguments were built over the transformation of health system. The monitoring and evaluation mechanism for health financing has been analysed in context of recent developments of health sector reforms. Further, the challenges and opportunities of health financing were also discussed. The existing health financing models have been discussed to understand the relation of financing and overall healthcare development in India. Evidence from international organisations has also been put forward for the understanding of health financing and comparison across the countries.
Discussion
Low Health Sector Performance
The performance of health sector has been low in India due to many reasons. The failure of insurance and risk management is one of the major reasons for low performance. Health insurance has not been able to reach most of the individuals in the country [2]. The insured individuals would have better health-seeking behavior due to provision of funding by insurance companies. Common Indians find the cost of medical care as burdensome expenditure [3]. Ayushman Bharat is the new health insurance scheme of the government, which has been filling the gap in health sector for special categories of Indian population [14].
There is a lack of health services for suitable treatment in private, trust, and government sectors in many parts of the country, especially in rural areas. Non-availability and lack of accessibility to basic health services is a big concern [3]. The utilisation of resources varies irrespective of the population living in rural or urban areas. Transportation methods and long distances are major problems for rural people regarding utilisation of available health services. Rapid economic growth has led to a wider gap amongst people, which also leads to different kinds of injuries among masses due to mental health challenges, pollution, and environmental issues. The injuries like road traffic accidents, mental health, homicide and suicide are some of the byproducts of economic development in India. Road traffic accidents are also holding back economic development due to morbidity and mortality of the workforce [18]. Emergency care is needed at the earliest in such scenarios. Whereas, lack of health care facilities and transportation is a major drawback in tackling such issues. Recent changes in provision of infrastructure and manpower from the health ministry of government of India in different parts is addressing the regional divide [14].
The quality of health care services and governance of public health organisations are a great concern in India due to inadequate infrastructural facilities, allocation of funds, less staff, or even absenteeism of healthcare staff in many cases [3]. Most of the medicines are also not available in all health centers. The cleanliness of these places is not maintained, leading to people having apprehensions about the service they provide [19]. Healthcare service centers do not have major equipment and specialised doctors leading to unwanted referrals of patients to higher centers [19].
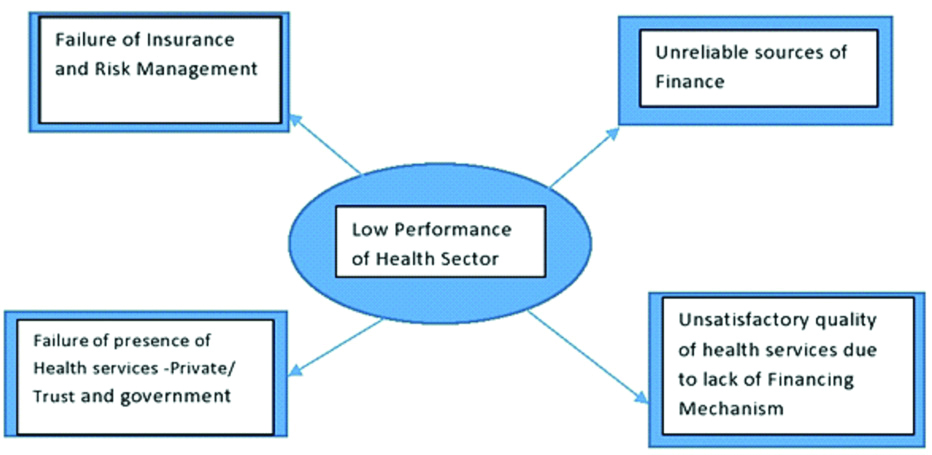
Unreliable sources of revenue also lead to low performance in provision of healthcare services. Increased contributions to the community-based insurance have been seen as a more reliable option for financing the poor who are facing health issues [4,15]. The cost of treatment many a time is beyond the affordability of low or middle-class people leading to only consultation but not treatment and medicine [20]. Government hospitals are available for people to receive treatment without cost. However, the facilities are limited, leading to a long waiting list [4]. A lot of voluntary organisations such as Milaap are working in India today to help the poor people with resources by doing crowdfunding or running a fundraiser campaign online [21]. The details of low performance of health sector are given in [Table/Fig-1].
Low performance of health sector.
Health Financing and Universal Health Coverage (UHC)
The UHC depends on robust healthcare financing, which supports for efficient use of money in health system. The fundamental concern for UHC are that irrespective of paying capacity, all are entitled to the most advanced healthcare technology or good health care in a nation [1]. Many countries in Latin America and South-East Asia achieved the UHC by provision of robust healthcare financing, which ranges from 4% to 8% of their GDP [4]. Countries like Thailand achieve the target by provision of sufficient healthcare to all people by empowering human resources, procurement of medicines and consumables, controlling emerging epidemics, providing primary care and curative care to people [22]. The nation provides a lot of scope in developing healthcare infrastructure, especially at primary level. The UHC provides scope for improvement of life of people and productivity. Indirectly productive citizens contribute to tax collection of the nation in long run, which can be used for creating more human development activities. A nation which is not providing UHC would lead to disastrous conditions although other development indicators keep improving. The people would be less creative, less productive and contribute less to the human development of the nation [23,24]. The UHC largely depends on provision of funding for infrastructure with strong commitment from the government. The exact percent of contribution from GDP of a nation for UHC and health sector development is unknown. Moreover, there is a need for a substantial contribution of approximately 6-8 % of GDP towards healthcare that is needed to achieve UHC. This financial provision may vary from country to country and the existing levels of human development aspects [4]. However, a country like India has always been a low financing country for the development of health sector [2].
In the twenty-first century, the period for achieving outcome of implementation of the UHC has come down drastically from the previous decades in the world due to technological innovation, data-driven decision making and modern development in medical sciences [23,24]. India should take this advantage of accelerated achievement in improving health sector goals in less time [1,2]. India will struggle less if more provision of funding would be there in the achievement of UHC. Indians also supply many drugs and medical devices to the developing and developed world due to its technological and business efficiencies. India has a robust human resources potential for the development of nations especially in health and wellness sector, which is always ready to serve even abroad. The only thing needed is to build capacity in medical and paramedical education for preparation of healthcare system [10,23,24].
The recent Astana Declaration in 2018 put primacy on health financing by political commitment from the member states of the WHO to facilitate the UHC. Further, the emphasis on the principles of primary health care (PHC) needs to be augmented by sufficient health financing [25,26]. Thus the component of equity and community participation for fostering human rights can be enhanced, which is already enshrined in Alma-Ata declaration in 1978 [25]. The health for all can be achieved by focusing on person-centered PHC care, which is one of the basic health services [26].
The objective of comprehensive PHC management, Health for All and UHC are facing difficulty due to various threats like lack of resources, human resources and infrastructure for implementation [25]. The lack of sustainable health financing is identified as one of the obstacles for lack of progress in health system in addition to factors like insecurity, conflicts, disease outbreaks, lack of political commitment, insufficient health workforce employment and lack of gender equity [27]. The efforts by various state governments on particular diseases by promoting vertical health programs and individual approaches in treatment helped in creating siloes in healthcare system rather than comprehensive care [28]. Therefore, there is a dare need to break the silos across health system by robust health financing for UHC by integrating all the services across the continuum of care.
Need for Efficient Health Financing
Adequate and timely financial resources are required to maintain a health system of high repute for the service of public. The development and maintenance of infrastructure need promising resources in a time-bound manner. The employment of adequate skilled workforce is required to put them in services of the public health system which need resources for training and development at various stages. Unlike many other industries, health care is very complex in terms of workforce and their management. Health systems employ doctors and paramedics in addition to non-clinical professionals to run the business. To prepare professionals ready for the service of a nation like India, it need much time and resources to attain desired standard [4]. The administrative and regulatory functions need a lot of meticulous planning to sustain the health system of a large scale for provision of care to the public [1]. Adequate health research is needed for the improvement of the health system in a time-bound manner. Mere import of research and development or technology transfer will not work in the strengthening of the health system. Every country has their challenges to tackle major health issues linked to local conditions. The research can be supported by maintenance of a good database with health information system along with an efficient team of researchers at every level for decision making [1,14]. Factors like wide outreach, accessibility, appropriate and affordable care can be achieved by UHC. It is near about impossible to achieve all these things without required public financing [23].
The low public health financing would place India in work in progress category rather than a successful player in the provision of healthcare. So, India can be considered as a place in health sector with an unfinished agenda for its poor performance. India achieved elimination of polio, guinea worm disease, yaws and maternal and neonatal tetanus in the last decades by providing sufficient funds for proper operation and monitoring of the diseases in the last decade [1,4].
It is difficult to achieve comprehensive health coverage for all in the absence of suitable and efficient financing models for building inclusive health. The provision of primary care cannot be achieved for half of the world’s population without free healthcare or at a very low cost [24]. This has a wide consequence of forcing 100 million people into poverty due to exorbitant healthcare expenditure. Recent evidence in India on health sector progress corroborates with the trajectory of global health financing from 1995 to 2014 in low-income and lower-middle-income countries, which shows that despite there is no marked increase in spending on the absolute term, they heavily depend on out-of-pocket spending and development assistance [29].
Quantum of Public Financing
Public health financing has been debated on different backgrounds. There is a requirement of sufficient funds to cover the medical expenditure of common man. However, the provision of health services with no cost to the people also does not go well with the spirit of the health financing and universal coverage [4]. In this backdrop, the WHO suggests that Out of Pocket Spending (OOPS) should not exceed above 15-20% of the healthcare expenditure [30]. Hence, for a country, the quantum of public health financing required can be easily estimated given the details of total healthcare budget for achievement of UHC. However, by strengthening health financing, a nation can achieve 100% healthcare coverage. The WHO also reiterates that to provide UHC in any country, there should be a provision of at least 5-6% of the GDP as public health financing which is also estimated by United Nations Sustainable Development Solution Network 2015 [14]. With such type of generous financing, India can achieve UHC by 2030 as per the requirement of Sustainable Development Goals (SDGs) [1]. It is also envisioned that both the state and centre have to increase the health financing to a great extent seriously. Out of the total outlay, the central government should always be in a position to spend 33 % of the total expenditure, and the rest would be borne by the state governments [14].
Health Financing and Role of Central Government
The central government in India has a great role in financing healthcare for the provision of primary, secondary and tertiary care. The word federal government is used interchangeably for the central government in various politico-economy discourses in India. Whereas, the word provincial government and state government are used interchangeably for government at state-level or provincial level. The central government usually launches most of the innovative programs for universal health care for the benefit of citizens. Though health is a state subject, there is still limited scope for the state governments to make budgetary provisions for continuation of health programs due to lack of fiscal resources. The state governments have little revenue sources to make provision for development of health infrastructure. There is a severe crunch of funds to take new healthcare initiatives for the benefit of population [1,14]. At this juncture, the central government has to take drastic steps for the provisioning of resources to create goodwill [5]. The central government has to provide resources to fight the communicable and noncommunicable diseases of national concern. Further, there should be provision of care in primary, secondary, and tertiary levels to create good healthcare infrastructure [14]. The central government has to play a role in upgrading the care with new developments for improvement of healthcare facilities. The state government has to create basic infrastructure of health care from its resources. Then, central government can upgrade with additional resources to accommodate the super specialty and specialty services as per regional requirement. There is also a need for assessment of the situation from time to time for an additional funds by the central government [1,14]. All these provisions should be synchronised for better healthcare and ultimately leads to UHC. Authors argue that the fiscal space and its infallible role for generation of financial resources for healthcare need to be well understood by the government [31,32]. Further, arguments are there for creation of fiscal space by the government in various methods like revenue mobilisation, grants and borrowings to strengthen the health system. After the generation of fiscal space, the prioritisation of expenditure towards healthcare depends on conducive macroeconomic policies in an economy by the central government [33,34]. The revenue mobilisation by government usually done by tax and non-tax revenue from various sources. The grants can be gathered from domestic and external sources. The borrowings can also be targeted from domestic and external sources for the improvement of health system [4,14,34].
Health Financing and Role of Provincial Government
Health being a state subject always has a mandate for the vast role for the provincial governments in India, which starts from preventive healthcare to provision of super specialty care. There is a need for sufficient finance from the state budget to develop a strong network of health centers. In India majority of the tax is collected by the central government, which has the power to utilise most of the resources according to the approval of parliament. So, it has been found there is a severe crunch of funds for the state governments to spend in health sector [1,4,14]. The state governments have more responsibility within its jurisdiction for human capital development, which includes health care services. Whereas limited resources make it almost impossible for implementing programs that are helpful to the people, especially in provision of healthcare services [5]. Further, the state governments have to provide the matching share in every central program, which is difficult for cash starved states. The matching share of state government ranges from 10-50% in various programs [35]. If a state does not provide sufficient matching share, they will lose the share of finance budget from the centre which otherwise they should get. Many states have limited resources and are not in a strong position to tackle the issues of finance. So, it is necessary for the states to improve sources of revenue for various health sector programs. The initiation of every program needs seed money, which is usually generated by states. The central government provides finance only when it realises the fund would be spent efficiently by the states which are subjected to audit by an independent auditor. To ensure this, provincial governments must have a firm team of monitoring and evaluation of the program in health sector. Overall the provincial government must have basic level financing for the development of strong healthcare infrastructure which can provide UHC [14,35]. Researchers argue that domestic health financing systems should be effective and resilient to achieve better coverage of healthcare. The financial achievement of provinces is important for UHC. There should not be any financial barriers to prevent people from using health services for prevention, promotion, treatment and rehabilitation care. The most important thing is to make sure that financial hardship should not be there for state governments [36].
The public hospitals are in the services of poor people in comparison to their richer counterparts. Whereas services of private hospitals are limited to the use of rich [2]. Moreover, maintenance of public hospitals is done by public funding to help the poor access the healthcare services. Researchers observe that irrespective of urban and rural areas, the public facilities run by state governments are always creating more equity than the private healthcare facilities [2]. There is a need for better financing of the public healthcare institutions in the provinces.
Health Financing and Role of Local Bodies
The local bodies in India provide healthcare to many people in rural and urban areas. They manage hospitals, health centres and campaign for immunisation and other preventive care services [37]. All these things need a huge amount of investment in health sector. Whereas, the local bodies struggle to generate such fund from their resources in India. The relatively wealthy corporations like Mumbai, Delhi, Bengaluru, Chennai and Hyderabad may not face problems in generating finance for spending in health sector. But, small towns and rural local bodies face huge challenges in generating resources for the delivery of healthcare. Overall, local bodies face challenges due to a lack of funding [38]. The grants received by the local bodies are not great for healthcare spending in their locality. The local bodies also spend money on programs like sanitation, nutrition, and education, which are indirectly influencing health of people [37]. So, there is a great need for the local bodies to finance sufficiently to further the actions for development of health sector. Unlike national health programs, the local bodies can intervene in the issues and challenges of their localities in health sectors. Local governments mostly do the plan and programs according to the need assessment, which is suitable for a particular time and geography [3]. There is a need to strengthen the local governments for health sector developments. The capacity building of healthcare workforce in local governments at district and sub-district level is required for improving the governance [37]. The local bodies have to mobilise other resources for the development of health sector by involving sanitation, water supply, control of epidemic, maintenance of food safety, reduction of drug consumption and increasing recreational facilities within their geography [4,14]. All these additional aspects now-a-days require critical interventions for human development by the local governments.
Health Financing and Role of International Donor Agencies
International donors have a say in the health financing of any country if they are financing various health programs. The bodies like Bill and Melinda Gates foundation always help in maternal health, child health, nutrition and other pressing health problems in some districts of India. They push for better programs with outcome-based interventions in the hard to reach areas. The international donors help in bringing more funds for the strengthening of existing health systems [39]. This usually helps in thinking in a new dimension of healthcare for better health outcomes. The international donors also ensure the fund provided by them match their mission and vision. The sectors they choose have to be aligned with the bigger work they do in the international arena. The international organisations chucked out plan outlay on a time frame basis in targeted areas for improvement of certain health indicators. Some international NGOs like CARE foundation, Bill and Melinda Gates Foundation allow the recipient country to function according to existing plans and in existing health structure. In those organisations, the existing health department of state governments works hand-in-hand as per local needs. The health financing by international NGOs sometimes goes down well when there is perceived achievement of their objectives in health sector. Many international NGOs have a clear cut exit policy to wind up their business [39]. In India, many philanthropic activities through foreign countries stopped after the targets were achieved. So, this is not a perennial source for health financing to build a state of the art health infrastructure [14]. The foreign NGOs have some pressing obligation towards the causes of human services, and they usually do their bit. They cannot be relied on for long term grants in health sector to build the capacity. There is difficulty in convincing them for certain health causes to be financed by them [4].
Sometimes funding may be a hindrance in implementing health programs. However, inefficiency creates problems in rolling out flagship programs meant for the vulnerable populations. Corruption affects healthcare programs with the involvement of high-level personnel [2]. Unless corruption is tackled, there is no meaning of reform in healthcare financing [2].
The donor commitments of funds for development of health has been increased more than four times since 2000 from time of the Millennium Development Goals (MDG) Declaration [40]. This amount reached around US$ 20 billion in 2008 [40]. However, the progress in achieving MDGs is quite unsatisfactory [41]. Attempts are made to bring more resources with an efficient operational mechanisms for progress of health system [42].
Monitoring and Evaluation Mechanism for Health Financing
The monitoring and evaluation mechanism for health financing in India needs improvement. Many ongoing healthcare projects do not have sufficient funds for completion. Infrastructural projects have been halted due to various reasons about a lack of finance. The lack of funds at different levels is commonly discussed in public domain for the completion of necessary work. There would be a barrage of issues due to lack of funds in ongoing projects [43]. Further, revised estimate always tend to be higher, and the projects get into the trap of non-completion, leading to a lack of healthcare services [43]. So, it is always advised to assess the feasibility of projects for garnering timely benefits. For which monitoring of financial mechanisms of the projects is very much needed. The provision of sufficient funds can be made for a strong monitoring mechanism of the projects for timely completion of projects and raising red flags [42]. In the age of information technology, it is not difficult to monitor projects of health systems having the utmost importance [14,42]. The grants provided by central and state governments have to be appraised for the projects immediately to assess the progress. There is a need for smart governance in financial aspects of health care by involving all the stakeholders [37].
There is another aspect of monitoring of finances in India, which many people complain of. The strict financial monitoring acts as a huddle in receiving timely financial resources for implementation of program. The rules and regulations of financial monitoring make trouble every-now-and-then which is difficult for progress of the system [14,43]. There are hurdles in releasing money and providing financial statements. The government audit system led by Controller and Auditor General (CAG) with its archaic rules and regulations is creating a problem for progress of the health system. The Indian audits system is very much colonial and needs to be responsive according to the need of the hour. Indian audit system creates problems in various stages of the project rather than bringing efficiency in the entire process [4].
According to the WHO, there are six building blocks required for the functioning of health system. These important building blocks of any health system are leadership and governance, health financing, health workforce, medical products and technologies, information, research, and services delivery [10]. The WHO model put primacy on healthcare financing to a great extent. The diverse healthcare system of India with a mix of state and central health services with public, private and voluntary divisions helps in improving the implementations of health programs. The predominant allopathic and AYUSH system of medicine with their registered and unqualified medical practitioners exists alongside all types of healthcare in India [44]. It is difficult to establish one or two types of health financing in India. Further, monitoring of such complex health system needs smart monitoring mechanism.
There should be sufficient effort to provide financial risk protection by monitoring different services as well as health financing [4]. The health services provided by clinicians like rational use of technology in healthcare, efficiency and affordability is really helpful. This would lead to cost-effective and reliability of healthcare among people [45].
Challenges of Health Financing
India is well known for its low level of public financing of healthcare [4]. The share of public health financing of GDP in India is abysmally low, with a range between 0.9 to 1.2% [23]. The per capita health expenditure of India remain low in comparison to many other countries [4]. Very low fraction of health care expenditure on people has been spent by public financing system. Whereas, most of the expenditure is borne by the people from out-of-pocket [23]. This phenomenon put tremendous pressure on the financial condition families and individuals, which push them into the brink of poverty [43]. Some studies found that approximately 7% of the people suffer from health-related poverty in India [14,43]. The majority of costs borne by individuals are on hospitalisation, outpatient care and essential medicines for cure of diseases [43]. Outpatient care is about 70% of overall expenditure. Within this, medicine cost is about 70% of the total outpatient care cost. The hospitalisation many a time causes catastrophic expenditure causing long term owes to the families due to loss of major resources [43,44]. There is a lack of access to medicine by the average Indians despite India is known as the world pharmacy of medicine with its high level of production.
In addition to the expenditure of direct medication, there is also indirect expenditure incurred by the patient. These indirect expenditures include loss of wage, transport cost, and bribes in public hospitals [43, 44]. No health system covers such expenditure of the patient to alleviate the financial hardship. Therefore, good governance is advocated for accessible and affordable health care. To provide such good governance, public financing is necessary for protection of marginalized groups [44].
Way Forward
Despite gloomy health financing conditions, there are silver lines in the Indian health sector to harvest good health. The strong economic foundation of India can help in achieving targets of health sector in the long run. The enhanced growth of economy coupled with low inflation and a high degree of global competitiveness would help in achieving the targets. The economic growth and health sector performance have to go hand in hand for the development of the country [4,46]. Increasing participation in health insurance schemes would help reduce expenditure of people. The health insurance would help to avoid falling below the poverty line in India, which would ultimately help in reducing the burden of diseases [43,44].
The health financing needs to be focused on population and public health care programs with uninterrupted resources [2]. Special budget is needed for the development of digital health as a critical enabler for healthcare in a rural areas [2,14].
The UHC not just helps in reducing diseases but also protects from financial risk, which enables a continuum of care. Good health outcomes are possible by increasing access to sufficient financing [1]. A study shows that only 25% of India’s population can have access to health services without much difficulty [47]. However, the availability of health insurance may not be helpful if the available health centres not equipped with infrastructure for treatment. Further, the health centres should not be far off from locality or community. In addition to this, the requirement of human resources and essential equipment should be available to provide services.
Just by using tax payer’s money in purchase of insurance from private firms and treatment in private hospitals have some negative aspects also. The opportunity cost governments bear by denying upgradtion of the primary health care infrastructure and human resources in public sector is detrimental for the progress of health system [1]. So, the Government should not only depend on health insurance; rather it should strengthen the primary care services with the fiscal provision in every budget.
There is a glaring gender-based discrimination in sex-selective abortion, nutrition, and provision of health care in low and middle-income countries. Women are discriminated more when health care cost is paid by borrowing, and sale of assets by family members [48]. So, there is a requirement of efficient health financing for empowerment of women from the government.
The sanitation program in India is a successful attempt for transformation in recent times. Various stakeholders contribute to the development of such public health projects [46]. The government, private sector, NGO sector, public funding and individual member’s contribution helped a lot. All the stakeholders have adopted an innovative strategy to finance for sanitation program. Overall, access to sanitation increases dramatically by providing sufficient finance. A study found that only provision of toilets would not help much in achieving sanitation. Rather there is a requirement of full-fledged financing required for maintenance of these created infrastructures [49]. The programs like Swachh Bharat Abhiyan is only a small part of the bigger sanitation project which need all-round financing of the infrastructural project [49].
Authors argue that critical issues like financing ventures in health sector, along with better coordination and implementation of the protocols and projects, are required. There is also a need for following up medical cases and examining all scenarios with use of evidence-based scientific methods. So, provision of finance plays an important role in achieving the target [50].
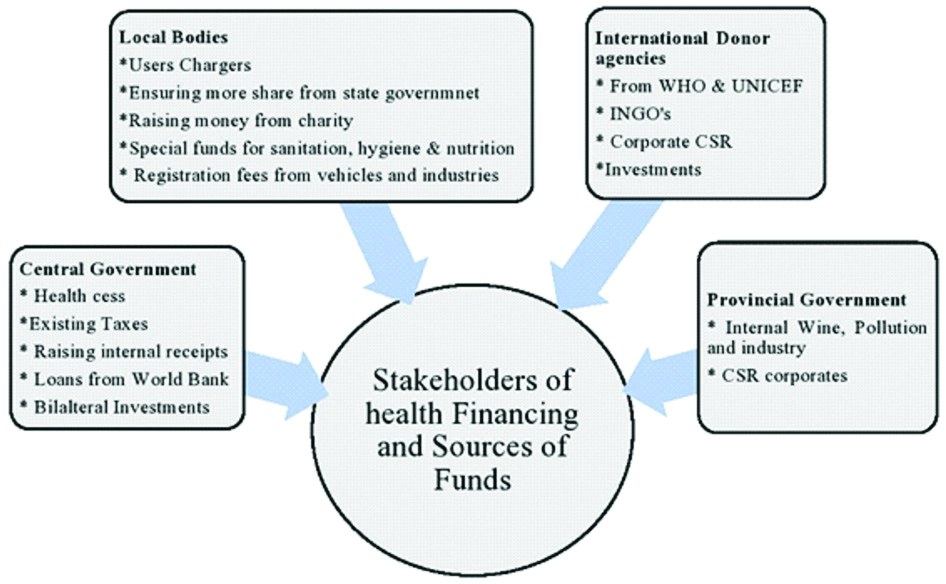
Health financing largely depends on the generation of revenue and involvement of various stakeholders. Therefore, the roles and responsibility of stakeholders on health financing need to be identified properly. [Table/Fig-2] provides a detailed account of fund generation from various stakeholders and the roles thereof.
Stakeholders on health financing and sources of fund.
Conclusion(s)
The entire health system revolves around health financing in India, which was found to be lagging. All the programs need a continuous stream of resources like medicine, human resources, physical infrastructure, monitoring and evaluation for grand success. Whereas, different stakeholders also need financial support to evolve with great vigour and vivacity. It can be suggested that there is a pressing need to infuse funds into public health system for achievement of universal health care rather than incremental growth in the usual financial process spreading over several decades. The particular roles and responsibilities of federal, provincial, local governments, along with international donors, have to be delineated for expedition of the resource mobilisation for a just and competent health system. However, while implementing programs, there should be coordination among all the stakeholders.
[1]. Mukherjee K, Selective universalism: The paradoxical strategy to achieve universal health coverage in IndiaJournal of Health Management 2019 21(1):154-59.10.1177/0972063418821826 [Google Scholar] [CrossRef]
[2]. Prinja S, Kumar MI, Pinto AD, Jan S, Kumar R, Equity in hospital services utilisation in IndiaEconomic and Political Weekly 2013 48(12):52-58. [Google Scholar]
[3]. Dehury RK, Samal J, Coutinho S, Dehury P, How does the largely unregulated private health sector impact the Indian mass?Journal of Health Management 2019 21(3):383-93.10.1177/0972063419868561 [Google Scholar] [CrossRef]
[4]. Duggal R, Financing healthcare in India-prospects for health insuranceCehat 2015 (1):01-10.http://www.cehat.org/go/uploads/Publications/A%20246%20Financing %20healthcare.pdf [Google Scholar]
[5]. Behera DK, Dash U, Prioritization of government expenditure on health in India: A fiscal space perspectiveSocioecon Plann Sci 2019 68:10066710.1016/j.seps.2018.11.004 [Google Scholar] [CrossRef]
[6]. Chatterjee P, India launches Ayushman Bharat’s secondary care componentLancet 2018 392(10152):99710.1016/S0140-6736(18)32284-0 [Google Scholar] [CrossRef]
[7]. Christensen IA, Hay JW, Peura AD, National Development Through Space: India as a ModelInSpace Technologies for the Benefit of Human Society and Earth 2009 1Springer, Dordrecht:453-82.10.1007/978-1-4020-9573-3_18 [Google Scholar] [CrossRef]
[8]. Fullman N, Yearwood J, Abay SM, Abbafati C, Abd-Allah F, Abdela J, Measuring performance on the Healthcare Access and Quality Index for 195 countries and territories and selected subnational locations: A systematic analysis from the Global Burden of Disease Study 2016Lancet 2018 391(10136):2236-71.10.1016/S0140-6736(18)30994-2 [Google Scholar] [CrossRef]
[9]. Science The WIRE. India Ranks 154 Among 195 Countries in Healthcare Index. 2017. https://science.thewire.in/health/india-rank-healthcare-index/ [Google Scholar]
[10]. World Health Report Health systems financing: The path to universal coverage World Health Organisation, Geneva. 2010. https://www.who.int/whr/2010/en/ [Google Scholar]
[11]. Kalra A, India’s universal healthcare rollout to cost $26 billionReuters 2014, October 30 http://in.reuters.com/article/uk-india-health-idINKBN0IJ0VN20141030 [Google Scholar]
[12]. International Monetary Fund. 2016. Report for selected countries and subjects: IMF Annual Report 2016. https://www.imf.org/external/pubs/ft/ar/2016/eng/pdf/ar16_eng.pdf [Google Scholar]
[13]. Mukherjee K, Haycox A, Walley T, Health technology assessment: A potential road map for IndiaInt J Med Sci Public Health 2017 6(5):969-73.10.5455/ijmsph.2017.1269225012017 [Google Scholar] [CrossRef]
[14]. Ministry of Health and Family Welfare, Government of India. National Health Policy -2017. https://www.nhp.gov.in/nhpfiles/national_health_policy_2017.pdf [Google Scholar]
[15]. Health in India, 2017Lancet 2017 389:12710.1016/S0140-6736(17)30075-2 [Google Scholar] [CrossRef]
[16]. Kumar AS, Chen LC, Choudhury M, Ganju S, Mahajan V, Sinha A, Sen A, Financing health care for all: challenges and opportunitiesLancet 2011 377(9766):668-79.10.1016/S0140-6736(10)61884-3 [Google Scholar] [CrossRef]
[17]. National Health Agency. About Pradhan Mantri Jan Arogya Yojana (PM-JAY). 2020. https://pmjay.gov.in/about/pmjay [Google Scholar]
[18]. World Bank. Road Deaths and Injuries Hold Back Economic Growth in Developing Countries. 2018. https://www.worldbank.org/en/news/press-release/2018/01/09/road-deaths-and-injuries-hold-back-economic-growth-in-developing-countries [Google Scholar]
[19]. Kasthuri A, Challenges to healthcare in India-The five A’sIndian J Community Med 2018 43(3):141-43. [Google Scholar]
[20]. Samal J, Dehury RK, An exploration and assessment on the current status and trend of Third Party Administrators (TPA) in IndiaInternational Journal of Health Sciences and Research (IJHSR) 2015 5(8):600-04. [Google Scholar]
[21]. Milaap. Overview. 2020. https://milaap.org/about-us/overview [Google Scholar]
[22]. Sumriddetchkajorn K, Shimazaki K, Ono T, Kusaba T, Sato K, Kobayashi N, Universal health coverage and primary care, ThailandBull World Health Organ 2019 97(6):415-22.10.2471/BLT.18.223693 [Google Scholar] [CrossRef]
[23]. World Health Organisation. Arguing for universal health coverage. 2013. https://apps.who.int/iris/bitstream/handle/10665/204355/9789241506342_eng.pdf [Google Scholar]
[24]. Universal health coverage (UHC). 2019. Available: https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc) [Google Scholar]
[25]. UNICEF. World Health Organisation., & International Conference on Primary Health. Declaration of Alma-Ata International Conference on primary health care, Alma-Ata, USSR, 6-12 September 1978. Development, 1978:159-61 [Google Scholar]
[26]. Rifkin SB, Alma Ata after 40 years: primary health care and health for All-from consensus to complexityBMJ Glob Health 2018 3:e00118810.1136/bmjgh-2018-00118830622747 [Google Scholar] [CrossRef] [PubMed]
[27]. Kraef C, Kallestrup P, After the Astana declaration: Is comprehensive primary health care set for success this time?BMJ Glob Health 2019 4(6):e00187110.1136/bmjgh-2019-00187131799000 [Google Scholar] [CrossRef] [PubMed]
[28]. Mills A, Mass campaigns versus general health services: What have we learnt in 40 years about vertical versus horizontal approaches?Bull World Health Organ 2005 83(4):315-16. [Google Scholar]
[29]. Dieleman J, Campbell M, Chapin A, Evolution and patterns of global health financing 1995-2014: Development assistance for health, and government, prepaid private, and out-of-pocket health spending in 184 countriesLancet 2017 389:1981-2004.(10083) [Google Scholar]
[30]. Evans DB, Etienne C, Health systems financing and the path to universal coverageBulletin of the World Health Organization 2010 88:40210.2471/BLT.10.07874120539847 [Google Scholar] [CrossRef] [PubMed]
[31]. Heller PS, The prospects of creating ‘fiscal space‘ for the health sectorHealth Policy and Planning 2006 21(2):75-79.10.1093/heapol/czj01316415338 [Google Scholar] [CrossRef] [PubMed]
[32]. Tandon AL, Cashin C, Assessing public expenditure on health from a fiscal space perspectiveThe World Bank, NW Washington, DC 20433 (2010) [Google Scholar]
[33]. Tandon AL, Fleisher L, Yap WA, Reprioritizing government spending on health: Pushing an elephant up the stairs?WHO South-East Asia J Public Health 2014 3(3):206-12.10.4103/2224-3151.20674228612804 [Google Scholar] [CrossRef] [PubMed]
[34]. McIntyre D, Kutzin J, World Health Organisation. Health financing country diagnostic: A foundation for national strategy developmentWorld Health Organisation 2016 [Google Scholar]
[35]. Ministry of Health and Family Welfare. National Rural Health Mission: Meeting people‘s health needs in rural areas. 2005. https://nhm.gov.in/WriteReadData/l892s/nrhm-framework-latest.pdf [Google Scholar]
[36]. Carrin G, Mathauer I, Evans DB, Universal coverage of health services: Tailoring its implementationBull World Health Organ 2008 86(11):857-63.10.2471/BLT.07.04938719030691 [Google Scholar] [CrossRef] [PubMed]
[37]. Panda B, Zodpey SP, Thakur HP, Local self-governance in health-a study of it‘s functioning in Odisha, IndiaBMC Health Serv Res 2016 16(6):55410.1186/s12913-016-1785-828185587 [Google Scholar] [CrossRef] [PubMed]
[38]. Aijaz R, Challenges for Urban Local Governments in IndiaAsia Research Centre Working Paper 19 2007 http://www.lse.ac.uk/asiaResearchCentre/_files/ARCWP19-Aijaz.pdf [Google Scholar]
[39]. Park K, Park‘s textbook of preventive and social medicine 2019 JabalpurBanarsidas Bhanot [Google Scholar]
[40]. OECD Stat Extracts. Paris: Organisation for Economic Co-operation and Development; 2010. Available from: http://stats.oecd.org/Index.aspx?DatasetCode=CRSNEW [Google Scholar]
[41]. The Millennium Development Goals report 2009. New York: United Nations; 2009 [Google Scholar]
[42]. Evans DB, Etienne C, Health systems financing and the path to universal coverageBull World Health Organ 2010 88:402Adoi:10.2471/BLT.10.078741 https://www.scielosp.org/article/bwho/2010.v88n6/402-403/en/10.2471/BLT.10.07874120539847 [Google Scholar] [CrossRef] [PubMed]
[43]. Selvaraj S, Farooqui HH, Karan A, Quantifying the financial burden of households‘ out-of-pocket payments on medicines in India: A repeated cross-sectional analysis of National Sample Survey data, 1994-2014BMJ Open 2018 8(5):e01802010.1136/bmjopen-2017-01802029858403 [Google Scholar] [CrossRef] [PubMed]
[44]. Reddy KS, Health care reforms in IndiaJAMA 2018 319(24):2477-78.10.1001/jama.2018.528429800246 [Google Scholar] [CrossRef] [PubMed]
[45]. Tangcharoensathien V, Patcharanarumol WIrP, Aljunid SM, Mukti AG, Akkhavong K, Banzon E, Health-financing reforms in southeast Asia: Challenges in achieving universal coverageLancet 2011 377(9768):863-73.10.1016/S0140-6736(10)61890-9 [Google Scholar] [CrossRef]
[46]. Lakshminarayanan S, Role of government in public health: Current scenario in India and future scopeJ Family Community Med 2011 18(1):26-30.10.4103/1319-1683.7863521694957 [Google Scholar] [CrossRef] [PubMed]
[47]. Business Standard, Only around 25% of the population has access to healthcare services in India 2015 Available from: http://www.business-standard.com/article/news-cm/only-around-25-of-the-population-hasaccess-to-healthcare-services-in-india-115060301032_1.html [Google Scholar]
[48]. Saikia N, Moradhvaja Gender disparities in Health-Care Expenditure (HCE) and financing strategies for in-patient care in IndiaSSM-Population Health 2019 :10037210.1016/j.ssmph.2019.10037231998823 [Google Scholar] [CrossRef] [PubMed]
[49]. Malik S, Bharti N, Models of financing sanitation infrastructure initiatives in India: Challenges and opportunitiesInternational Journal of Innovative Technology and Exploring Engineering 2018 8(11):392-400.10.35940/ijitee.K1070.09811S19 [Google Scholar] [CrossRef]
[50]. Sharma R, Hossain MM, Strengthening public health partnerships in India: Envisioning the role of law enforcement during public health emergenciesIndian J Community Med 2019 44(3):188-92.10.4103/ijcm.IJCM_110_1931602100 [Google Scholar] [CrossRef] [PubMed]