Endodontic treatment was made possible because of the successful pain control. Pain is a complex phenomenon involving biologic and psychological factors. Biologically, pain is multilevel system that begins with the detection stimuli by the peripheral nerves, then the medullary spinal cord processes the stimuli and the processed information is felt as pain in higher brain regions such as the cerebral cortex. The endogenous and exogenous factors can influence this process which results in modification of the pain perception [1].
Local anaesthetic administration has been the key to control pain during endodontic procedure. It is often challenging to anaesthetise the tooth with irreversible pulpitis. Many patients reported pain during endodontic treatment in teeth with irreversible pulpitis even after achieving the clinical signs of analgesia like numbness of lip & tongue in case of inferior alveolar nerve block and numbness of buccal mucosa in case of infiltration [2].
The role of voltage-gate Na+ channels in inflammatory states is of particular interest because they contribute to neuronal hypersensitivity, and up-regulation of some voltage-gated Na+ channel isoforms, which play key roles in local anaesthetic failure when treating inflamed pulps. Sodium channels have subpopulations in the nerve membrane, which can be pharmacologically classified according to whether they are sensitive or resistant to Tetrodotoxin (TTX). Sodium channels that are TTX-Resistant (TTX-R), such as Nav1.9 channels, are about 4 times more resistant to the effects of lidocaine than TTX-sensitive Na+ channels in inflammatory state [3].
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) diminish inflammation at different levels in the inflammatory process. NSAIDs block the cyclooxygenase enzyme, resulting in lower levels of inflammation-inciting prostaglandins [4].
There have been multiple studies conducted on the influence of premedication with NSAIDs on the success of inferior alveolar nerve block anaesthesia [4-7]. All these studies evaluated inferior alveolar nerve block where local anaesthesia is administered away from the site of inflammation produced by irreversible pulpitis. So a study aimed at evaluating the effectiveness of premedication with NSAIDs in maxillary infiltration anaesthesia where the local anaesthesia administered is directed to periapical area of the tooth with irreversible pulpitis is required. The purpose of this double-blind, randomised controlled clinical trial is to evaluate and compare the effectiveness of oral premedication with three different drugs IBUP, PARA, and DS on improving the outcome of maxillary infiltration anaesthesia in patients with irreversible pulpitis.
Materials and Methods
This study was approved by the Ethics Committee of KLE University of Medical Sciences in India. This double-blind, randomised controlled clinical trial study done in the Department of Conservative Dentistry and Endodontics, KLE VK Institute of Dental Sciences, Belgaum. A total of 120 patients with irreversible pulpitis of permanent maxillary first molar teeth diagnosed by electric pulp-testing device (parkell) and cold stimulus (EndoFrost, Coltene/Whaledent) participated during the period between years 2015-17 [Table/Fig-1].
Flow Chart of study design.
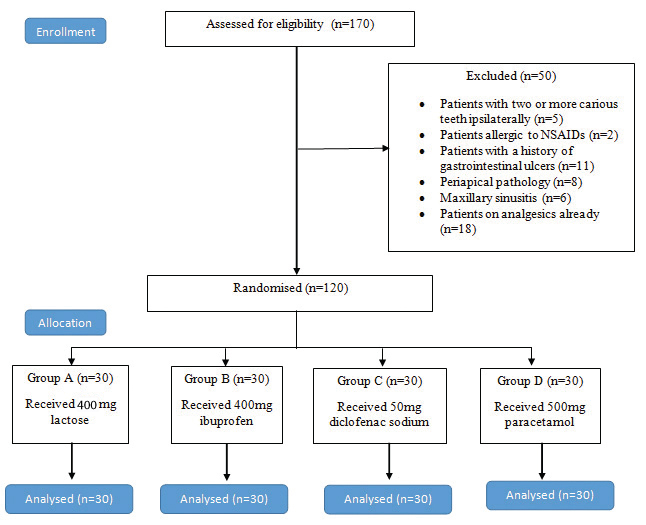
Exclusion criteria: The presence of systemic disorders, those requiring root canal treatment of two or more teeth ipsilaterally, known allergy to NSAIDs, or with a history of gastrointestinal ulcers, Periapical pathology, Aggressive periodontitis, Maxillary sinusitis or Patients already on analgesia within 24 hours before the treatment were excluded from the study.
Inclusion criteria: Healthy patients having first maxillary molar tooth with irreversible pulpitis without periapical pathology, belonging to age group of 18-50 years without any medical history were included in the study.
The clinical diagnosis of irreversible pulpitis was confirmed by a response to an electric pulp test with lingering pain for more than 10 seconds after cold test and electric pulp test and belonging to the age group of 18-50 years with noncontributory medical history and periapical pathology to be confirmed radiographically.
After taking affirmatory consent form from each patient, A single operator had evaluated and performed treatment of all the patients to avoid inter-examiner bias. The age and sex of the patient were also recorded and standard deviation is analysed at the end of the study to co-relate the confounding factors in the form of varying pain threshold between different subjects.
To randomise the patients, number of patients under each group was written on paper and kept in a sealed opaque envelope. After that each patient was alloted to the group according to the number chosen by them. Allocation of the patients was done by a trained dentist who was blinded to the treatment procedures.
To facilitate the double-blind study all groups of drugs IBUP 400 mg (BRUFEN400), PARA 500 mg (DOLO- 500), DS 50 mg (VOVERAN 50), and a placebo 400 mg lactose were customised by a pharmacist. The pharmacist prepared capsules similar in shape, size and colour and encoded them so that the clinicians and patients did not know about the placbeo or NSAIDs medication that was taken. The pre-intervention pain score with electric pulp test was recorded on the Heft parker visual analog scale by asking patient to place mark on the 170 mm long line. The millimeter marks were removed from the scale, and the scale was divided into four categories no pain corresponded to 0 mm; faint, weak or mild pain corresponded to 1-54 mm; moderate to severe pain corresponded to 55-114 mm; and strong, intense maximum possible pain corresponded to more than 114 mm [7]. Patients were instructed to place a mark on the line to indicate the pain; this mark was then measured with the scale and the score was recorded. Patient is given either one of the drugs of group A, group B, group C or group D orally according to the allocated group by randomisation. Patient was asked to wait for one hour before the treatment initiation to allow the drug to reach its maximum plasma concentration. Local anaesthesia was administered with 2% lignocaine in 1:80,000 concentration adrenaline through 0.6 mL by buccal infiltration and 0.2 mL by palatal infiltration using 26 gauge 38 mm needle. After 5 minutes, numbness was checked. Those patients where there is a failure to achieve numbness due to procedural error were to be excluded from the study. None of the subjects were excluded from the current study as procedural error was not encountered.
After achieving numbness and isolation with rubber dam, the access cavity preparation was initiated with Endo access bur (DentsplyMaillefer). The patients had to rate any pain that they experienced during access cavity preparation. This was recorded as pain within dentin, when entering the pulp chamber, or when a 10# k-file (Kendo, VDW, Munich, Germany) was inserted into the root canals. Root canal treatment was completed according to the standard protocol. No or mild pain is classified as success of anaesthesia. Moderate and severe pain is classified as failure of anaesthesia.
Statistical Analysis
Data was recorded on an excel sheet under respective groups A, B, C, D to prevent investigator bias. The data was statistically analysed by using SPSS software (version 20).
Comparison of 4 groups: statistical analysis was performed by two way ANOVA test. Pairwise comparison of four main groups (A, B, C, D) and four positions (Pre-op, Bur is in dentin, Bur enters the pulp chamber and on pulp extirpation) with respect to pain score on Heft Parker scale was analysed by Tukey’s multiple post-hoc procedures. The comparisons were considered significant if p<0.05.
Results
Disclosure of the envelope containing the particulars of the drug dispensation during the customisation of the capsules revealed that Group A subjects were administered 400 mg lactose, Group B subjects were administered 400 mg IBUP, Group C subjects were administered DS 50 mg, and Group D subjects were administered 500 mg PARA.
From the [Table/Fig-2,3] obtained through statistical analysis, the mean pain score of all the patients from the particular group (A, B, C or D) at any phase of treatment (whether preoperatively or on pulp extirpation) can be compared to any group’s (A,B,C or D) treatment phases (whether preoperatively oron pulp extirpation) by intersecting p-value between them in the table to find if the difference is significant or not.
Pairwise comparison of four main groups (A, B, C, D) and two positions (Pre-op and on pulp extirpation) with respect to pain score on heft parker scale by Tukey’s multiple post-hoc procedures (p<0.05). *p-value significant.
| Groups with positions | Group A (PLAC) with Pre-op | Group A with on pulp extirpation | Group B (IBUP) with Pre-op | Group B with on pulp extirpation |
|---|
| Mean | 120.37 | 91.57 | 124.47 | 45.00 |
| SD | 24.12 | 46.15 | 23.48 | 37.96 |
| Group A with Pre-op | - | | | |
| Group A with On pulp extirpation | p=0.2202 | - | | |
| Group B with Pre-op | p=0.9990 | p=0.0737 | - | |
| Group B with On pulp extirpation | p=0.0001* | p=0.0004* | p=0.0001* | - |
| Group C (DS) with Pre-op | p=0.9990 | p=0.0752 | p=0.9990 | p=0.0001* |
| Group C with On pulp extirpation | p=0.0001* | p=0.0013* | p=0.0001* | p=0.9990 |
| Group D (PARA) with Pre-op | p=0.9986 | p=0.0048* | p=0.9990 | p=0.0001* |
| Group D with On pulp extirpation | p=0.0001* | p=0.0201* | p=0.0001* | p=0.9999 |
Pairwise comparison of two main groups (C & D) and two positions (Pre-op and on pulp extirpation) with respect to pain score on heft parker scale by Tukey’s multiple post-hoc procedures (p<0.05).
| Groups with positions | Group C with (DS) Pre-op | Group C (DS) with On pulp extirpation | Group D (PARA) with Pre-op | Group D (PARA) with On pulp extirpation |
|---|
| Mean | 124.40 | 47.93 | 132.13 | 54.73 |
| SD | 20.30 | 40.69 | 16.32 | 45.18 |
| Group C (DS) with on pulp extirpation | p=0.0001* | - | | |
| Group D (PARA) with Pre-op | p=0.9990 | p=0.0001* | - | |
| Group D with on pulp extirpation | p=0.0001* | p=0.9990 | p=0.0001* | - |
*denote significant p-value
As tabulated in [Table/Fig-4], the results are as follows: In group A, during the treatment procedure there is 20% success rate and 80% failure rate. Tukey’s multiple post-hoc procedures showed no significant difference (p=0.2202) between the preoperative pain and on pulp extirpation within the group.
Results (H-P scale: Heft Parker Scale).
| Groups | No pain 0 mm on H-P scale | Mild pain 1-54 mm on H-P scale | Moderate pain 55-114 mm on H-P scale | Severe pain 114 mm on H-P scale |
|---|
| Group A(400 mg lactose) | 2.5% | 17.5% | 33.33% | 46.67% |
| Group B(400 mg ibuprofen) | 17.5% | 47.5% | 9.17% | 25.83% |
| Group C(diclofenac sodium 50 mg) | 8.33% | 52.50% | 9.17% | 30.00% |
| Group D(500 mg paracetamol) | 10.00% | 48.33% | 7.50% | 34.17% |
| Successful anaesthesia | Failure of anaesthesia |
In group B, during the treatment procedure there is 65% success rate and 35% failure rate. Tukey’s multiple post-hoc procedures showed significant difference (p=0.0001) between the preoperative pain and on pulp extirpation within the group.
In group C, during the treatment there is 60.83% success rate and 39.17% failure rate. Tukey’s multiple post-hoc procedures showed significant difference (p=0.0001) between the preoperative pain and on pulp extirpation within the group.
In group D, during the treatment procedure there is 58.33% success rate and 41.67% failure rate. Tukey’s multiple post-hoc procedures showed significant difference (p=0.0001) between the preoperative pain and on pulp extirpation within the group.
Discussion
Almost 85% of all dental emergencies are caused by the pulpal or periapical disease; of these emergencies 50% are associated with irreversible pulpitis which would require either endodontic treatment or extraction to relieve the symptoms [8].
If complete pulpal anaesthesia could be achieved, the pulp could be removed in one visit, which would give more rapid pain relief for patients and considerably reduce the time spent on emergency primary dental care. But in the presence of acute inflammation, conventional infiltration or block local anaesthetic injections may not achieve complete anaesthesia [9].
Nociceptive neurons within human trigeminal ganglion express multiple voltage-gated sodium channels (VGSCs), of which the TTX-R channel Nav1.9 has been suggested to play a major role in inflammatory pain. Wells JE et al., through their molecular research has suggested the existence of at least nine subtypes of VGSCs that differ in their expression pattern and roles in mediating peripheral pain. The TTX-R currents are preferentially expressed in small trigeminal neurons, which give rise to thinly myelinated Aδ-fibers and unmyelinated C- fibers, many of which are nociceptive [3].
Sensitisation of TTX-R channels by prostaglandins in inflammation resists the local anaesthesia by lowering the activation threshold and increasing the amount of sodium ions that flow through the channel. In other words, an inflammation induces elevation in prostaglandin levels and sensitises TTX-R channels, leading to depolarisation at lower levels of stimulus strengths. This may explain the reason for failure of anaesthesia and increased response to stimulus in irreversible pulpitis [10]. So, in the current study by administration of NSAIDs preoperatively, we tested the theory that advocates the sensitisation of TTX-R resistant sodium channels by prostaglandins as a reason for the failure of local anaesthesia in irreversible pulpitis. Irreversible pulpitis is a localised inflammatory event, so maxillary teeth usually anaesthetised by local infiltration were selected in the present study to test the hypothesis [7].
NSAIDs are chosen in the current study as they are a part of regularly prescribed drug regimen in dentistry. NSAIDs act as inhibitors of the enzyme cyclooxygenase (COX) nonselectively, inhibiting both the cyclooxygenase-1 (COX-1) and cyclooxygenase-2 (COX-2) isoenzymes. COX catalyses the formation of prostaglandins and thromboxane from arachidonic acid. The advantage of selecting these drugs is that they can be administered orally; they are highly bound to plasma proteins and have less chances for displacement reactions. They have high margin of safety with regard to dosage, have ease of accessibility, and have minimal potential for drug abuse [11].
IBUP is a propionic acid derivative. Modaresi J et al., in 2006 concluded that preoperative administration of IBUP, if not contraindicated, is a drug of choice 1 hour prior to local anaesthesia injection to enable deep anaesthesia during RCT of teeth with irreversible pulpitis [12].
PARA (acetaminophen; N-acetyl-p-aminophenol) is an acetanilide derivative. It is a most commonly used drug and has an excellent safety record. Acetaminophen’s mechanism of action points to multisite activity peripherally by involving inhibition of prostaglandin synthesis, and in the central nervous system by interaction with both cannabinoid and serotoninergic pathways [13]. Diclofenac potassium, which is a benzoic acid derivative is a potent NSAID. Diclofenac can affect arachidonic acid release and uptake by inhibition of thromboxane-prostanoid receptor, Gan TJ in his research suggested that additional novel mechanisms of actions may include the inhibition of substrate P, inhibition of peroxisome proliferator activated receptor gamma (PPARgamma), blockage of acid-sensing ion channels. This diversity in diclofenac’s mechanisms of actions has potential for a relatively more favourable profile compared with other NSAIDs [14].
Atasoy Ulusoy Öİ and Alaçam T evaluated the efficacy of single buccal infiltrations for maxillary first molars in patients with irreversible pulpitis in a randomised controlled clinical trial and found that single buccal infiltration is insufficient for adequate pulpal anaesthesia in the palatal root canal of the maxillary first molars associated with irreversible pulpitis [15]. So to eliminate the procedural error in the current study both buccal and palatal infiltration were utilised.
IBUP 400 mg (Group B) showed a 65% success rate and 35% failure rate. During the treatment, 17.5% of the patients had no pain, 47.5% of the patients had mild pain corresponding to the 65% success rate and 9.17% of the patients had moderate pain, 25.83% had severe pain corresponding to the 35% failure rate. Statistical analysis with respect to pain score on heft parker scale by Tukeys multiple post-hoc procedures showed significant difference (p=0.0001) between the preoperative pain and on pulp extirpation within the group. The results obtained with IBUP in this study are consistent but in slight difference with the results obtained by Parirokh M et al., and Noguera-Gonzalez D et al., [4,16]. The slight difference can be attributed to their different study design where they tested the success of Inferior Alveolar Nerve Block (IANB). Ianiro SR et al., reported a success rate of 75.9%, but for the combination of acetaminophen and IBUP group. The higher success rate may be attributed to the combination of the drugs as acetaminophen have additional activity [17]. Ramachandran A et al., reported a success rate of 93.3% with IBUP but they used 800 mg dose in their study [7].
This study aimed at evaluating the effectiveness of premedication with NSAIDs in maxillary infiltration anaesthesia where the local anaesthesia administered is directed to periapical area of the tooth with irreversible pulpitis is required. Furthermore, the results obtained from other studies have been tabulated in [Table/Fig-5,6 and 7] [4,6,7,16-19].
| Drugs | Technique | Authors | Success % |
|---|
| Ibuprofen | IANB | Parirokh M et al., [4] | 78% |
| Aggarwal V et al., [6] | 27% |
| Noguera-Gonzalez D et al., [16] | 72% |
| Shahi S et al., [18] | 25.4% |
| Jena A, and Shashirekha G [19] | 50% |
| Infiltration | Ramachandran A et al., [7] | 93.3% |
| Current study | 65 |
| Ketorolac | IANB | Jena A, and Shashirekha G [19] | 70% |
| Aggarwal V et al., [6] | 39% |
| Acetminophen | IANB | Ianiro SR et al., [17] | 71.4% |
| Infiltration | Ramachandran A et al., [7] | 73.3% |
| Current study | 58.3% |
| Aceclofenac | Infiltration | Ramachandran A et al., [7] | 90% |
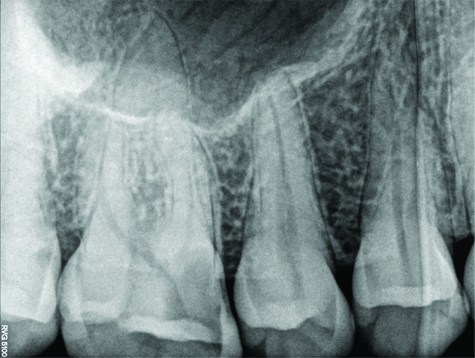
Radiographic representation of teeth with irreversible pulpitis.
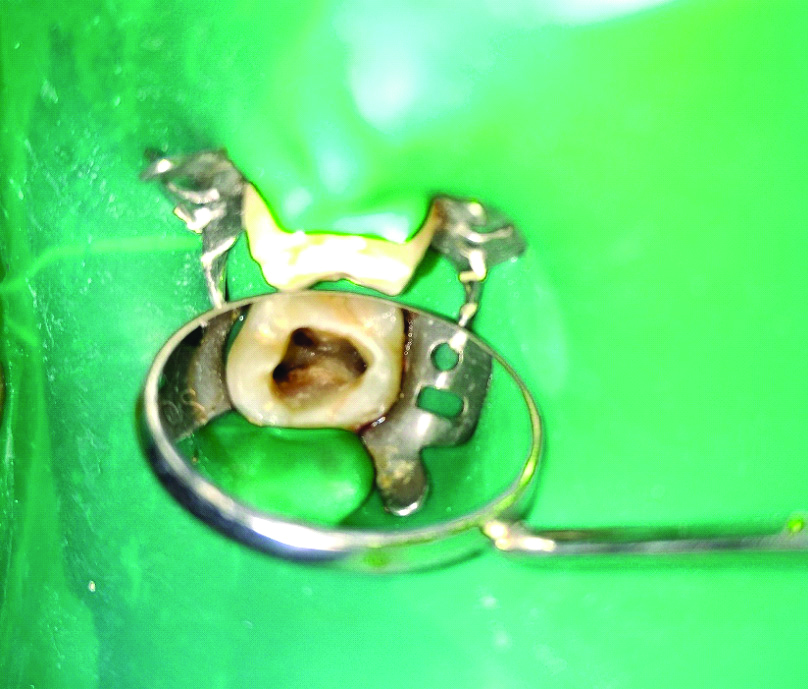
Pictorial representation of maxillary molar access opening.
DS 50 mg (Group C) showed a 60.83% success rate and 39.17% failure rate. During the treatment 8.33% of the patients had no pain, 52.50% of the patients had mild pain corresponding to the 60.83% success rate and 9.17% of the patients had moderate pain, 30.00% had severe pain corresponding to the 39.17% failure rate. Statistical analysis with respect to pain score on heft parker scale by Tukey’s multiple post-hoc procedures showed significant difference (p=0.0001) between the preoperative pain and on pulp extirpation within the group. The results obtained with IBUP in this study are consistent with the results obtained by Prasanna N et al., [20].
PARA 500 mg (Group D) showed a 58.33% success rate and 41.67% failure rate. During the treatment 10.00% of the patients had no pain, 48.33% of the patients had mild pain corresponding to the 58.33% success rate and 7.50% of the patients had moderate pain, 34.17% had severe pain corresponding to the 41.67% failure rate. Statistical analysis with respect to pain score on heft parker scale by Tukey’s multiple post-hoc procedures showed significant difference (p=0.0001) between the preoperative pain and on pulp extirpation within the group. Ramachandran A et al., in a similar study design has reported a success rate of 73.3% with 1000 mg dose in their study [7]. The higher success rate might be due to the higher dose in this study.
The inter-group comparison of pain score during pulp extirpation showed that there is statistically significant difference when the placebo group is compared with IBUP (p=0.0004), DS (p=0.0013) and PARA (p=0.0201) groups. This parameter is of particular importance because in irreversible pulpitis, the maximum pain is experienced while extirpating the pulp as the nerve fibres are in direct contact with the endodontic instrument.
Among all the experimental groups, the subjects experienced maximum pain while extirpating the pulp, followed by when the bur enters the pulp chamber and least pain was experienced by the patients when the bur is in dentin.
When the bur is in dentin, least pain was experienced by the subjects of IBUP group, followed by diclofenac group, PARA group and maximum pain was experienced by placebo group. The order was the same when the bur enters pulp chamber and on pulp extirpation.
The IBUP and diclofenac group demonstrated better analgesic effect than the PARA group. This could be because IBUP and DS drugs inhibit COX-2 enzyme which plays a major role in inflammation. As PARA has a weak analgesic/anti-inflammatory effect and a strong antipyretic effect, Also, its analgesic activity mechanisms are located in the CNS. However, further research is needed in this direction. A further clinical trial with a larger sample size would strengthen the results of the present study.
Limitation(s)
The readings obtained on visual analog scale completely depend on the patient’s pain threshold and also psychological factors can play a role on the the outcome.
Conclusion(s)
It is imperative to interpret that premedication with Ibuprofen 400 mg, Paracetamol 500 mg or Diclofenac Sodium 50 mg have positive effect on the outcome of maxillary infiltration anaesthesia in patients with irreversible pulpitis. Even after determining the success of anaesthesia by electric pulp test in methodology of current study, the varied results may be due to difference in the depth of anaesthesia. Author’s tried to associate the depth of anaesthesia during endodontic procedure with premedication. Though, local anaesthesia has been a boon to dentistry, Author’s opinion is that there is always a room for improvement, premedication is one of the prospects to improve the depth of anaesthesia during endodontic therapy.
*denote significant p-value