Subungual Melanoma- An Enigmatic Entity
Madhusmita Jena1, Rajeswari Bhat2
1 Professor and Head, Department of Pathology, East Point College of Medical Sciences and Research Centre, Bengaluru, Karnataka, India.
2 Assistant Professor, Department of Dermatology, East Point College of Medical Sciences and Research Centre, Bengaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Madhusmita Jena, Block 11, Flat C4, Krishna Nagar Apartment, Annasandrapalya. HAL: Post Bengaluru: 17, Karnataka, India.
E-mail: jenadrmadhusmita@gmail.com
Hutchinson’s sign, Nail matrix, Trauma
Dear Editor,
Subungual melanoma is a rare variant of melanomas that originates from the nail matrix accounting for 1.5-2.5% of all melanomas [1]. These melanomas get misdiagnosed as pyogenic granuloma or onychomycosis clinically [1,2]. The role of recurrent trauma in the progression of the lesion has been described; but its role in the pathogenesis of acral melanomas is not clear as many a times, the injury draws the attention of the lesion [3]. The history of recurrent injury and clinical presentation is often misleading resulting in delayed diagnosis and treatment [3].
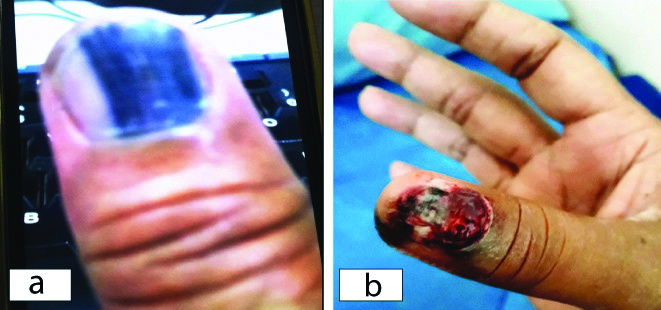
A 61-year-old male, stenographer by profession presented with chief complaint of a painful reddish mass in the nail matrix of the right thumb, associated with bleeding following a history of repeated trauma of three months with loosening of nail plate from the nail bed and a slowly growing mass with a increased tendency to bleed. The patient gave the history of a linear brown to blackish discolouration of the nail plate eight years back which was stored in his mobile camera [Table/Fig-1a]. The patient had been treated with antifungals and antibiotics for a long time on a clinical suspicion of Onychomycosis after eight years of the blackish discolouration of the nail, the patient presented with a fleshy reddish irregular mass measuring about 1 × 0.9 cm along with blackish pigmentation of the nail bed and tip of right thumb (Hutchinson’s sign). The mass was friable and was bleeding easily on touch [Table/Fig-1b]. A surgical removal of the nail plate was done at our institute and a small biopsy from the mass was taken.
a): Blackish linear discolouration of nail (clinical image of year 2011); b): Patient presenting with friable mass from the nail matrix with blackish discolouration extending to distal tip of thumb.
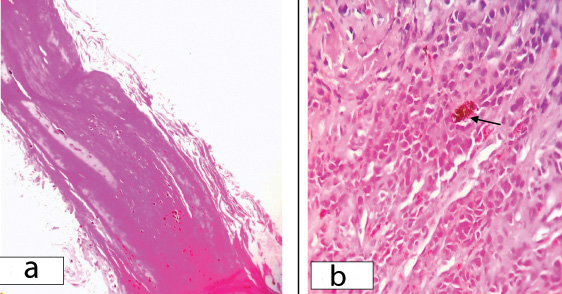
Microscopy showed layers of lamellar keratin and granular squamous epithelium with intracytoplasmic melanin pigments [Table/Fig-2a]. The other tissue fragment was composed of malignant cells arranged in sheets showing mild pleomorphism with hyperchromatic to vesicular nuclei, occasional small prominent eosinophilic nucleoli and moderate cytoplasm. Intracytoplasmic and extracellular melanin pigment was noted [Table/Fig-2b]. Mitotic activity was not seen in the tumor tissue. The Breslow’s thickness could not be assessed as the epidermis was separated out from the tumour tissue. However, the thickness of the tumour in the tissue received was found to be 4 mm. A negative Periodic Acid Schiff (PAS) stain ruled out fungal infection. A Perls stain done on tissue which was negative excluded the haemosiderin pigment from melanin. A melanin bleach was also performed. As both the tests favoured towards melanin pigment in the malignant cells, a diagnosis of melanoma was signed out. There were no enlarged and palpable epitrochlear or axillary lymphnodes. Systemic examination and routine investigations were all normal. Screening for metastasis was negative on radiology like ultrasound and CT scan. The patient was referred to a higher centre where he underwent disarticulation of the interphalangeal joint of the thumb and the melanoma was confirmed on histopathology with margins free of tumour.
a): Lamellar keratin and squamous epithelium showing intracytoplasmic melanin (H&E stain X100); b): Sheets of malignant cells showing pleomorphism with hyperchromatic to vesicular nuclei and intracytoplasmic melanin (H&E stain X400).
The patient had a history of recurrent trauma to his right thumb as he was using it for stenography. The association of trauma with melanoma has been reported in the literature [3]. Also, the patient gave a long history from the time of the blackish linear discolouration till the appearance of a bleeding mass from the nail bed. Inspite of such a long history, there was no evidence of distant metastasis which is quite unusual, unlike other malignant melanomas.
Subungual melanomas are rare and account for 0.7% to 3.5% of all malignant melanomas worldwide. They are more frequent in Asians than whites [4]. The diagnosis of a subungual melanoma needs a stepwise approach of clinical examination, dermoscopic findings and histopathological examination [4,5]. The findings of linear discolouration of the nail plate >5 mm, single nail involvement, periungual pigmentation, enlargement of the pigmented band from distal to proximal end should raise a suspicion of malignancy [3,5].
The poor prognostic factors include elderly age group, ulceration and mitosis. Delay in diagnosis of the lesion can result in a poor prognosis. The five year survival rate ranges from 16% to 87% [1,2,5]. Management is surgical involving amputation of fingers or toes.
Subungual melanoma is extremely rare in Indian population and only a few cases are reported in the Indian literature because the cases are missed in the early stages, but it has to be kept in mind while dealing with pigmentary lesions of the nail unit [2]. What is enigmatic of this entity is getting missed in its early stage and also the absence of local and distant metastasis despite a very long history of eight years as in this case. This case is presented to highlight its rare incidence amongst Indian population and the need for an awareness of this entity to make an early detection.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 06, 2020
Manual Googling: May 18, 2020
iThenticate Software: Jul 22, 2020 (10%)
[1]. Singal A, Pandhi D, Gogoi P, Grover C, Subungual melanoma is not so rare: Report of four cases from IndiaIndian Dermatol Online J 2017 8(6):471-74.10.4103/idoj.IDOJ_411_1629204392 [Google Scholar] [CrossRef] [PubMed]
[2]. Verma R, Kakkar S, Vasudevan B, Rana V, Mitra D, Neema S, A rare case of subungual melanomaIndian J Dermatol 2015 60(2):188-90.10.4103/0019-5154.15252625814711 [Google Scholar] [CrossRef] [PubMed]
[3]. Ghariani N, Boussofara L, Kenani N, Ghannouchi N, Mebazaa A, Denguezli M, Post traumatic amelanotic subungual melanomaDermatol Online J 2008 14(1):13 [Google Scholar]
[4]. Ozdemir F, Errico MA, Yaman B, Karaarslan I, Acral lentiginous melanoma in the Turkish population and a new dermoscopic clue for the diagnosisDermatol Pract Concept 2018 8(2):140-48.10.5826/dpc.0802a1429785333 [Google Scholar] [CrossRef] [PubMed]
[5]. Haneke E, Ungual melanoma- Controversies in diagnosis and treatmentDermatol Ther 2012 25(6):510-24.10.1111/j.1529-8019.2012.01515.x [Google Scholar] [CrossRef]