Chyluria: An Unending Illness- A Case Report
Dwijesh Kumar Panda1
1 Lymphologist and Microbiologist, Department of Pathology and Microbiology, Sanaria Research Center, Bhubaneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dwijesh Kumar Panda, M-5/12, Acharya Vihar, Bhubaneswar-751013, Odisha, India.
E-mail: doctordwijesh@gmail.com
Chyluria is the passage of milky urine due to a lymphourinary fistula. It is secondary to lymphatic stasis caused by obstruction of the lymphatic flow. It is caused by the parasite Wuchereria bancrofti in more than 95% of cases in tropical countries. Chyluria occurs in 2% of filarial-infested patients. When an abnormal connection between intestinal lacteals and the urinary tract develops, chyluria appears. The diagnostic approach is aimed to define the site of lymphourinary fistula. It is a benign disease that can be controlled by medical treatment and dietary restrictions. A small number of patients require surgical intervention. The 45-year-old thin built woman was suffering from chyluria, flank pain in the abdomen, weakness and loss of weight for the last 10 years. The serum test for circulating adult filarial antigen was positive in moderately high titer. Antifilarial treatment was advised. The symptoms improved for three months and again relapsed.
Lymphoscintigraphy, Povidone iodine, Sclerotherapy
Case Report
A 45-year-old thin built woman presented with complaints of milky white urination for the last 8 years. There was report of weakness, loss of weight, mild pain in the flanks and psychologically upset for a long time illness. The patient was a resident of Bhubaneswar, Odisha, India which is an endemic zone of Lymphatic filariasis. The patient consulted one gynaecologist in the year 2010 for treatment of white discharge which mimics chyluria. On microscopical examination of the sediment of the urine, Candida albicans and Trichomonas vaginalis were not detected. Ultrasonography of the abdomen did not reveal any pathology. The family history was suggestive of lymphatic filariasis.
The patient was suffering from type-2 diabetes and undergoing treatment by an endocrinologist with oral hypoglycemic drugs. The patient was taking Glimepiride (1 mg) + Metformin (500 mg) twice daily before food and one tablet Metformin (1000 mg) before dinner. The sugar level was not under control, blood HbA1c level is 8.5%, high serum triglyceride (196 mg/dL), serum protein (6.8 gm/dL) and serum albumin (3.7 gm/dL) were found to be within reference value. The urine examination revealed the presence of protein, sugar (0.5%) and chyle in very high quantity, without red blood cells.
The patient consulted one Urologist in 2014. Her cystoscopy examination was done under local anaesthesia. Urethral stenosis noticed. Chyle mixed urine was present in the urinary bladder. No reflux from both ureteric orifices noticed. Urine culture showed no growth of uro-pathogen after 24 hours of incubation.
The patient was prescribed the following medicines along with liquid potassium citrate and antacid for one month.
Tab. Diethylcarbamazine citrate- one tablet twice daily after food for 14 days.
Tab. Atorvastatin (10 mg)- one tablet once daily for 14 days.
Tab. Dehydroepiandrosterone- 75 mg daily for one month.
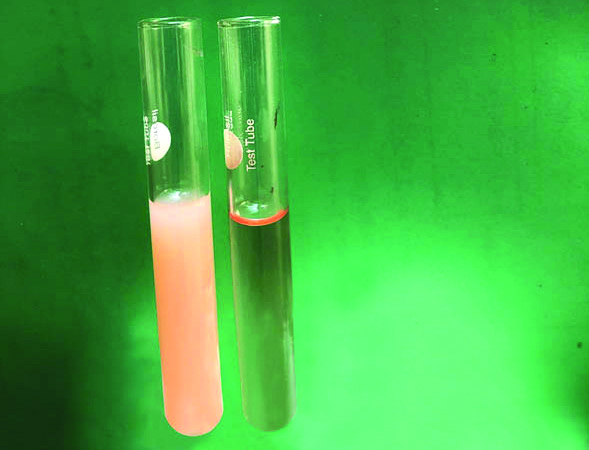
The patient did not get any improvement. Ultimately, she came to the “Sanaria” lymphology clinic for treatment. The patient was informed about medical examination and consent obtained for required procedures. The urine was examined. A copious quantity of chyle was detected. It was cloudy and milky, unctuous clots were present [Table/Fig-1]. Microscopic examination of the sediment revealed fats, few lymphocytes, no red blood cells and the absence of urinary casts. An equal volume of chloroform was added to the urine. After shaking for a few minutes, it was kept standing in the test tube rack. The specimen separates into two layers: milky on the surface and clear below. Sudan III reagent is a saturated solution of the powder in 70% alcohol. Five ml of urine was taken in a test tube and 3 drops of the reagent were added and shaken for a few minutes. It was kept standing for 10 minutes. The upper portion of the normal urine formed a thin red layer above the clear layer below. This is due to the presence of a little quantity of lipoproteins. The chylous urine (left tube) of the patient looks red throughout. It indicated the presence of a high quantity of lipids, triglycerides and lipoproteins in the urine [Table/Fig-2].
Image of chyluria (left) and normal urine (right).
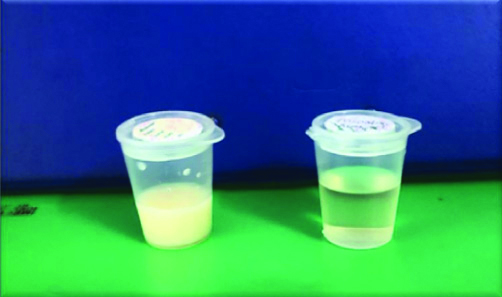
Image of chyluria (left) and normal urine (right) (Sudan III Test).
Serum urea was 18.2 mg/dL and creatinine 0. 7mg/dL. Both the results were within reference value. Kidney function was normal. The haemogram showed eosinophilia of 18%.
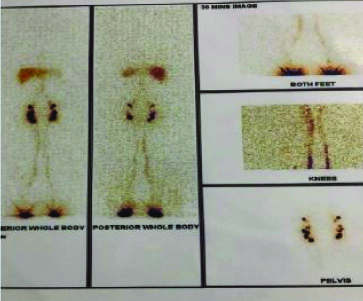
Lymphoscintigraphy was done after intradermal injection of 2 mCi of Tc-99m-S-colloid in the first interdigital space of both feet. Images of lower legs, knee region and inguinal area were taken after 15 minutes and 60 minutes. The images indicated the persistence of tracer uptake in both superficial and deep lymphatics and bilateral ilioinguinal nodes [Table/Fig-3]. The whole-body scan at 60 minutes showed an increased number of ilioinguinal lymph nodes along with visualisation of liver indicative of no deep lymphatic system obstruction.
Lymphoscintigraphy image.
Immunological Examination
Adult filarial circulating antigen detection in the serum was done with ELISA (Og4C3) test. It detected the presence of the monoclonal somatic antigen of the Wuchereria bancrofti. The test became positive in serum i.e., 256 Antigen Units (AU). The reference value is below 128 units. The urine test was done by Immuno Chromatographic Technique (ICT) qualitative method which confirmed the presence of the parasitic antigen.
Treatment
Conservative treatment
The patient was treated with dietary restriction and drugs. The long-chain triglycerides were strictly avoided. Only medium-chain triglycerides were advised. It contains less than 12 carbon atoms and is recommended instead of normal lipids. This is directly absorbed from the gut and transported to the liver via the portal vein, bypassing the lymphatics. The use of coconut oil, which contains medium-chain triglycerides was strongly advised to use. As the commonly used cooking medium in northern India is ghee and mustard oil which contributes to chyluria was completely abandoned. Ghee is the worst offender. To prevent secondary infection, the drugs prescribed were albendazole for two weeks (400-800 mg/day), benzathine penicillin for 12 weeks (1.2 million units weekly), diethylcarbamazine for 21 days (6 mg/kg/day) and ivermectin (6-12 mg stat, repeated after 3 weeks). A combination of drugs was used in this case. The patient was advised to take rest and use abdominal binders. Three courses of drug therapy were given to the patient. Conservative management showed success.
Endoscopic Sclerotherapy (EST)
The recurrence of chyluria occurred after six months. So, the patient was advised to consult urosurgeon for sclerotherapy. The procedure was performed under local anaesthesia. The patient was advised a fatty meal in the previous night to facilitate the identification of the affected ureteric orifice. A ureteric catheter was inserted to the renal pelvis under radiological control and an amount of 7-10 mL povidone-iodine (0.2-5%) was injected. An 8-hourly instillation for three days was given. Chyluria gradually disappeared for three months and again reappeared. The patient continued to be monitored at SANARIA research center, Bhubaneswar, Odisha, India. Detailed report of the patient is presented in [Table/Fig-4].
Different manifestation of chylous urine.
| Patient’s detail investigations | Chylous urine of the patient presented | Chylous urine of a patient suffering from Haemato-Chyluria | Chylous urine of a patient suffering from Nephrotic syndrome | Chylous urine of a lady suffering from Vaginal Candidiasis |
|---|
| Patient’s history | The passing of white turbid urine since last 10 years, weakness, flank pain, afebrile, weight loss | Loss of weight, weakness, Pinkish-white turbid urine, pain while passing urine and pain in the loin | Passing of white turbid, foamy urine, swelling around the eyes and ankles, weight gain | Urine mixed with thick- white vaginal discharge, itching, vaginal sore |
| Laboratory investigations | All biochemical tests-Normal. High quantity Chyle present in the urine. Red blood cells absent in the urine | All biochemical tests- Normal. Haematuria and ‘Chyluria | High lipoproteins in the urine, elevated lipids, urea and creatinine in the serum | Detection of Candida albicans in the wet vaginal smear |
| Hematological findings | High eosinophil count | High eosinophil count | Low haemoglobin | Normal |
| Immunological findings | W.bancrofti antigen test-Positive | W. bancrofti antigen test- Positive | Immuno-fluorescent antibody test- Positive | Unavailable |
| Diagnosis | Lymphatic filariasis | Lymphatic filariasis/Kidney stone | Nephrotic Syndrome | Vaginal Moniliasis |
| Treatment | Diet, Drugs and SclerotherapyLympho-Venous disconnection at the renal hilum | Diet, Drugs and SclerotherapyShockwave, Stone removal, and laser lithotripsy for stone | Diet and Medications | Nystatin cream and Tablet |
| Follow-up | Recurrence | Recurrence/Cure | Dialysis | Cured |
Discussion
Lymphatic filariasis is endemic in India (WHO bulletin- 2010-2015) [1]. The great Indian sage Charak described it as ‘Suklameha’ in 300 BC (Charak Samhita Volume 1). The incidence of filarial parasite infestation in tropical countries due to Wuchereria bancrofti is more than 95% [2,3]. Chyluria occurs among 2% of bancroftian filarial patients [4]. The pathophysiology is due to obstruction or dilation of the retroperitoneal lymphatics [5]. Urine examination showed the presence of chylomicrons and triglycerides. Detection of chylomicrons in the urine is the most sensitive test for chyluria [6]. Sudan III is a red fat-soluble dye which reacts with the lipids to stain red. The oil in the urine forms a red layer above the water in the test tube [7]. The serum test for the detection of circulating adult filarial monoclonal antigen (Og4C3) became positive in moderate titer. The test is positive in Bancroftian. filariasis. It is a quantitative assessment of the parasitic antigen (ELISA) in human lymphatic filariasis. It is highly sensitive and specific in the diagnosis of the disease [8].
Lymphoscintigraphy is a safe and non-invasive technique to visualise structural and functional changes in lymphatic flow after the injection of the radiotracer. There is no evidence of obstruction of lymphatic flow in the lower extremity. Iliac, para-aortic and bilateral inguinal lymph nodes are well visualised. The liver shows normal tracer activity. This indicates that there is no obstruction of lymphatic flow. In this case, the outdated lymphangiography is the best diagnostic tool [9]. The medium-chain triglycerides are strongly advised to use. It is directly transported to the liver via portal vein bypassing the lymphatics and reduces the excretion of lipids in the urine [10]. Triple-drug therapy helps the elimination of lymphatic filariasis [11]. Sclerotherapy is done when the patient fails to respond to conservative therapy. It is observed that the lymphourinary fistula is mostly located at the renal pelvis. The renal calyceal fornix is the most frequent site of lymphourinary fistula. The injection of sclerosant gives relief to the patient when the leaking lymphatics heal by fibrosis [12,13]. Surgical treatment is considered when two or three courses of sclerosing therapy fail. Chylolymphatic disconnection is the most commonly performed procedure [14].
Conclusion(s)
Chyluria caused by lymphatic filariasis is a benign disease. This can be effectively treated by drugs and dietary restrictions. The success rate is more than 70%. A small number of patients having severe chyluria may require surgical intervention. Since spontaneous remissions are frequent and other invasive therapeutic options carry the risk of severe complications; conservative management is recommended.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 03, 2020
Manual Googling: Jun 29, 2020
iThenticate Software: Jul 13, 2020 (19%)
[1]. Preventive Chemotherapy and Transmission Control (PCT) Department of Control of Neglected Tropical Diseases (NTD) World Health Organization 20, Avenue Appia 1211 Geneva 27, Switzerland http://www.who,int/neglected_diseases/en [Google Scholar]
[2]. Agrawal VK, Sashindran VK, Lymphatic filariasis in India: Problems, challenges and new initiativesMed J Armed Forces India 2006 62(4):359-62.10.1016/S0377-1237(06)80109-7 [Google Scholar] [CrossRef]
[3]. Taylor MG, Hoerauf A, Bockarie M, Lymphatic filariasis and onchocerciasisLancet 2010 376:1175-85.10.1016/S0140-6736(10)60586-7 [Google Scholar] [CrossRef]
[4]. Sharma S, Hemal AK, Chyluria- An overviewInt J Nephrol Urol 2009 1:14-26. [Google Scholar]
[5]. Ansari MS, Medical treatment of filariasis and chyluriaIndian Journal Urol 2005 21:24-26.10.4103/0970-1591.19546 [Google Scholar] [CrossRef]
[6]. Okamoto K, Ohi Y, Recent distribution and treatment of filarial chyluria in JapanJ Urol 1983 129(l):64-67.10.1016/S0022-5347(17)51921-7 [Google Scholar] [CrossRef]
[7]. Refat NA, Ibrahim ZS, Moustafa GG, Sakamoto KQ, Ishizuka M, Fujita S, The induction of cytochrome P450 1A1 by Sudan dyesJ Biochem Mol Toxicol 2008 22(2):77-84.10.1002/jbt.2022018418879 [Google Scholar] [CrossRef] [PubMed]
[8]. Panda DK, Panda Mohapatra DP, Mohapatra MM, Breast filariasis or inflammatory breast carcinoma? Reaching a diagnosisBMJ Case Rep 2015 10.1136/bcr-2015-21225426567240 [Google Scholar] [CrossRef] [PubMed]
[9]. Freedman DO, de Almeida Filho PJ, Besh S, Maia e Silva MC, Braga C, Maciel A, Lymphoscintigraphic analysis of lymphatic abnormalities in symptomatic and asymptomatic human filariasisJ Infect Dis 1994 170:92710.1093/infdis/170.4.9277523538 [Google Scholar] [CrossRef] [PubMed]
[10]. Singh LK, Datta B, Dwivedi US, Singh PB, Dietary fats and chyluriaIndian J Urol 2005 21:50-54.10.4103/0970-1591.19552 [Google Scholar] [CrossRef]
[11]. Fischer PU, King CL, Jacobson JA, Weil GJ, Potential value of triple drug therapy with Ivermectin, Diethylcarbamazine, and Albendazole (IDA) to accelerate elimination of lymphatic filariasis and onchocerciasis in AfricaPLoS Negl Trop Dis 2017 11:e00051630.1371/journal.pntd.000516328056015 [Google Scholar] [CrossRef] [PubMed]
[12]. Singh KJ, Srivastava A, Nonsurgical management of chyluria (sclerotherapy)Indian J Urol 2005 21:55-58.10.4103/0970-1591.19553 [Google Scholar] [CrossRef]
[13]. Shanmugam TV, Prakash JV, Sivashankar G, Povidone-iodine used as a sclerosing agent in the treatment of chyluriaBr J Urol 1998 8210.1046/j.1464-410X.1998.00861.x9806194 [Google Scholar] [CrossRef] [PubMed]
[14]. Maol L, Li W, Lu M, Cheng H, Wen R, Chen J, Surgical treatment of intractable chyluriaInt J Clin Exp Med 2016 9(5):8230-35. [Google Scholar]