Haematological abnormalities are commonly seen in patients with thyroid disorder with anaemia being the most common abnormality. It has been defined in 20-60% of patients with hypothyroidism [1]. Anaemia is often the first sign of hypothyroidism [1]. Through erythropoietin, thyroid hormones stimulate the growth of erythroid colonies both by direct and indirect method. Hypothyroidism can cause a wide variety of anaemic disorders. Morphologically, anaemias can be normocytic, microcytic or macrocytic and in pathogenesis of these anaemias, various mechanisms has been involved. Normocytic normochromic anaemia has been found to be the most common form of anaemia in hypothyroidism [2,3].
Pregnancy is frequently associated with anaemia, most commonly iron deficiency anaemia, followed by dimorphic anaemia [4]. Iron deficiency anaemia is associated with a higher risk of pre-term delivery, low birth weight and perinatal death. Pregnancy complicated by the development of hypothyroidism could be further associated with a higher incidence of anaemia. The WHO definition for diagnosis of anaemia in pregnancy is Hb concentration of less than 11 g/dl [5]. Anaemia may be classified as mild 10-11 g/dL, moderate 7-10 g/dL, severe <7 g/dL and very severe <4 g/dL [6].
Various adverse effect of overt hypothyroidism in pregnancy has been reported. These adverse effects include rise in number of anaemia, low birth weight, premature birth, neonatal respiratory distress and intra-uterine fetal death. In addition to these, increase in prevalence of pre-eclampsia was also reported. Pregnancy induced hypertension, abortion, placental abruption and post-partum haemorrhage has also been reported in pregnant hypothyroid patients [7]. Serum TSH level is used as single most sensitive test to reliably detect abnormalities of thyroid function [8]. Studies have used TSH cut-offs of 4.5 mIU/l to look at prevalence of hypothyroidism in the first trimester of pregnancy [9,10]. However, TSH levels during pregnancy are lower as compared to TSH levels in a non-pregnant state. So, lower cut-offs have been suggested by many study groups to avoid missing cases, and hence to prevent the associated maternal and fetal complications [11]. Clinical practice guidelines for hypothyroidism in adults, co-sponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association have recommended trimester specific reference levels for TSH in pregnancy as follows: 1st trimester: 0.1-2.5 mIU/l, 2nd trimester: 0.2-3 mIU/l, 3rd trimester: 0.3-3 mIU/l [8,12]. Keeping in view the various adverse effects of hypothyroidism in pregnancy, this study was conducted with the aim to determine the incidence and characteristics of anaemia in pregnancy associated with hypothyroidism.
Materials and Methods
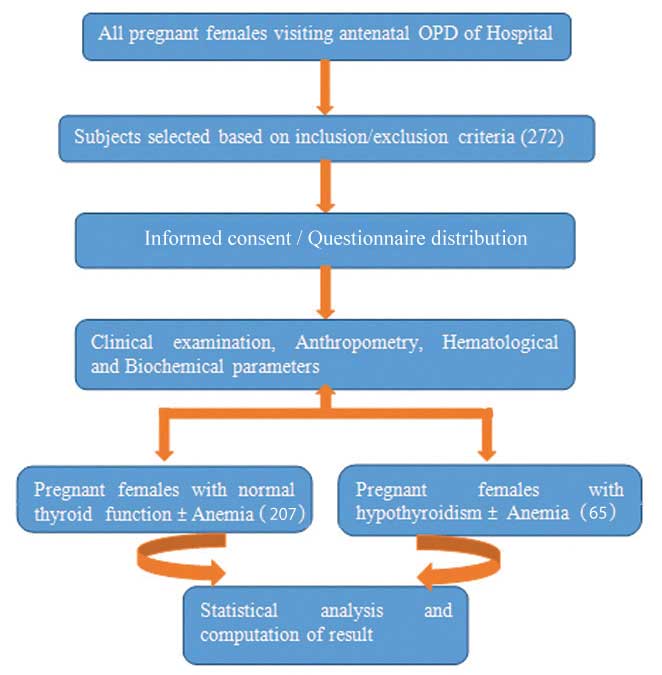
This study was a case-control study conducted in School of Medical Sciences and Research (SMS&R), Sharda University, Greater Noida, Uttar Pradesh during January 2015 to January 2016. A prior approval of Institutional Ethical Committee (Ref. No. SU/SMS&R/76-A/2020/12) was taken. Flow chart of study design is shown in [Table/Fig-1].
Flow chart of study design.
The sample size was calculated by using formula:
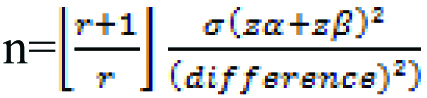
n=sample size, r=ratio of control to cases, Zα=level of significance (1.96), Zβ=desirable power (80%), Difference=2.34, s=standard deviation
By using above mentioned formula, minimum sample size required for the study was 272 and we enroll 272 pregnant women in this study.
Inclusion criteria: All pregnant females in the age group of 18-40 years who attended the antenatal OPD were included in this study.
Exclusion criteria: All pre-diagnosed cases of thyroid disorder or patients with a family history of hypothyroidism or known cases of anaemia, currently on treatment were excluded from the study. Subjects with any history of smoking and addiction and patients on treatment for any chronic disease, like diabetes were also excluded from the study.
Written informed consent was then taken from all subjects before the start of the study. Anthropometric measurements (height and weight) were noted using a stainless steel stadiometer (IndoSurgicals Pvt., Ltd., New Delhi) and digital weighing machine (Omron Healthcare Co., Ltd., Japan). Gestational age was confirmed by Ultrasonography (Samsung, South Korea). Following an overnight fast, blood sample was collected in the morning from each subject. The concentration of TSH was measured by an electrochemiluminescence immunoassay diagnostic kit (Johnson & Johnson, USA). Complete Blood count was done by using an automated 6 part haematology analyser XN-1000i (Sysmex Corporation, Kobe, Japan). Peripheral blood smear was stained by Leishman stain and subsequently studied under microscope for morphological classification of anaemia [13]. Pregnant woman was considered to be hypothyroid, if TSH was ≥2.5 mIU/L in the first trimester and the others were considered to be euthyroid. In the second and third trimester, a TSH cut-off of 3 mIU/L was used [12]. Patients were classified as Euthyroid or Hypothyroid based on TSH levels. Patients were categorised as anaemic or non-anaemic based on a Hb level cut-off of 11 gm/dL [6]. Anaemia was further classified according to the Hb level into mild, moderate and severe anaemia [6]. Anaemia was further characterised based on morphology into normocytic normochromic, microcytic hypochromic, macrocytic or dimorphic and percentages were calculated in the euthyroid and hypothyroid groups.
Statistical Analysis
All statistical analysis was done using Microsoft excel and SPSS software (Version 24). Mean Body Mass Index (BMI) of euthyroid and hypothyroid groups was compared using unpaired t-test. Pearson’s correlation test was used to determine any correlation of BMI with TSH levels in the hypothyroid group. Unpaired t-test was done to see level of significance of Hb in euthyroid and hypothyroid subjects. Chi-square test was used to calculate the association between hypothyroidism and anaemia. TSH levels of anaemic subjects were compared with those of non-anaemic subjects using unpaired t-test. Mean values for Mean Corpuscular Volume (MCV), Mean Corpuscular Haemoglobin (MCH) and Mean Corpuscular Haemoglobin Concentration (MCHC) were computed. Unpaired t-test was done to see any significant difference in the mean values in euthyroid and hypothyroid groups. Percentage of anaemia in euthyroid and hypothyroid subjects was calculated and were compared with p<0.05 as level of significance.
Results
The incidence of anaemia in present study was 92.31% in hypothyroid patients (60/65 cases), while 63.28% (131 out of 207) of euthyroid patients were anaemic. Overall, 70.22% (191/272) of all pregnant females were found to be anaemic. Out of 272 subjects, 71 subjects were from the first trimester, 98 were from second trimester and 103 were from the third trimester.
Out of a total of 272 subjects, 207 were euthyroid, using a TSH cut-off of 2.5 mIU/L. 65 subjects were hypothyroid. The mean age of euthyroid subjects were 23.12 years (22.73-23.50) while that of hypothyroid subjects were 24.57 years (23.77-25.38). Of the 65 hypothyroid subjects, 19 were in the first trimester, 25 in the second trimester and 21 were in the third trimester. The mean TSH of euthyroid group was 2.49±1.35 mIU/L and hypothyroid group was 6.27±3.6 mIU/L.
Mean Hb of Euthyroid was 10.16 g/dL (CI 0.195-0.258) while mean Hb of hypothyroid subjects was 8.92 g/dL (CI 0.355-0.457). Mean Hb of Euthyroid was significantly different from mean Hb of hypothyroid subjects (p-value 0.0001) However, no significant difference was found in MCV, MCH and MCHC of the two groups [Table/Fig-2].
Comparison of various parameters in Euthyroid and Hypothyroid pregnant women and their level of significance.
| Parameters | Euthyroid Mean (95% CI) | Hypothyroid Mean (95% CI) | p-value |
|---|
| BMI (kg/m2) | 23.51 (20.88-26.14) | 24.58 (23.11-26.05) | >0.05 |
| TSH (μIU/mL) | 2.49 (1.14-3.84) | 6.27 (2.67-9.87) | <0.0001 |
| Hb (g/dL) | 10.16 (0.195-0.258) | 8.92 (0.355-0.457) | 0.0001 |
| MCV (fl) | 83.20 (82.43-83.97) | 82.06 (80.37-83.76) | >0.05 |
| MCH (pg) | 28.55 (28.16-28.96) | 28.19 (27.43-28.94) | >0.05 |
| MCHC (g/dL) | 32.07 (31.76-32.38) | 31.21 (30.63-31.79) | >0.05 |
Out of 272 pregnant subject, 191 (70.22%) subjects were found to be anaemic. A 63.28% (131 out of 207) of euthyroid patients were anaemic (Hb <11 gm/dL), while 92.31% (60 out of 65) of hypothyroid patients showed anaemia. A significant association was found between Hypothyroidism and anaemia p-value <0.0001. The mean TSH value of anaemic patients was 3.98±1.02 mIU/L while that of non-anaemic was 2.65±0.98 mIU/L. TSH levels in anaemic patients were significantly higher as compared to non-anaemic patients (p<0.0001) [Table/Fig-3]. No significant association was found between Hb and TSH level in the hypothyroid group (p>0.05).
Comparison of various parameters in anaemic and non-anaemic pregnant women and their level of significance.
| Parameters | Anaemic subjects | Non-anaemic subjects | p-value |
|---|
| Euthyroid | 131 (63.28%) | 76 (36.72) | >0.05 |
| Hypothyroid | 60 (92.31%) | 05 (7.69%) | <0.0001 |
| Mean TSH | 3.98±1.02 mIU/L | 2.65±0.98 mIU/L | <0.0001 |
The majority of anaemia cases in both euthyroid and hypothyroid groups were found to be of moderate severity [Table/Fig-4]. Anaemia of moderate severity was also most commonly seen in all the three trimesters of pregnancy [Table/Fig-5]. Dimorphic anaemia was the most common type of anaemia seen in both euthyroid and hypothyroid subjects [Table/Fig-6]. It was also the most common type of anaemia in all three trimesters [Table/Fig-7]. Of moderate anaemia, 26 (54%) cases were of the dimorphic type in the hypothyroid group and 59 (71.9%) cases were in the euthyroid group.
Characterisation of anaemia in Euthyroid and hypothyroid pregnant women.
| Type of anaemia (Hb) | Euthyroid (%) | Hypothyroid (%) |
|---|
| Mild (10-11 g/dL) | 48 (36.65%) | 5 (8.34%) |
| Moderate (7-10 g/dL) | 82 (62.59%) | 48 (80%) |
| Severe (<7 g/dL) | 1 (0.76%) | 7 (11.66%) |
| Total | 131 (100%) | 60 (100%) |
Trimester wise frequency of severity of anaemia in euthyroid and hypothyroid pregnant women.
| Stage of pregnancy | Euthyroid patients | Hypothyroid patients |
|---|
| Mild anaemia | Moderate anaemia | Severe anaemia | Mild anaemia | Moderate anaemia | Severe anaemia |
|---|
| 1st trimester | 15 | 37 | 00 | 03 | 12 | 02 |
| 2nd trimester | 25 | 36 | 00 | 02 | 19 | 03 |
| 3rd trimester | 08 | 09 | 01 | 00 | 17 | 02 |
| Total | 48 | 82 | 01 | 05 | 48 | 07 |
Distribution of morphological type of anaemia in Euthyroid and Hypothyroid pregnant women.
| Type of anaemia | Euthyroid (%) | Hypothyroid (%) |
|---|
| Dimorphic | 87 (66.5%) | 40 (66.7%) |
| Microcytic hypochromic | 39 (29.7%) | 17 (28.3%) |
| Macrocytic | 5 (3.8%) | 3 (5%) |
| Total | 131 (100%) | 60 (100%) |
Trimester wise morphology of anaemia in Euthyroid and Hypothyroid pregnant women.
| Stage of pregnancy | Euthyroid patients | Hypothyroid patients |
|---|
| Dimorphic anaemia | Microcytic hypochromic anaemia | Macrocytic anaemia | Dimorphic anaemia | Microcytic hypochromic anaemia | Macrocytic anaemia |
|---|
| 1st trimester | 38 | 13 | 01 | 11 | 06 | 00 |
| 2nd trimester | 39 | 20 | 02 | 17 | 06 | 01 |
| 3rd trimester | 10 | 06 | 02 | 12 | 05 | 02 |
| Total | 87 | 39 | 05 | 40 | 17 | 03 |
Discussion
The prevalence of hypothyroidism among pregnant women in the present study was 24%. Prevalence of hypothyroidism in pregnancy has been reported at 14.3% in North India [9]. This is lower than what we found (24%), possibly due to the higher cut-offs (4.5 mIU) used in Dhanwal Dinesh K’s study [9]. Moreover, they looked at cases only in the first trimester, though we looked for the development of hypothyroidism in all three trimesters as shown in [Table/Fig-5,7]. We found the maximum number of cases of hypothyroidism in the second trimester followed by the third trimester and least in the first trimester. It is possible that these differences were due to differences in iodine levels in the population. However, both the studies did not determine the iodine sufficiency in the population. Moreover, a prevalence of 18% was reported by Nidhi J et al., in an urban set-up in South India, despite iodine sufficiency, using similar TSH cut-offs in pregnant women ≤14 weeks [14]. However, higher prevalence rate of 31.81% was reported by Agrawal U et al., from central India [15]. A recent study found 13.13% of pregnant women to be hypothyroid, keeping upper normal limit of TSH <4.5 mIU/L. However, by using American Thyroid Association (ATA) trimester specific TSH cut-offs, they reported 44.3% women to have hypothyroidism in 1st trimester, 32% in 2nd trimester and 34% in 3rd trimester [9]. Various factors seem to be responsible for these discrepancies in prevalence rates of hypothyroidism in pregnancy ranging from iodine deficiency, different TSH cut-offs and geographical or dietary differences.
Early maternal thyroid insufficiency, even Subclinical Hypothyroidism (SCH) and isolated hypothyroxinemia have the potential to impair fetal neurodevelopment. Studies reported that screening for high risk cases only with higher TSH cut-off level of 4.5 mIU/L would miss 81.6% of cases with hypothyroidism [16]. Bijay V et al., reports a lower figure, at missing 1/3rd of cases [17]. Similarly, in the present study we calculated that we would miss 24% cases if we used a higher cut-off of 4.5 mIU/L. Based on the high prevalence of hypothyroidism in pregnancy in this population, we feel a need for universal screening of all pregnant women for hypothyroidism.
The most common type of anaemia in pregnancy is iron deficiency anaemia. Iron deficiency anaemia is associated with a higher risk of pre-term delivery, of low birth weight and perinatal death. Ivan EA and Mangaiarkkarasi A reported that in pregnancy, the most common anaemia is of the iron deficiency type, followed by dimorphic anaemia [4]. Physiological anaemia of pregnancy is usually mild, but moderate to severe anaemia is usually of iron deficiency type [5]. In the present study, we found most cases of moderate anaemia in the hypothyroid group to be of the dimorphic type. In the euthyroid group also, most cases of moderate anaemia were also of the dimorphic type.
The most common type of anaemia in hypothyroidism has been found to be normocytic normochromic anaemia, followed by microcytic hypochromic anaemia of the iron deficiency type [18]. Sharma JB and Shankar M found that Iron Deficiency Anaemia is the most common type of anaemia in pregnancy [5].
Present study focused on determining the incidence of anaemia in pregnant women who developed hypothyroidism during the course of their pregnancy compared to euthyroid pregnant women. The National Family Health Survey-3 (NFHS-3) reported a prevalence of anaemia in pregnancy as 57.9% and specifically 51.6% in Uttar Pradesh [19]. However, we found a higher prevalence of 70.22%. The incidence of anaemia was higher in the hypothyroid group compared to the euthyroid group, as expected. It was interesting to note that in both the groups, euthyroid and hypothyroid, we found dimorphic anaemia to be the most common type of anaemia. Of the hypothyroid individuals, dimorphic anaemia was also found to be the most common in all trimesters, followed by microcytic anaemia and lastly macrocytic anaemia. We did not find a single case of normocytic normochromic anaemia. Similar to present study, Singh N et al., in their study also reported dimorphic anaemias as the most common type in hypothyroid patients, followed by microcytic anaemia and macrocytic anaemia [20]. We did not find any difference in the type of anaemia in the euthyroid and the hypothyroid groups; hence we cannot attribute present finding of dimorphic anaemia to the thyroid status of the individual. It is possible that nutritional deficiencies due to common dietary habits may account for development of dimorphic anaemia in these pregnant populations.
Limitation(s)
First, we were not able to specify the cause of high prevalence of hypothyroidism in this study population, as we don’t have any data regarding iodine status of the present study group. Hence, we were unable to label iodine deficiency as a cause for hypothyroidism. Secondly, we further did not divide our hypothyroid study group into overt and SCH.
Conclusion(s)
In present study, anaemia was seen in 92.31% cases of pregnant hypothyroid patients and 63.28% cases of pregnant euthyroid patients. Thus, based on high incidence of anaemia in both hypothyroid and euthyroid pregnant women, it is recommended to do compulsory routine screening of all pregnant women for thyroid disease so that anaemia can be detected and treated early in the course of pregnancy. This will lead to prevention and control of adverse maternal and fetal outcome associated with hypothyroidism.