The CAD is the most common cardiovascular disease worldwide and therefore its early diagnosis and management can save thousands of lives annually [1]. Coronary syndromes without ST elevation are a heterogeneous disorder ranging from Stable Angina (SA) without evidence of myocardial necrosis to NSTE-ACS which includes UA and NSTEMI [2]. Now-a-days, conventional coronary angiography is the gold standard for diagnosis of obstructive CAD [3]. The diagnosis of NSTEMI and the urgent revascularisation strategy is supported by many biochemical markers and risk scores however, these markers becomes elevated when ischemia and infarction has occurred. Therefore, a valuable biomarker for prediction of presence and severity of CAD before occurrence of such events is required [4].
The cardiomocytes produce a pro-hormone known as B-Type Natriuretic Peptide (BNP) that consists of 32 amino acids. The increase in ventricular pressure and volume trigger the release of its active form into the circulation [5]. In addition BNP and NT-proBNP can be released in response to myocardial ischemia and provide prognostic information in NSTEMI and unstable angina [6]. Hence, the present study compared serum NT-proBNP levels in NSTE-ACS and controls and assessed the relation of serum NT-proBNP with the severity of CAD in patients with NSTE-ACS.
Materials and Methods
Study Population
This observational study was carried out after obtaining approval from institutional Medical Ethics Committee of Alexandria University (020978, 15/6/2017), from September 2017 to September 2019. A total of 80 study subjects (cases 60 and controls 20) that presented to Cardiology Department, Alexandria Main University Hospital, Egypt, after taking informed consent to participate, were included.
Sample Size Calculation
The sample sizes of 60 cases and 20 controls achieve 80% power to detect a difference of at least 30 pg/mL in the mean NT-proBNP level between cases and controls, assuming standard deviation of (50) with a significance level (alpha) of 0.05, using Mann-Whitney U test. The statistical power was calculated using NCSS 2004/PASS 2000 software.
Inclusion Criteria:
Cases: Sixty patients of both genders in the age range of 40-80 years presenting with history of NSTE-ACS, that were referred to coronary angiography unit within 72 hours of hospital admission. All patients had preserved ejection fraction (EF>50%).
Controls: Twenty matched subjects with normal coronary angiography.
Exclusion Criteria:
Cases and controls: Patients with acute or chronic heart failure, moderate to severe valvular heart disease, cardiomyopathy, renal disease with creatinine clearance < 50 mL/min, neoplastic disease, inflammatory and infectious diseases.
Laboratory Analysis
All patients and controls were subjected to detailed history taking including cardiovascular disease risk factors and full clinical examination. Electrocardiography (ECG) was performed on all study subjects.
Sample Collection
Five mL of venous blood was drawn in red capped tubes, serum was separated and stored at -70°C. Blood urea, serum creatinine and Cardiac troponin I were measured in all patients.
Method of measurement of serum NT-pro BNP
Serum NT-pro BNP was analysed before coronary angiography on an Elecsys 2010 analyser, a commercially available electrochemiluminescent sandwich immunoassay (ElecsysproBNP, Roche Diagnostics, Mannheim, Germany). The lowest and highest detection limits of the assay were at 5 to 35.000 pg/mL [7].
Conventional Echocardiography and Tissue Doppler Imaging
Echocardiography was performed within 24 hour of admission using (HD11 XE, Philips) machine. The following parameters were measured: Left Ventricular Ejection Fraction (LVEF), wall motion and Wall Motion Score Index (WMSI). Left ventricular diastolic function parameters including E wave, A wave, E/A ratio, E wave Deceleration Time (DT), Ea wave and E/Ea ratio were measured. Assessment of cardiac valves was carried out [8,9].
Coronary Angiography
Coronary angiography was done on all patients. Physicians who didn’t know about patient’s clinical presentation or NT-proBNP serum levels graded all coronary angiographic data, with coronary diameter stenosis >50% was considered significant. Thrombolysis In Myocardial Infarction (TIMI) flow grade was used to assess epicardial coronary flow [10]. CAD severity and complexity were assessed using Gensini and Syntax scores (SX score) [11,12]. The SX score was calculated using a dedicated software [13].
Statistical Analysis
Statistical analysis was performed by using Statistical Package for the Social Sciences (SPSS) system for windows (version 20 Chicago, IL, USA). The Kolmogorov- Smirnov, Shapiro and D’agstino tests were used to verify the normality of distribution of variables. Comparisons between groups for categorical variables were assessed using Chi-square test (Fisher or Monte Carlo). Qualitative variables were presented as number and percentage, while quantitative variables were expressed as mean±Standard Deviation (SD). To compare abnormally distributed quantitative variables, the Mann-Whitney U test was used. To compare normally distributed quantitative variables, the Student’s t-test was used. For comparison between three groups for abnormally distributed quantitative variables, Kruskal Wallis test was used. Correlation between variables was tested by using the spearman’s correlation test. The results were considered significant when the p-value was <0.05. Receiving Operating Characteristics (ROC) curve was used to identify the cut-off value for diagnosis of CAD. Kaplan-Meier curves for six months MACE by median NT-proBNP was presented.
Results
The mean value of serum NT-proBNP in NSTE-ACS (662.7±635.2)pg/mL was significantly higher than that in control group (102.3±96.4) pg/mL, p<0.001 [Table/Fig-1]. Out of 60 cases that underwent coronary angiography, it was found that 22 (36.7%) had Single Vessel Disease (SVD) and 20 (33.3%) had two vessel disease followed by multivessel disease in 18 (30%) as shown in [Table/Fig-2].
Baseline, demographic data and echocardiographic data of the study population.
| Cases, (n=60) Mean±SD | Control, (n=20) Mean±SD | p-value |
|---|
| Age (years) | 60.6±9.1 | 56.8±7.2 | 0.093 |
| Male, n (%) | 50 (83.3%) | 12 (60%) | 0.060 |
| BMI (kg/m2) | 28.2±2.3 | 27.3±2.6 | 0.147 |
| Risk factors |
| Smoking, n (%) | 33 (55%) | 3 (15%) | 0.002* |
| Family history of CAD, n (%) | 23 (38.3%) | 3 (15%) | 0.054 |
| Hypertension, n (%) | 40 (66.7%) | 13 (65%) | 0.891 |
| Diabetes, n (%) | 29 (48.3%) | 2 (10%) | 0.002* |
| Hyperlipdemia, n (%) | 60 (100%) | 12 (60%) | <0.001* |
| Triglycerides (mg/dL) | 145.2±67.8 | 123.1±45.8 | 0.173 |
| Total cholesterol (mg/dL) | 165.8±52.9 | 156.9±41.0 | 0.512 |
| LDL (mg/dL) | 91.3±34.7 | 85.9±37.4 | 0.554 |
| HDL (mg/dL) | 39.1±9.2 | 45.5±8.5 | 0.008* |
| Random blood glucose (mg/dL) | 110.4±57.1 | 78.7±22.6 | 0.017* |
| Serum Creatinine (mg/dL) | 1±0.3 | 0.9±0.3 | 0.075 |
| eGFR (mL/min/1.73 m2) | 84.6±50.6 | 85.3±20 | 0.110 |
| ST depression, Yes (%) | 60 (100%) | 12 (60%) | <0.001* |
| Troponin I (ng/mL) | 0.7±2.3 | 0±0 | 0.607 |
| Grace score | 144.2±20.6 | 104.8±16.9 | <0.001* |
| NT-proBNP (pg/mL) | 662.7±635.2 | 102.3±96.4 | <0.001* |
| LVEF (%) | 60±0.08 | 64±0.06 | 0.063 |
| WMSI | 1.17±0.18 | 1.05±0.13 | 0.004* |
| E/Ea | 9.41±4.55 | 8.43±2.83 | 0.705 |
χ2: Chi square test; *: Statistically significant at p ≤ 0.05; p: p-value for comparing between the studied groups; t: Student t-test; U: Mann whitney test; A: pulse wave Doppler late diastolic velocity; CAD: Coronary artery disease; eGFR: estimated glomerular filtration rate; E: Pulse wave Doppler early diastolic velocity; FE: Fisher exact; HDL: High density lipoprotein; LDL: Low density lipoprotein; LVEF: Left ventricular ejection fraction; NT pro BNP: N-terminal pro brain natriuretic peptide; WMSI: Wall motion score index; SD: Standard deviation
Distribution of the studied cases according to coronary angiographic findings.
| No. (%) |
|---|
| Coronary angiography |
| Single vessel disease | 22 (36.7%) |
| Two vessels | 20 (33.3%) |
| Multi vessel disease | 18 (30%) |
| Single vessel |
| LAD | 15 (25%) |
| RCA | 7 (11.7%) |
| Two vessel |
| LAD+LCX | 5 (8.3%) |
| LAD+RCA | 13 (21.7%) |
| LM+LCX | 1 (1.7%) |
| LM+LAD | 1 (1.7%) |
| Multi vessel disease | 18 (30%) |
| Syntax score |
| Mean±SD. | 16.9±9.9 |
| Gensini score |
| Mean±SD | 51.8±47.3 |
LAD: Left anterior descending coronary artery; LCX: Left circumflex coronary artery; LM: Left main coronary artery, RCA: Right coronary artery; SD: Standard deviation
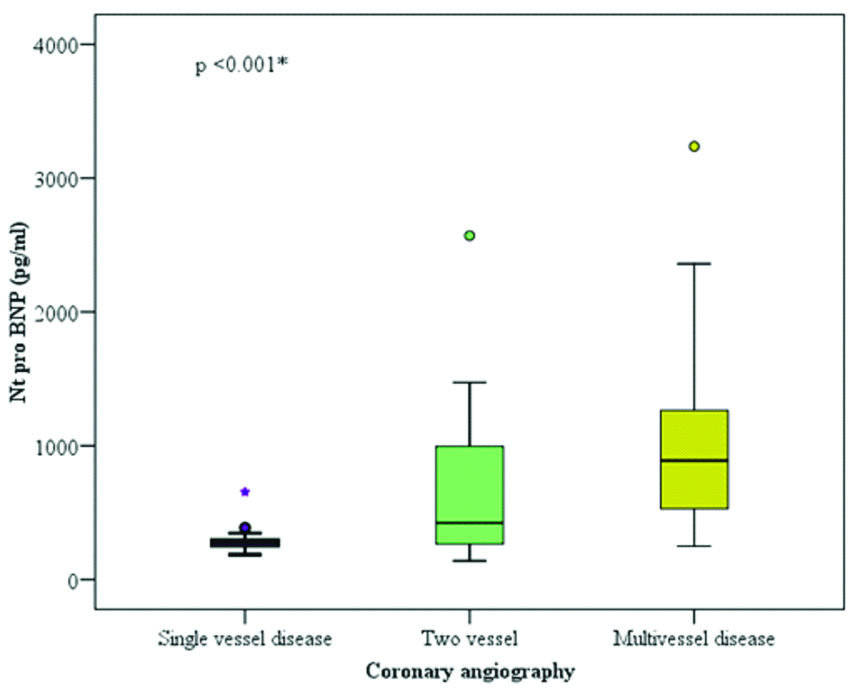
The NT-proBNP, Gensini score and syntax score were higher in multivessel disease group as compared to two vessel and SVD groups and the association was statistically significant with p-values of <0.001, <0.001, <0.001, respectively as shown in [Table/Fig-3]. Serum NT-proBNP IQR and extent of CAD is shown in [Table/Fig-4]. Serum NT-proBNP levels were found to be significantly higher in the High Syntax Score (HSX) group compared to the intermediate and Low Syntax Score (LSX) tertiles and was higher in the Intermediate Syntax Score (ISX) group compared to the LSX group. The Nt-proBNP levels showed an increase from LSX to HSX tertiles. (p=0.006) as shown in [Table/Fig-5]. The most common six months MACE in NSTE-ACS patients was myocardial infarction that occurred in 11 (18.3%). Mortality and stroke occurred in 1 (1.7%), 1 (1.7%), respectively as shown in [Table/Fig-6].
Serum NT-proBNP and extent of Coronary Artery Disease (CAD).
| Coronary angiography | H | p-value |
|---|
| Single vessel disease (n=22) | Two vessel (n=20) | Multivessel disease (n=18) |
|---|
| NT-proBNP |
| Mean±SD | 292.2±92.1 | 693.5±602 | 1081.3±787.7 | 22.388* | <0.001* (0.0000138) |
| Median (IQR) | 276.5 (250-305) | 423.5 (262-999.8) | 889 (509.8-1351.5) |
| Gensini score |
| Mean±SD | 12.7±11.6 | 57±35.2 | 93.7±48.5 | 35.367* | <0.001* (0.0000000209) |
| Median (IQR) | 8.5 (5-14.9) | 54 (24.5-92) | 100.5 (39.5-136.5) |
| Syntax score |
| Mean±SD | 8.1±4.7 | 19±7.3 | 25.2±8.5 | 34.591* | <0.001* (0.0000000308) |
| Median (IQR) | 6.5 (50-10.3) | 18 (13.4-24.8) | 24.3 (16-32.4) |
H: H for Kruskal wallis test; p: p-value for association between different categories; *: Statistically significant at p ≤0.05; NT-proBNP: N terminal pro brain natriuretic peptide; SD: Standard deviation; IQR: Interquartile Range
Serum NT-proBNP Interquartile Range (IQR) and extent of Coronary Artery Disease (CAD).
Relation between serum NT-proBNP and Syntax Score (SS).
| Syntax score | H | p-value |
|---|
| Low (0-21) (n=40) | Inter (22-32) (n=15) | High (>33) (n=5) |
|---|
| NT-proBNPpg/mL |
| Mean±SD | 542.5±535.8 | 800.9±585.8 | 1210±1166.2 | 10.140* | 0.006* |
| Median (IQR) | 292.5 (251-544.8) | 750 (385-1046) | 750 (475.5-2174.5) |
H: H for Kruskal wallis test; p: p-value for association between different categories; *: Statistically significant at p ≤0.05; NT-proBNP: N terminal pro brain natriuretic peptide; SD: Standard deviation; IQR-Interquartile Range
Distribution of six months MACE among NSTE-ACS patients.
| MACE | No. (%) |
|---|
| Mortality | 1 (1.7%) |
| Stroke | 1 (1.7%) |
| MI | 11 (18.3%) |
| HF | 5 (8.3%) |
| Re PCI | 2 (3.3%) |
| CABG | 3 (5%) |
MACE: Major adverse cardiovascular events; CABG: Coronary artery bypass grafting; MI: Myocardial infarction; HF: Heart failure; PCI: Percutaneous coronary intervention
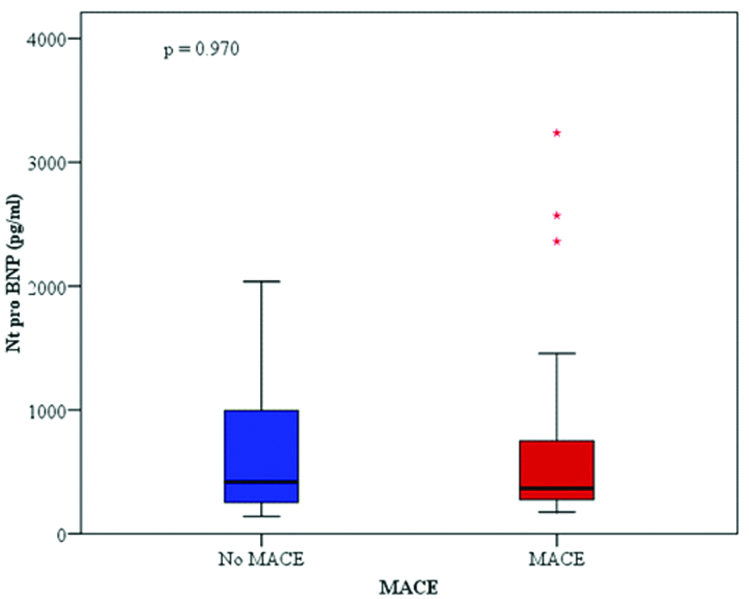
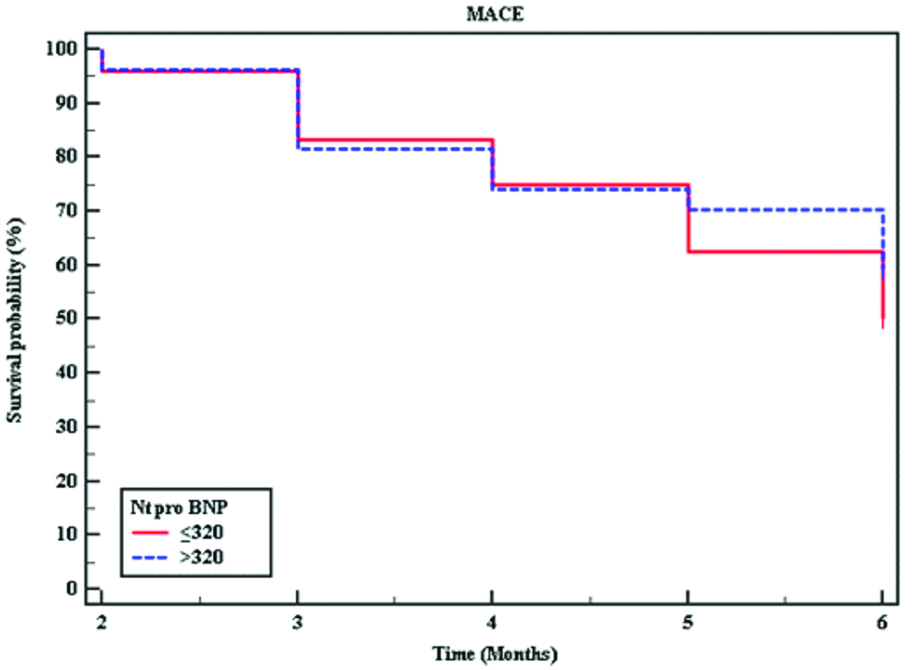
The serum NT-proBNP IQR in patients with six month MACE didn’t differ from those without MACE 418.5 (139-2037), 366 (175-3237), respectively as shown in [Table/Fig-7]. Kaplan-Meier survival curve for six months MACE by median NT-proBNP. The p-value (0.557) is derived by log-rank test is shown in [Table/Fig-8].
Relation between NT-proBNP Interquartile Range (IQR) and six months MACE and in Non ST Elevation Acute Coronary Syndrome (NSTE-ACS) patients.
Kaplan-Meier survival curve for six months Major Adverse Cardiovascular Events (MACE) by median NT-proBNP. The p-value (0.557) is derived by log-rank test.
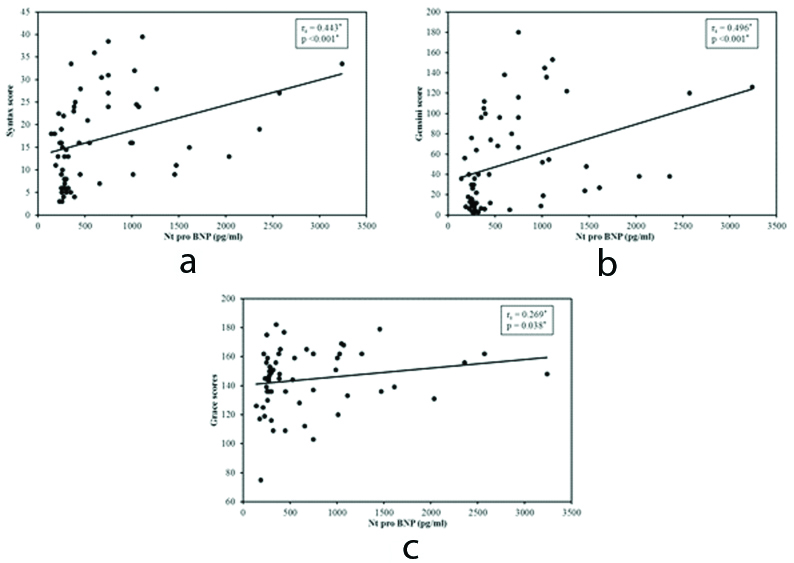
There was significant positive correlation between the NT-proBNP and the Grace risk score (r=0.269, p=0.038), Syntax score (r=0.443, p<0.001) and Gensini score (r=0.496, p<0.001) as shown in [Table/Fig-9].
Correlation between NT-proBNP with Syntax score (a), Gensini score (b) and Grace score (c) in Non St Elevation Acute Coronary Syndrome (NSTE-ACS) patients.
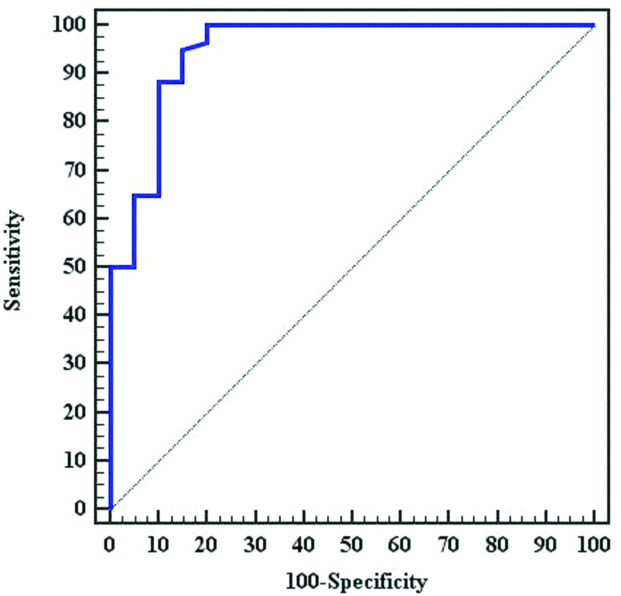
In a ROC curve analysis, serum NT-proBNP value of 139 pg/mL was the cut-off value in the diagnosis of CAD (AUC=0.950, 95% CI: 0.890-1.00) [Table/Fig-10].
ROC curve of NT-proBNP for diagnosis or exclusion of Coronary Artery Disease (CAD).
Discussion
Natriuretic peptides are well established marker for diagnosis and prognosis of heart failure, left ventricular dysfunction and it has been found that it becomes elevated in ischemic heart disease independent of ventricular wall stress [14]. In a patient with stable CAD, BNP levels have been correlated linearly with number of coronary artery involvement [15].
This study compared serum NT-proBNP levels in NSTE-ACS patients and controls and assessed the relation between serum NT-proBNP and the severity of CAD in patients with NSTE-ACS. In this study prevalence of risk factors such as, Diabetes Mellitus (DM), dyslipidemia and smoking in the CAD group were significantly higher than in the control group (all p<0.05) and this comes in agreement with an observation by Wu N et al., investigated total of 658 consecutive patients that were divided into two groups based on angiograms [16], CAD group (n=484) and angiographic normal control group (n=174). They demonstrated that the prevalence of risk factors such as age, male gender, DM, dyslipidemia, smoking and family history of CAD in the CAD group were higher than that in the control group. In the present study, the mean value of NT-proBNP in NSTE-ACS (662.7±635.2) pg/mL was significantly higher than that in control group (102.3±96.4) pg/mL with p-value <0.001. This comes with what was reported by Wu N et al., who found that NT-proBNP levels in the CAD group were significantly higher than that in the angiographically normal control group [16].
In this study, the NT-proBNP value of 139 pg/mL was found to be cut-off value in the diagnosis of CAD. A similar observation by Xu L et al., who found that NT-proBNP level acts as a predictor of positive results of angiographic stenosis and Fractional Flow Reserve (FFR), with the AUC being 0.697 and 0.787, respectively [17]. They found that NT-proBNP level of 101.5 pg/mL had a sensitivity of 0.49, a specificity of 0.92 and an accuracy of 1.41 in differentiating patients with advanced CAD. In the FFR-measured population, the AUC was 0.787, while NT-proBNP level of 118.0 pg/mL had a sensitivity of 0.61, a specificity of 0.90 and accuracy of 1.51. They concluded that NT-proBNP levels are correlated with the severity of anatomic coronary occlusion and inducible myocardial ischemia.
In this study, the NT-proBNP, Gensini score and syntax score were higher in multivessel disease group as compared to two vessel disease and single vessel disease groups and the association was statistically significant with p-values of <0.001, <0.001, <0.001, respectively. This was similar to study by Rajabiani A et al., where they found that a progressive significant increase in the NT-proBNP concentration according to the Gensini score and the number of involved vessels after adjustment for sex and age [18].
From these observations it can be concluded that higher levels of NT-proBNP among ACS patients were associated with the severity of angiographic lesions in terms of both the Gensini score and the number of involved vessels.
In this study, NT-proBNP levels were found to be significantly higher in the HSX group compared to the intermediate SX score and low SX score groups. It was also high in the ISX group compared to the LSX group. The NT-proBNP levels showed an increase from LSX to HSX tertiles, p=0.006. This was demonstrated by Kurtul A et al., and Sarak T and Karadeniz M, who observed that NT-proBNP levels were found to be significantly higher in the HSX group compared to the other groups (p<0.001) and in the ISX group compared to the LSX group (p<0.001) [7,19]. The NT-proBNP levels showed an increase from LSX to HSX tertiles.
From previous observation, it can be concluded that NT-ProBNP levels in patients with NSTE-ACS on admission are associated with severity and complexity of CAD as assessed by Gensini and Syntax scores.
In this study, it was found that the mean Nt-proBNP was insignificantly higher in patients with six month MACE than in patients without MACE (678.66±740.81 vs. 644.46±500.94, p=0.970). This is in contrast to Shon HS et al., who studied the prognostic value of NT-proBNP for MACE among patients with NSTEMI [4]. They reported that NT-proBNP is a significant variable among patients with MACE compared with those without MACE. They also concluded that NT-proBNP is a valuable predictor for 12-month MACE among patients with NSTEMI and in those with heart failure. The difference may be related to small sample size in this study, low age range, most of present study cases were males, relatively preserved ejection fraction (0.60±0.08%) and shorter follow-up period.
In this study, it was found a significant positive correlation between the NT-proBNP and the Grace risk score (r=0.269, p=0.038). This come in accordance with study by Klingenberg R et al., who revealed that the prognostic accuracy of the Grace score was improved when combined with three individual biomarkers including high sensitivity troponin T (hsTnT), NT-proBNP and high sensitivity C-reactive protein (hsCRP) [20].
This study demonstrated a significant positive correlation between the NT-proBNP and the Gensini score (r=0.496, p<0.001). A similar observation was revealed by Wu N et al., [16]. From the previous findings it can be inferred that there was a direct positive correlation between NT-proBNP and Gensini score in patients with ACS with preserved left ventricular function and can be used as an important marker to risk stratify those patients.
In the present study, there was a significant positive correlation between the NT-proBNP in the studied patients with NSTE-ACS and the Syntax score (r=0.443, p<0.001), this was in agreement with study by Sarak T and Karadeniz M, who reported that NT-ProBNP levels in patients with myocardial infarction on admission were independently associated with extent, severity and complexity of coronary atherosclerosis as assessed by Syntax score [19]. This study reveals that NT-proBNP is a candidate for entry into the setting of principal risk scores. Thus, serum NT-proBNP may be considered as an indicator of regional ischemia and can predict the extent, severity and complexity of CAD in patients with NSTE-ACS and preserved left ventricular systolic function.
Limitation(s)
The study didnot compare serum NT-proBNP levels to high sensitivity C-reactive protein or cytokine levels.
Conclusion(s)
The serum NT-proBNP is increased in patients with NSTE-ACS with preserved ejection fraction and it has a significant correlation with the severity and complexity of CAD in NSTE-ACS. Hence NT-proBNP can be useful measure to predict the presence and severity of CAD, but has no impact on six months MACE.
χ2: Chi square test; *: Statistically significant at p ≤ 0.05; p: p-value for comparing between the studied groups; t: Student t-test; U: Mann whitney test; A: pulse wave Doppler late diastolic velocity; CAD: Coronary artery disease; eGFR: estimated glomerular filtration rate; E: Pulse wave Doppler early diastolic velocity; FE: Fisher exact; HDL: High density lipoprotein; LDL: Low density lipoprotein; LVEF: Left ventricular ejection fraction; NT pro BNP: N-terminal pro brain natriuretic peptide; WMSI: Wall motion score index; SD: Standard deviation
LAD: Left anterior descending coronary artery; LCX: Left circumflex coronary artery; LM: Left main coronary artery, RCA: Right coronary artery; SD: Standard deviation
H: H for Kruskal wallis test; p: p-value for association between different categories; *: Statistically significant at p ≤0.05; NT-proBNP: N terminal pro brain natriuretic peptide; SD: Standard deviation; IQR: Interquartile Range
H: H for Kruskal wallis test; p: p-value for association between different categories; *: Statistically significant at p ≤0.05; NT-proBNP: N terminal pro brain natriuretic peptide; SD: Standard deviation; IQR-Interquartile Range
MACE: Major adverse cardiovascular events; CABG: Coronary artery bypass grafting; MI: Myocardial infarction; HF: Heart failure; PCI: Percutaneous coronary intervention