Malignant Warty Lesion at Cervix in Asymptomatic Postmenopausal Woman- A Case Report
Sangam Jha1, Vidhi Vanya2, Tarun Kumar3
1 Associate Professor, Department of Obstetrics and Gynaecology, AIIMS Patna, Patna, Bihar, India.
2 Senior Resident, Department of Obstetrics and Gynaecology, AIIMS Patna, Patna, Bihar, India.
3 Assistant Professor, Department of Pathology, AIIMS Patna, Patna, Bihar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Sangam Jha, Phulwarisharif, Patna, Bihar, India.
E-mail: sangam.jha78@gmail.com
Verrucous carcinoma is a rare variant of cervical carcinoma, usually occurs in postmenopausal group. Aetiology is still not understood but it is thought to be associated with chronic irritation and inflammation. Histological diagnosis is usually difficult since the pathologic findings may be benign especially if biopsy specimen contains only surface epithelium. Prognosis of this histological subtype is better compared to the well-differentiated Squamous Cell Carcinoma (SCC) of cervix. Author present a case of verrucous carcinoma where patient came for routine check-up and on pelvic examination; cervix was replaced by friable, cauliflower like warty growth, clinically staged as stage 1B. Punch biopsy was taken from the growth and it reported benign pathology but due to high index of suspicion, repeat biopsy was taken and second histopathology also reported benign pathology. Contrast Enhanced Computed Tomography (CECT) whole abdomen was advised as clinical picture and Histopathological Examination (HPE) was not matching. CECT reported mass confined to the cervix, features consistent with carcinoma cervix. So, the patient underwent radical hysterectomy with pelvic lymphadenectomy. Final histopathology reported verrucous carcinoma of cervix. Patient is under regular follow-up and free of disease since 1 year.
Punch biopsy, Radical hysterectomy, Verrucous carcinoma
Case Report
A 74-year-old postmenopausal woman P4L4 presented for routine check-up. There was no history of any bowel or bladder complaints, postmenopausal bleeding or discharge, weight or appetite loss. On repeated questioning, patient gave history of occasional itching in the vulva and vagina for last six months. The gynaecologic examination revealed the cervix flushed with vagina along with an irregular, friable, warty growth of 3×4 cm involving both anterior and posterior lip of cervix which bled slightly on touch. Bimanual examination revealed normal sized, ante-verted uterus with bilaterally free parametrium. Vaginal examination findings were confirmed on rectal examination and clinical diagnosis of carcinoma cervix stage 1B was made [based on International Federation of Gynecologists and Obstetricians (FIGO)] staging of carcinoma of the cervix uteri 2018) [1].
Punch biopsy was taken from the growth revealed features of polypoidal tissue (acanthosis epidermis and parakeratosis with no evidence of dysplasia or malignancy). As there was high clinical suspicion, a repeat biopsy was performed. However, repeat punch biopsy also returned negative for malignancy. No sub-epithelium was noted in the biopsied epithelium. Based on the nature of the growth and age of the patient, there was a strong clinical suspicion in favour of cervical carcinoma.
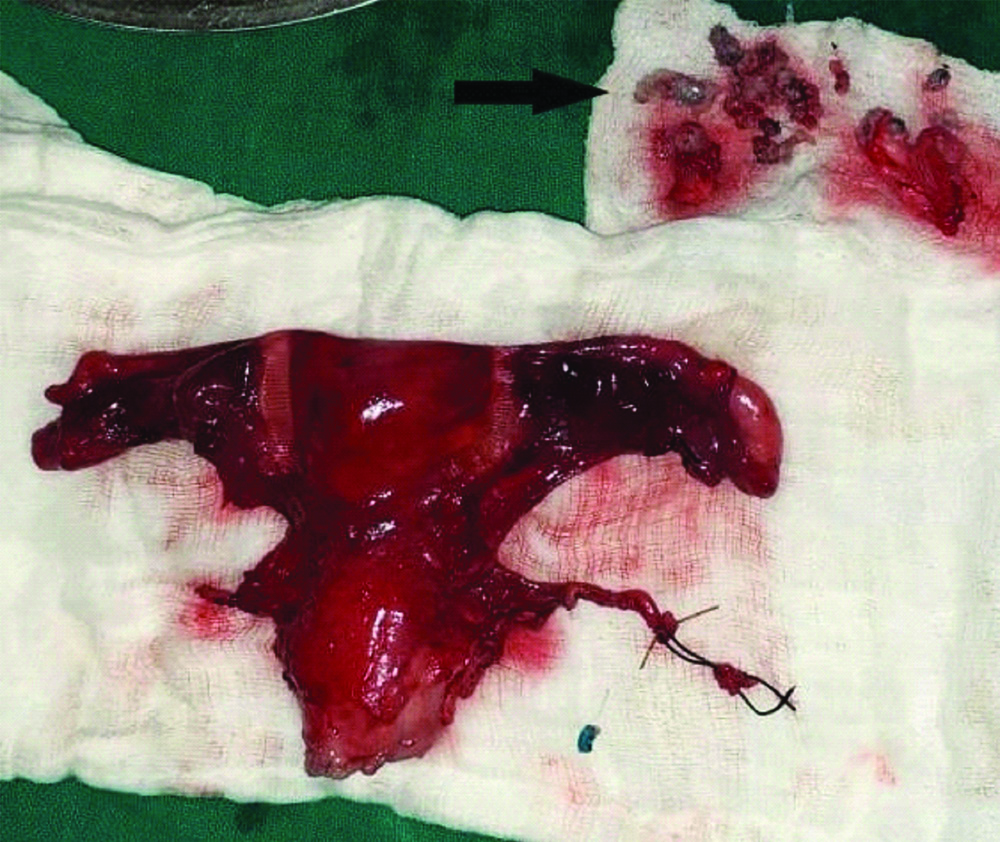
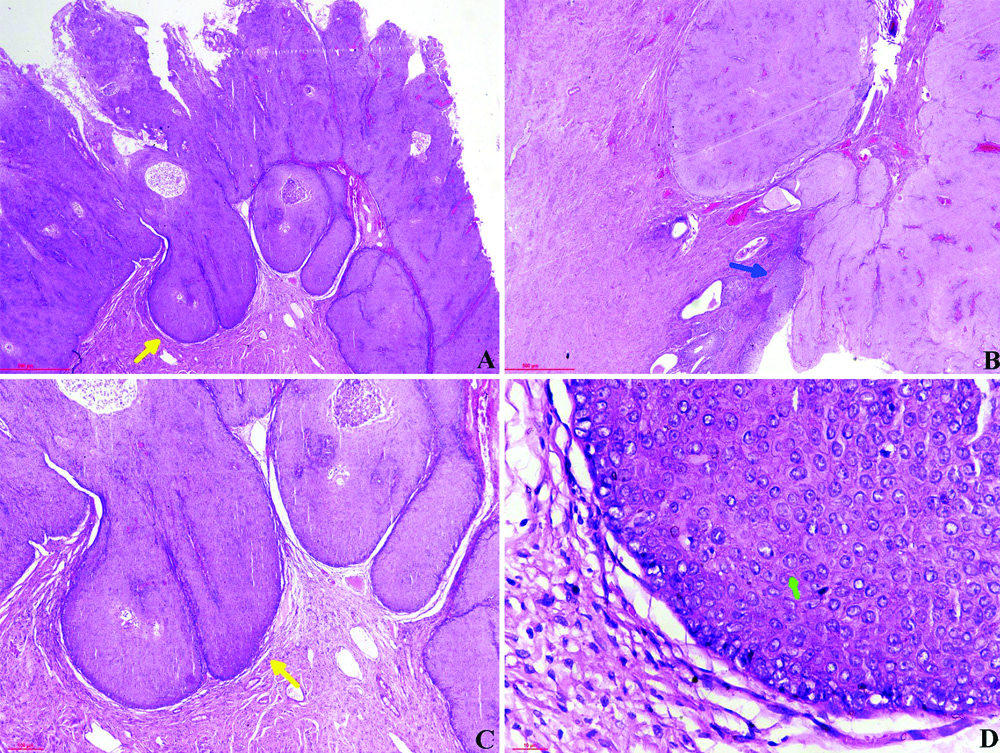
A CECT of whole abdomen was performed. It showed an irregular cervix with soft tissue attenuating heterogeneously enhancing mass of 4×2.3 cm, which was confined to the cervix. Features were suggestive of Carcinoma cervix (stage 1B). Hence, the decision to proceed with radical hysterectomy with bilateral pelvic lymphadenectomy was taken. Radical hysterectomy along with pelvic lymphadenectomy was performed and tissue sent for HPE. Gross appearance of specimen after removal is showing complete excision with uterus [Table/Fig-1]. Histopathology of multiple sections studied from the cervical growth showed an exophytic tumour with hyperkeratotic, acanthotic squamous epithelium with invasion of the underlying stroma in the form of broad and bulbous epithelial pegs with a pushing border [Table/Fig-2]. Individual tumour cells show minimal to mild nuclear pleomorphism, high Nuclear:cytoplasmic ratio, vesicular chromatin, prominent nuclei with moderate amount of eosinophilic cytoplasm. Occasional atypical mitosis was also noted. These histopathological features were suggestive of SCC, verrucous type. The postoperative period was unremarkable and discharge was given on 8th postoperative day. Patient is under regular follow-up and disease free for the last one year.
Macroscopic appearance of excised material showing the complete specimen with uterus, bilateral tubes, ovaries and the growth at cervix. At upper right corner, wart like tissue (black arrow) is shown which got detached from the specimen while removing.
A &2 B (H&E x20): Markedly acanthotic and keratinized squamous epithelium (yellow arrow) invading the subjacent stroma with bulbous and broad rete ridges. (blue arrow). C (H&E x40): Bulbous & broad rete ridges invading the stroma. (yellow arrow). D (H&E; ×400): Squamous epithelium shows minimal cytological atypia (green arrow)
Discussion
Cervical cancer is the second most common female cancer in developing countries. The common histological variants are squamous, adenocarcinoma and adenosquamous carcinoma. Verrucous carcinoma of genital tract is a rare variant of well differentiated SCC. It is usually found in the oral cavity, skin and larynx [2] and rarely occurs in the genital tract with an incidence of about 0.2% of all gynaecological cancers [3]. In genital tract involvement of the vulva and cervix seems to be more common than the vagina [4]. It is a slow growing, locally invasive tumour that hardly metastasizes. It is commonly misinterpreted as benign condyloma acuminata, resulting in a delay of the appropriate treatment. In this case too, the growth involved the entire cervical canal with invasion of underlying stroma, but without local or distant metastasis.
It is primarily a tumour of the postmenopausal group but can occur at young age too. A case of fulminant verrucous carcinoma has been reported in 29-year-old female [5]. Patient of the present case was 74-year-old and menopausal since last 20 years.
The aetiology is uncertain, although it has been associated with chronic irritation and inflammation and infection with Human Papilloma Virus (HPV) (types 6, 11 and 16). However, few studies suggested that the presence of HPV in genital verrucous lesion favours the diagnosis of giant condyloma and exclude the diagnosis of verrucous carcinoma [6-8]. In the present case too, HPV could not be detected. Maeyama M et al., also could not detect HPV antigen by immunohistochemistry in a case of cervical verrucous carcinoma [7]. Pino de M et al., conducted a comprehensive analysis of HPV prevalence in 27 specimens of verrucous carcinoma of different origin and they failed to prove any causal relationship of HPV to development of verrucous carcinoma [8].
Owing to its rare nature in female genital tract, reports of cytological description in cervico-vaginal smears are also scarce. Pantanowitz L et al., reviewed 26 cases of uterine cervical verrucous carcinoma and reported that 23% cases showed negative cytology. This high false-negative rate on cytology could be brought about by the high degree of epithelial maturation with minimal nuclear atypia [9]. Because of the rarity of verrucous carcinoma, diagnosis is difficult to make as biopsied material is either inadequate or may exhibit epithelial maturation and a deceptive lack of atypia [10]. Clinical suspicion should be ferocious and evaluation should be done cautiously to arrive at correct diagnosis as the pathologic findings may mimic those of condyloma or papillary SCC or it may be benign in nature [11]. Verrucous carcinoma invades locally with ‘pushing margin’ and fibro-vascular cores are limited to the superficial layers, in contrast to a benign condyloma, of which the fibro-vascular layers extend from a deep layer to the surface [12]. Papillary SCC differs from verrucous SCC by the presence of true papillae, greater nuclear atypia, inconspicuous keratinization, and the presence of an invasive deep margin. However, in some cases, it may be difficult to obtain the material from the base and an erroneous diagnosis can be made. In addition, the specimen may exhibit epithelial maturation and cytological atypia may be absent. In present case too, repeated biopsies showed benign features as the biopsy specimen consisted of only the surface epithelium and hence, invasion of the underlying stroma could not be evaluated. Similar case reported in postmenopausal women with utero-cervical prolapse by Dane B et al., where erroneous diagnosis of giant condyloma was made from the biopsy specimen as it consisted only superficial layers [13]. The age, postmenopausal status and the clinical appearance of the lesion clued to clinically distinguish it from benign polyp. The treatment of verrucous carcinoma is still a matter of discussion. As it is a slow but relentlessly expanding tumour, unlikely to involve lymphnodes or distant areas, radical surgery remains the mainstay of treatment with complete removal of tumour along with free margin. Primary hysterectomy, with or without adjuvant radiotherapy, has achieved a 50% cure rate in most cases [2]. Radiotherapy is not recommended due to reported cases of sarcomatous or anaplastic transformation of verrucous carcinomas after radiation [4]. Surgery with adjuvant interferon has also been used for local recurrence after surgery [14,15]. There are no reports of use of chemotherapy in cervical verrucous carcinoma. Similar cases of verrucous carcinoma of cervix in postmenopausal women have been reported previously [2,10,14,16], but most of them presented with vaginal bleeding, this is the first case where patient was asymptomatic and thus deserve mention.
Conclusion(s)
As cervical verrucous carcinoma is a rare variant with poorly defined cytological features, In present case, punch biopsy findings are not correlating with the clinical findings and CECT played an important role in its diagnosis, hence early diagnosis and appropriate treatment is required in case of any suspicion.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 16, 2020
Manual Googling: May 12, 2020
iThenticate Software: Jun 25, 2020 (16%)
[1]. Bhatla N, Berek SJ, Fredes CM, Denny LA, Grenman S, Karunaratne K, Revised FIGO staging for carcinoma of the cervix uteriInternational Journal of Gynecology and Obstetrics 2019 145(1):129-35.10.1002/ijgo.1274930656645 [Google Scholar] [CrossRef] [PubMed]
[2]. Chen DC, Yu MH, Yu CP, Liu JY, Verrucous carcinoma of the uterine cervixZhonghua Yi Xue Za Zhi (Taipei) 2000 63(10):765-69. [Google Scholar]
[3]. Bray F, Colombet M, Mery L, Piñeros M, Znaor A, Zanetti R, Cancer Incidence in Five Continents, Vol. XI (electronic version)LyonInternational Agency for Research on Cancer [Google Scholar]
[4]. Crowther ME, Lowe DG, Shepherd JH, Verrucous carcinoma of the female genital tract: a reviewObst Gynaecol Survey 1988 43(1):263-80.10.1097/00006254-198843050-00003 [Google Scholar] [CrossRef]
[5]. Anghel RM, Trifanescu OG, Mitrica RI, Curea FG, Botnariuc I, Herghelegiu CG, Good prognosis went badly: Fulminant evolution of a 29-year-old patient with verrucous carcinoma of the cervixJ Adolesc Young Adult Oncol 2017 6(3):499-502.10.1089/jayao.2017.000928498727 [Google Scholar] [CrossRef] [PubMed]
[6]. Robertson DI, Maung R, Duggan MA, Verrucous carcinoma of the genital tract: Is it a distinct entity?Can J Surg 1993 36(2):147-51. [Google Scholar]
[7]. Maeyama M, Fukuma K, Tanaka N, Inoue S, Tooya T, A case of verrucous carcinoma of the uterine cervix: Clinical, light, and electron microscopic, and immunohistological observationsGynecol Oncol 1985 22(2):244-49.10.1016/0090-8258(85)90033-2 [Google Scholar] [CrossRef]
[8]. del Pino M, Bleeker MC, Quint WG, Snijders PJ, Meijer CJ, Steenbergen RD, Comprehensive analysis of human papillomavirus prevalence and the potential role of low-risk types in verrucous carcinomaMod Pathol 2012 25(10):1354-63.10.1038/modpathol.2012.9122684225 [Google Scholar] [CrossRef] [PubMed]
[9]. Pantanowitz L, Upton MP, Wang HH, Nasser I, Cytomorphology of verrucous carcinoma of the cervixActa Cytol 2003 47(6):1050-54.10.1159/00032664514674078 [Google Scholar] [CrossRef] [PubMed]
[10]. Kanamori T, Cytology of uterine cervical verrucous carcinomaTaiwan J Obstet Gynaecol 2008 47(10):367-69.10.1016/S1028-4559(08)60147-3 [Google Scholar] [CrossRef]
[11]. Frega A, Stentella P, Tinari A, Vecchione A, Marchionni M, Giant condyloma acuminatum or Buschke-Lowenstein tumour: review of the literature and report of three cases treated by CO2 laser surgery. A long-term follow-upAnticancer Res 2002 22(2B):1201-04. [Google Scholar]
[12]. Shidara Y, Karube A, Watanabe M, Satou E, Uesaka Y, Matsuura T, A case report: Verrucous carcinoma of the endometrium-the difficulty of diagnosis, and review of the literatureJ Obstet Gynaecol Res 2000 26(3):189-92.10.1111/j.1447-0756.2000.tb01309.x10932980 [Google Scholar] [CrossRef] [PubMed]
[13]. Dane B, Dane C, Erginbas M, Baran S, Cetin A, Verrucous carcinoma of the cervix in a case with uterine prolapseAnn Diagn Pathol 2009 13(5):344-46.10.1016/j.anndiagpath.2009.02.00519751912 [Google Scholar] [CrossRef] [PubMed]
[14]. Yorganci A, Serinsoz E, Ensari A, Sertcelik A, Ortac F, A case report of multicentric verrucous carcinoma of the female genital tractGynaecol Oncol 2003 90(2):478-81.10.1016/S0090-8258(03)00270-1 [Google Scholar] [CrossRef]
[15]. Matsumoto Y, Ishiko O, Nishimura S, Ogita S, Kubota K, Haba T, Angiogenesis in metastatic verrucous carcinoma of the uterine cervixOncol Rep 2000 7(5):1079-82.10.3892/or.7.5.1079 [Google Scholar] [CrossRef]
[16]. Szczepulska E, Nasierowska-Guttmejer A, Bidziński M, Cervical verrucous carcinoma involving endometrium. Case reportEur J Gynaecol Oncol 1999 20(1):35-37. [Google Scholar]