Glomus tumour is a rare small benign lesion which is typically located at fingertip. Most patients with glomus tumour have delayed diagnosis. Recognition of the classical triad of glomus tumour which include paroxysmal pain, exquisite tenderness to touch and cold intolerance; and advanced imaging like MRI and biopsy would help in making the diagnosis. Here, a case of an elderly patient is reported with painful right forearm swelling for three years which progressively increased in size. The size of the swelling was unusually large for glomus tumour. Unfortunately, during the same time period he suffered from acute coronary event. MRI revealed subcutaneously located lobulated soft tissue mass. Surgical biopsy with marginal excision was done. Histopathological examination revealed small uniform rounded cells surrounding capillary vessels, consistent with the diagnosis of glomus tumour. There was no recurrence up to 2 year of follow-up and his cardiac symptoms also stabilised.
Benign lesion, Coronary event, Extradigital, Surgical excision
Case Report
A 66-year-old man with an underlying hypertension for fifteen years was referred to our centre for right forearm swelling which progressively increased in size for the past three years. The swelling was painful especially on touch and cold shower. He had no history of trauma or any constitutional symptoms such as fever, loss of weight and appetite. There was no family history of malignancy or any contact with tuberculosis patient. He gave no history of other swelling elsewhere. The patient had sought medical attention multiple times for the swelling but he was told it was a benign condition and was never further investigated. It was treated symptomatically with analgesics and reassurance. Unfortunately, the patient had accidentally bumped the swelling against the door and experienced an intense pain on the left forearm which triggered a left sided chest pain. The pain was associated with shortness of breath for 2 hours which prompted him to seek medical attention. Serial ECG and cardiac enzyme were done and he was diagnosed with acute coronary syndrome. He was stabilised and then treated medically with anticoagulant Fondaprinux 2.5 mg for three days and Tab. Aspirin 150 mg daily.
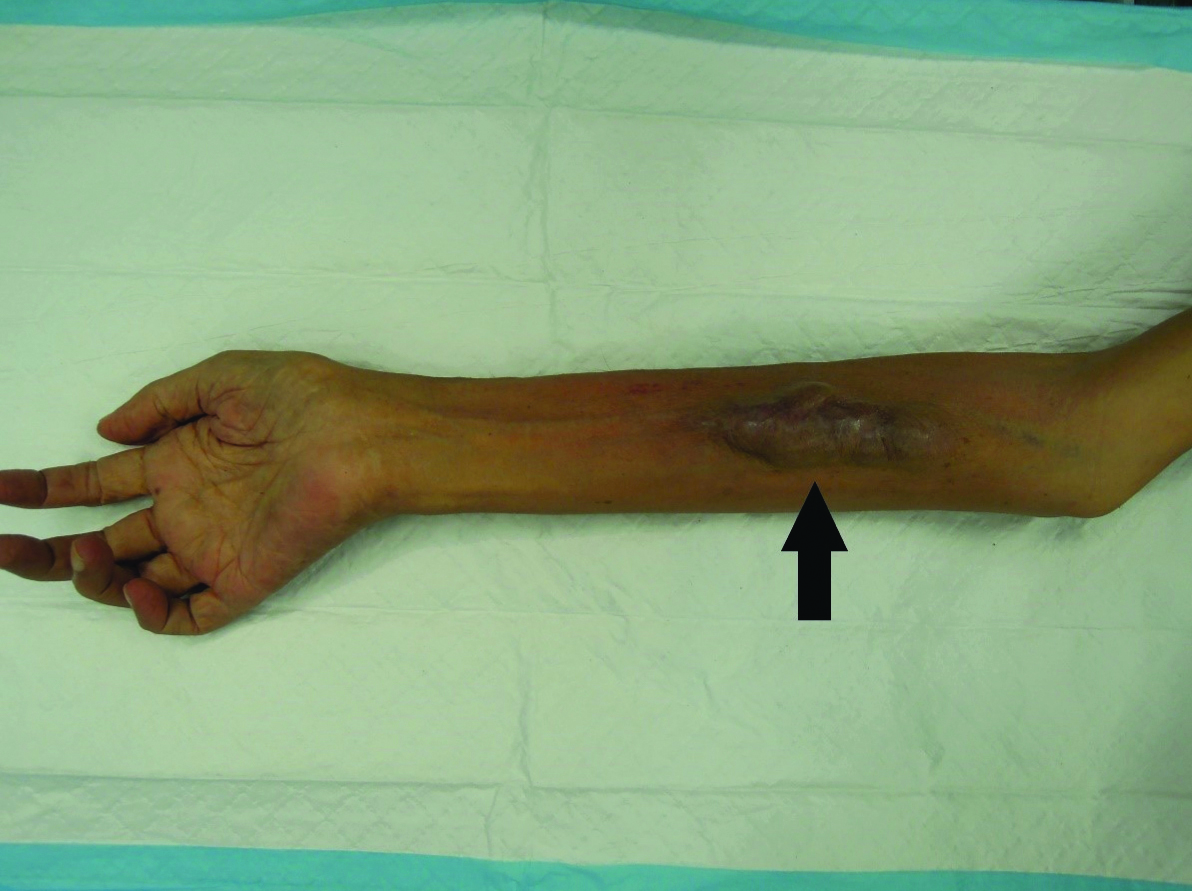
On examination of his right forearm, there was a red-bluish oval shaped swelling measuring 9x3cm on volar aspect of forearm which was soft but exquisitely tender on palpation. The swelling was non pulsatile, not fluctuant, not transilluminable, not warm or erythematous [Table/Fig-1]. Special tests such as Love test and Hildreth test were positive. No other swelling was noted elsewhere.
Clinical picture of the swelling.
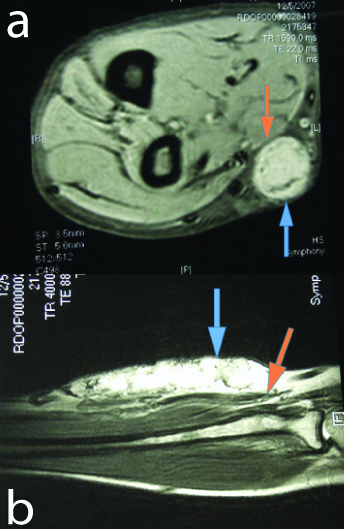
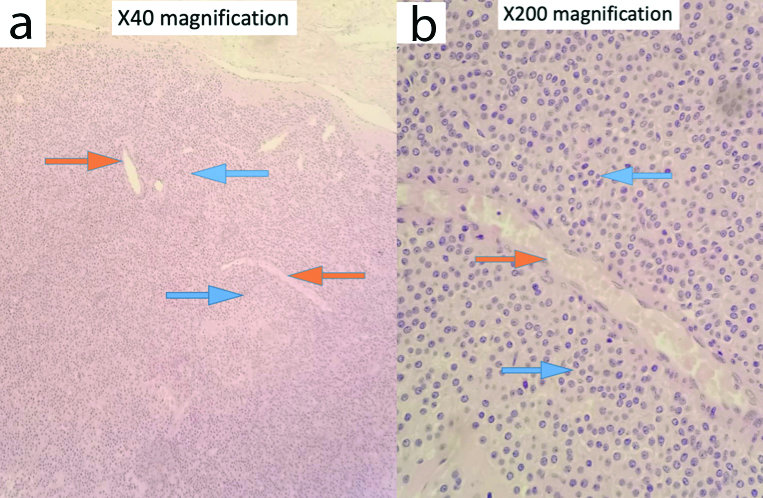
Plain radiography of radius ulnar did not show any calcification of the swelling nor any bony erosion. Initially ultrasound was planned to evaluate the nature and extent of the swelling, however, due to the painful nature of the swelling, the patient could not cooperate in completing the examination. MRI forearm was done and it showed lobulated soft tissue mass at subcutaneous region involving the skin, isointense with muscle on T1 and homogenously enhanced following contrast measuring 1.8×2.3×8.9 cm [Table/Fig-2a,b]. The mass extended superficially to skin and there was no clear fat plane between flexor carpi radialis and palmaris longus tendon. There was no extension into deep fascial layer. Differential diagnosis based from MRI was dermatofibrosarcoma protuberance. He underwent a surgical biopsy and histopathology sample, reported it as Glomus Tumour. It showed nest of lesional cells surrounding capillary vessels. The cells were uniform and rounded with centrally placed nuclei. These were amphophilic to lightly eosinophilic cytoplasm [Table/Fig-3a,b]. On immunochemistry cells were SMA positive, CD34 negative, EMA negative and S100 negative.
Magnetic Resonance Imaging of right forearm in (a) sagittal view and (b) axial view, showing subcutaneously located soft tissue mass involving the skin (blue arrow) and no extension into deep facial layer (orange arrow).
Histopathological examination (Hemotoxylin and Eosin stain) (a) x40 magnification and (b) x200 magnifiation, showing nest of lesional cells with small uniform rounded cells (blue arrow) surrounding capillary vessels (orange arrow).
Marginal excision of the glomus tumour [Table/Fig-4a-c] was done under regional block and the wound was primarily closed. Post operatively wound healing was good and there was no sign of recurrence up to 2 years of follow-up. His cardiac symptoms also stabilised and there was significant postoperative relief.
(a) Intraoperative picture- excision of large glomus tumour; (b) Excised glomus tumour and after tagged. (c) Bisected glomus tumour.

Discussion
Glomus body is a neuromyoarterial apparatus richly located in reticular dermis which regulates blood flow and thermal regulation of the skin [1]. Glomus tumour is a rare benign tumour that could arise from these glomus body. Most glomus tumour described are in subungual region 75-90%, however rare location has been reported such as palm, wrist, forearm, foot, stomach, colon, cervix and mesentery [2]. There are three variant of glomus tumours, most common is solid form (75%) which has poor vasculature and scant smooth muscle component, followed by gloangioma (20%) which has prominent vascular component and glomangiomyoma (5%) which has prominent vascular and smooth muscle component [3]. Though glomus tumours are generally benign, extremely rare malignant glomus tumour has been reported in literature and is termed as glomangiosarcoma [4].
The classic presentation for glomus tumour is triad of paroxysmal pain, exquisite tenderness to touch and cold intolerance. Its appearance is usually reddish-blue in colour and small in size. In general, the mean size varies from 6.1 mm to 6.6 mm [5], while the mean size in the forearm is 13.7 mm [6]. Nevertheless, few authors had described large or giant glomus tumour measuring 30 mm at the fifth ray [7], 65 mm at prepatellar [8], and 50 mm in the wrist [9]. However, in this case the size of the glomus tumour was 75×15 mm which is way larger than the average size described in literature.
Because of pain, most patients tend to present early. However, in literature it has been reported that despite patient had taken medical attention early, most of the initial diagnosis were wrong and there had been delay in the diagnosis. The delayed time for diagnosis ranges from 3.3 to 14.6 years [10]. This could be due to low incidence of this tumour, lack of awareness or suspicion of the attending clinician, or atypical presentation. Fazwi R et al., had highlighted in his case series that the tumour is diagnosed clinically earlier if seen by a resident hand surgeon, which reflect the importance of clinical experience and awareness of diagnosis among treating doctors [10].
This calls for better recognition of glomus tumour. There are few tests that can aid the diagnosis. Aside from the classical triad, Love test can be done by putting pressure to the area with a pinhead which will elicit exquisite pain. Hildreth test is done by inflating tourniquet which reduces pain/tenderness and abolishes tenderness to the Love test, and upon release of tourniquet the pain returns. Love test has sensitivity 100%, accuracy 78%, Hildreth test has sensitivity 77.4% and 100% specificity [11].
There are several imaging that might be helpful to aid in diagnosis. Plain radiography is normal in most cases, although in long standing lesion there could be bony erosion [12].
High frequency ultrasound can be useful. It was described that, when captured in B mode, glomus tumour is seen as small solid, hypoechoic, well defined nodules with regular border, most oftenly in superficial dermis with no involvement in of deep layers [13]. Doppler study would show extensive vascularisation inside the tumour, consistent with vascular lesion such as glomus tumour and pulsed Doppler study usually shows low grade systolic murmur. Ultrasound is especially useful in a small glomus tumour as it is able to detect as small as 1-3 mm lesion which can point-out exactly where the lesion is, to aid surgery and also helpful in differentiating from other nonvascularised tumour [13].
On MRI, because of its vascular nature, it is typically described as well marginated, oval shape and hypointense on T1 and homogenously hyperintense on T2 with hypointense rim [14]. Contrast-enhance CT would show peripheral nodular, strong enhancement in the arterial phase and prolonged enhancement in delayed phase. Christie A and Teasdale E had compared efficiency of multidetector contrast CT and MRI in diagnosis of jugular foramen lesion and found that CT is more accurate than MRI in diagnosing glomus tumour [15].
Histologically, it is described as angiocentric uniform small rounded cells with oval nuclei surrounding blood vessel with lesional cells in background of stellate cells and myxoid matrix which mostly are SMA positive (99%), MSA positive (95%), S100 negative (98%) and CD34 negative (68%) in a case series of 138 cases of glomus tumour by Mravic M et al., [16].
Pain induces stress and stress leads to cardiovascular events but in present case it was incidental or causative factor could not be determined. To our knowledge, there is no similar report of painful glomus tumour which induced angina symptoms, nor any report to show resolution of cardiac symptoms after medical treatment and surgical excision of the tumour.
Current treatment recommendation for glomus tumour is surgical excision. Most surgical excision results in success for pain reduction with documented recurrence rate range from 4% to 15% [17]. Our patient has satisfactory pain relief and most importantly no more symptoms of acute coronary syndrome.
Conclusion(s)
In a lump or swelling associated with exquisite pain with cold intolerance, differential diagnosis of rare glomus tumour needs to be considered. Advanced imaging like computed tomography and magnetic resonance imaging would be helpful in aiding diagnosis and preoperative planning. The recommended treatment is surgical resection which has a good clinical outcome.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 31, 2020
Manual Googling: May 23, 2020
iThenticate Software: Jun 25, 2020 (12%)
[1]. Wheeles CR, Glomus TumourWheeless’s Textbook of Orthopedics 2015 Duke University Medical Center [Google Scholar]
[2]. Muneer M, Alkhafaji A, El-Menyar A, Al-Hetmi T, Al-Basti H, Al-Thani H, Intravascular extra-digital glomus tumour of the forearmJ Surg Case Rep 2016 2016(7):rjw12410.1093/jscr/rjw12427421300 [Google Scholar] [CrossRef] [PubMed]
[3]. Fletcher CD, Unni K, Meretens F, Pathology and genetics of tumours of the nervous system 2002 2002Lyon, France:136-37. [Google Scholar]
[4]. Woodward JF, Jones NF, Malignant glomus tumours of the handHand 2016 11(3):287-89.10.1177/155894471561487427698629 [Google Scholar] [CrossRef] [PubMed]
[5]. Schiefer TK, Parker WL, Anakwenze OA, Amadio PC, Inwards CY, Spinner RJ, Extradigital glomus tumours: A 20-year experienceIn Mayo Clinic Proceedings 2006 81(10):1337-1344.10.4065/81.10.133717036559 [Google Scholar] [CrossRef] [PubMed]
[6]. Sacchetti F, De Gori M, Grossi S, Bonadio GA, Capanna R, An exceptional case of malignant glomus tumour and a review of the literatureActa Orthop Traumatol. Turc 2019 53(4):31310.1016/j.aott.2019.04.01431155303 [Google Scholar] [CrossRef] [PubMed]
[7]. Valero J, Gallart J, González D, Deus J, Lahoz M, Giant glomus tumour and neuroma in the fifth ray: A case reportJ Am Podiatr Med Assoc 2016 106(2):151-54.10.7547/13-14627031555 [Google Scholar] [CrossRef] [PubMed]
[8]. Maxey ML, Houghton CC, Mastriani KS, Bell RM, Navarro FA, Afshari A, Large prepatellar glomangioma: A case reportInt J Surg Case Rep 2015 14:80-84.10.1016/j.ijscr.2015.07.00226254119 [Google Scholar] [CrossRef] [PubMed]
[9]. Chim H, Lahiri A, Chew WY, Atypical glomus tumour of the wrist: A case reportHand Surg 2009 14(02n03):121-23.10.1142/S021881040900434720135739 [Google Scholar] [CrossRef] [PubMed]
[10]. Fazwi R, Chandran PA, Ahmad TS, Glomus tumour: A retrospective review of 15 years experience in a single institutionMalaysian Orthop J 2011 5(3):810.5704/MOJ.1111.00725279028 [Google Scholar] [CrossRef] [PubMed]
[11]. Bhaskaranand K, Navadgi BC, Glomus tumour of the handJ Hand Surg 2002 27(3):229-31.10.1054/jhsb.2001.074612074607 [Google Scholar] [CrossRef] [PubMed]
[12]. Morey VM, Garg B, Kotwal PP, Glomus tumours of the hand: Review of literatureJ Clin Orthop Trauma 2016 7(4):286-91.10.1016/j.jcot.2016.04.00627857505 [Google Scholar] [CrossRef] [PubMed]
[13]. Park HJ, Jeon YH, Kim SS, Lee SM, Kim WT, Park NH, Gray scale and colour Doppler sonographic appearances of nonsubungual soft tissue glomus tumoursJ Clin Ultrasound 2011 39(6):305-09.10.1002/jcu.2083021520136 [Google Scholar] [CrossRef] [PubMed]
[14]. Ham KW, Yun IS, Tark KC, Glomus tumours: Symptom variations and magnetic resonance imaging for diagnosisArch Plast Surg 2013 40(4):39210.5999/aps.2013.40.4.39223898437 [Google Scholar] [CrossRef] [PubMed]
[15]. Christie A, Teasdale E, A comparative review of multidetector CT angiography and MRI in the diagnosis of jugular foramen lesionsClin Radiol 2010 65(3):213-17.10.1016/j.crad.2009.11.00620152277 [Google Scholar] [CrossRef] [PubMed]
[16]. Mravic M, LaChaud G, Nguyen A, Scott MA, Dry SM, James AW, Clinical and histopathological diagnosis of glomus tumour: An institutional experience of 138 casesInt J Surg Pathol 2015 23(3):181-88.10.1177/106689691456733025614464 [Google Scholar] [CrossRef] [PubMed]
[17]. Van Geertruyden J, Lorea P, Goldschmidt D, De Fontaine S, Schuind F, Kinnen L, Glomus tumours of the hand: A Retrospective study of 51 casesJ Hand Surg Eur 1996 21(2):257-60.10.1016/S0266-7681(96)80110-0 [Google Scholar] [CrossRef]