The CAD is a leading cause of morbidity and mortality throughout the world. As per the recently published study the estimated prevalence of cardiovascular diseases in India was 5,681 per 100,000 population in the year 2016 and there were an estimated 62.5 million years of lives lost prematurely due to cardiovascular diseases in India [1]. CCA is an excellent procedure and aid in diagnosis and treatment due to its better spatial and temporal resolution and it can able to do the therapeutic procedures in single and same session, but it has certain risk of complications as it is invasive and mortality rates can vary upto 0.1%. Further at least 20% of the total angiographies are found to be negative thereby increasing the burden on the department in addition to the risk on the patients [2].
Emergence of Multi-Slice Computed Tomography (MSCT) angiography, which is a robust and rapidly evolving technology has challenged the current gold standard i.e., CCA for the evaluation of CAD. The MSCT angiography in addition to the diagnosis of CAD has distinct ability to detect other cardiac and non-cardiac conditions which might be responsible for patient’s symptoms. Majority of previous studies with 64 or lesser slice CT scanner have failed to show consistent and optimal IQ at HR more than 70 bpm and required beta blockers [3,4]. However, with the advent of DSCT many studies have shown further improvement in sensitivity and specificity mainly because of wide Z-axis coverage and better temporal resolution thereby providing better IQ at higher HR [5,6].
Hence the present study was conducted with an aim to evaluate the diagnostic accuracy of 256-slice DSCTA in comparison with CCA in evaluation of CA in patients with clinical suspicion of CAD and to study its effectiveness at higher HR without using beta blockers.
Materials and Methods
The present study was a cross-sectional study conducted in Govind Ballabh Pant Hospital, New Delhi in close collaboration between Department of Radiology and Cardiology from November 2010 to December 2011. A total of fifty consecutive patients which were referred to us with the suspicion of CAD were enrolled in this study after approval from ethical committee (NBE/THESIS/733/2012/7487). However four patients with history of coronary artery bypass graft surgery were excluded. Hence a total of 46 patients were included in the statistical analysis. A written informed consent was obtained after complete explanation of the risk involved during and/or after intravenous contrast administration and radiation exposure during the study.
Patients with history of allergy to iodinated contrast agent, very sick patients who were unable to hold breadth, pregnant women and patients with abnormal renal function test were excluded from the study.
On the basis of HR recording at the time of CT scan the patients were enrolled into three subgroups: 1) Low HR-50-70 bpm (18 patients); 2) Medium HR-71-90 bpm (24 patients); and 3) High HR- ≥91 bpm (8 patients). Blood urea and serum creatinine values were also checked before intravenous contrast administration. No premedication viz., oral or IV beta blocker was used even in patients with higher HR of more than 90 bpm. All the CT examinations were done on a 256-slice, dual source CT scanner (SOMATOM Definition FLASH).
Scanning was done in supine position with the heart in the centre of the gantry (slightly lateral to midline). Hands were lifted above the head to reduce the artefacts from humerii. Table height was adjusted until the horizontal laser (marking the gantry center in y-axis) was located one-third of the way down on the anterior portion of the chest. Central location of the heart in the gantry (in both x- and y-axes) optimises both spatial and temporal resolution. The arm with IV access was kept as straight as possible. The IV line and dual head injector were positioned cranially in such a way that the line did not cross through the gantry thus resulting in streak artefacts. ECG leads were positioned outside the field of view to avoid artefacts from ECG electrodes and cables. In some patients shaving at the site of anticipated electrode placement was required. Breath-hold instructions were practiced by the patient at the time of investigation.
Image acquisition was carried out adhering to ALARA (As Low as Reasonably Achievable) principle, which required thoughtful patient preparation and scanning technique. The scanned volume covered the distance from 1 cm below the carina to just below the diaphragmatic surface of the heart.
Three different scan protocol were used depending upon patients HR: 1) High-pitch spiral scan protocol: Prospective ECG triggering, data obtained in a single heartbeat, was used in patients with regular and low HR (<65 bpm); 2) Sequential scan protocol: Prospective ECG triggering, was used in patients with HR 65 to 75 bpm. The scan window was 40-75% of R-R interval. Depending on the heart size, three or four blocks of images were obtained; 3) Retrospective spiral scan protocol: Retrospective ECG gating with prospective ECG pulsing, was used when HR was more than 75 bpm. Maximum tube current output was applied during 31%-75% of the R-R interval.
Contrast volume was adapted to the scan protocol. The exact volume (V) of contrast agent was calculated using the following equation V= (scan delay + scan time) × flow rate. Contrast agent was given at a flow rate of 5 to 5.5 mL/s, followed by 50 mL of saline solution at the same rate. For timing purposes, automatic bolus triggering technique was used with the Region-Of-Interest (ROI) placed in the descending aorta at carina level. The scanning was started when a threshold of 100 HU was attained. An automatic delay of eleven seconds was added after the desired HU value was attained at the ROI.
In the present study, the slice thickness used was 0.6 mm, increment of 0.4 mm, field of view of 180 mm, and a medium-soft convolution kernel for the reconstruction of CT angiographic data. An additional data set with a sharp convolution kernel was reconstructed in patients with coronary calcifications and stents. The percentage of R-R Interval with best IQ was chosen for image analysis. Image processing and data analysis was performed on a separate workstation using syngo via software. The significant coronary artery stenosis was defined as the luminal narrowing of above 50% [Table/Fig-1] [7].
Grading system for luminal diameter stenosis in CT coronary angiography [7].
| Degree of stenosis | Diameter reduction (%) |
|---|
| Normal | None |
| Minimal | 1-25 |
| Mild | 26-50 |
| Moderate | 51-70 |
| Severe | 71-99 |
| Occlusion | 100 |
American Heart Association (AHA) has provided the 16-segment coronary artery scheme which was used at the time of CT scan data analysis [8]. Two radiologists who have an experience of more than 10 years evaluated the CT coronary angiography images independently and he was not aware of patients clinical history and results of invasive coronary angiography. Axial view, Multiplanar Reformation (MPR) and Maximum Intensity Projection (MIP) on a per-segment, per-vessel basis was used to analyse the images.
IQ was assessed on a score of 1 to 4. Score of 4 denoted excellent IQ, while the score of 1 denoted non diagnostic IQ [Table/Fig-2] [9].
Criteria for assessing Image Quality (IQ) [9].
| Score 1 | Non-discriminable vessel structure or poor image quality with severe artifect. |
| Score 2 | Moderate artifect but assessable on the axial images. |
| Score 3 (Fair) | Good image quality with minor artifect. |
| Score 4 (Excellent) | Excellent image quality |
The CCA was performed using standard angiographic techniques. CCA data was reviewed by two experienced observers (>10 years’ experience), who were blinded to the result of DSCT and patient clinical history. At least two orthogonal projections were used to determine the degree of stenosis. Additional projections were used if necessary. Coronary luminal stenosis in diameter was analysed and recorded visually by two reviewers.
Statistical Analysis
It was performed using a commercial software package (SPSS 17.0 for windows, SPSS, Chicago, IL, USA). The DSCT and CCA were compared on a per-segment and per-vessel basis to determine sensitivity and specificity as well as PPV and NPV for the detection of stenoses of at least 50% diameter reduction. A binomial based proportion analysis was used for patient’s characteristic data. The sensitivity, specificity and accuracy of CTCA were calculated and the differences were compared by using the χ2 test of contingency on a per-segment and per-vessel basis. CCA was taken as the gold standard. Inter-observer agreement of CTCA assessment was performed using kappa analysis (<0.4, poor agreement; 0.4-0.75, fair to good agreement; >0.75, excellent agreement). A p-value of <0.05 was considered to be statistically significant.
Results
Per Artery and Per Segment Analysis
In 50 patients, 690 segments were available, however 4 patients with coronary artery bypass graft and 15 segments of one patient with very high calcium score were excluded. Hence statistical analysis included data from 46 patients and 675 segments.
IQ score was calculated for different segments of RCA, LAD and LCX in three different heart groups. The overall score of a vessel was given by assigning the lowest segment score of that vessel. The mean and SD for different vessels were compared in subgroups. The differences were statistically significant (p<0.05) among all the subgroups. The LCX showed lowest IQ score in each HR subgroup [Table/Fig-3].
Shows combined analysis of IQ score of RCA, LCA and LCX in low, medium and high heart rate groups.
| Heart rate groups | | CT-RCA image quality score | CT-LCA image quality score | CT-LCX image quality score |
|---|
| Group 1Low HR(50-70) | Minimum | 3 | 3 | 3 |
| Maximum | 4 | 4 | 4 |
| Range | 1 | 1 | 1 |
| Mean | 3.88 | 3.88 | 3.76 |
| Std. deviation | 0.332 | 0.332 | 0.437 |
| Median | 4.0 | 4.0 | 4.0 |
| Group 2Medium HR(71-90) | Minimum | 3 | 2 | 2 |
| Maximum | 4 | 4 | 4 |
| Range | 1 | 2 | 2 |
| Mean | 3.65 | 3.70 | 3.30 |
| Std. deviation | 0.489 | 0.571 | 0.801 |
| Median | 4.0 | 4.0 | 3.50 |
| Group 3High HR(≥91) | Minimum | 3 | 2 | 2 |
| Maximum | 4 | 4 | 4 |
| Range | 1 | 2 | 2 |
| Mean | 3.38 | 3.25 | 3.13 |
| Std. deviation | 0.518 | 0.707 | 0.641 |
| Median | 3.0 | 3.0 | 3.0 |
| Total | Minimum | 3 | 2 | 2 |
| Maximum | 4 | 4 | 4 |
| Range | 1 | 2 | 2 |
| Mean | 3.69 | 3.69 | 3.44 |
| Std. deviation | 0.468 | 0.557 | 0.693 |
| Median | 4.0 | 4.0 | 4.0 |
| Std. Error of mean | 0.070 | 0.083 | 0.103 |
In total 675 evaluable segments the overall sensitivity, specificity and NPV were 98.4%, 100%, 99.5 and 95.8%, 100%, 98.6% and 94.3%, 98.4%, 97.6% for three HR subgroups. Out of three arteries RCA reveals highest sensitivity, specificity and PPV in each sub groups.
The inter-reader Kappa values of the low, medium and high HR subgroups for RCA were 0.821, 0.948 and 0.889, respectively which reflect excellent agreement between DSCT angiography and conventional angiography in all three groups. Even patients with higher HRs showed excellent agreement.
In low HR group RCA and LCX showed highest sensitivity, specificity and NPV [Table/Fig-4].
Comparison of diagnostic values among all three Heart Rate (HR)
| | Heart rate | |
|---|
| 50-70 | 71-90 | >91 |
|---|
| RCA |
| Sensitivity | 100% | 95.5% | 90% |
| Specificity | 100% | 100% | 100% |
| PPV | 100% | 100% | 100% |
| NPV | 100% | 98.3% | 95.7% |
| Accuracy | 100% | 98.7% | 96.9% |
| Kappa | 0.821 | 0.948 | 0.889 |
| p-value | <0.001 | <0.001 | <0.001 |
| LMA and LAD |
| Sensitivity | 96.7% | 95.7% | 92.9% |
| Specificity | 100% | 100% | 100% |
| PPV | 100% | 100% | 100% |
| NPV | 99% | 99% | 97.1% |
| Accuracy | 99% | 98.9% | 97.9% |
| Kappa | 0.874 | 0.940 | 0.874 |
| p-value | <0.001 | 0.001 | <0.001 |
| LCX |
| Sensitivity | 100% | 96% | 100% |
| Specificity | 100% | 100% | 96.7% |
| PPV | 100% | 100% | 90.9% |
| NPV | 100% | 99% | 100% |
| Accuracy | 100% | 99% | 98.9% |
| Kappa | 0.909 | 0.935 | 0.941 |
| p-value | <0.001 | <0.001 | <0.001 |
subgroups for detecting ≥50% luminal stenosis using conventional catheter angiography as the reference standard (per segment and per vessel analysis). (The sensitivity, specificity and accuracy of CTCA were calculated and the differences were compared using the χ2 test of contingency on a per-segment and per-vessel basis).
Discussion
CT angiography is a well-established modality for the evaluation of CAD, however many a times its quality suffers because of high HR and often requires administration of beta blockers before the start of the procedure. This study with 256-slice DSCTA showed that excellent IQ can be obtained without using beta blockers even in patients with high HR and it can also provide high diagnostic accuracy in comparison to the current gold standard i.e., CCA.
Image Quality (IQ)
Optimal IQ is an essential prerequisite for the accurate assessment of CAD. This study indicates that even in medium (71-90 bpm) and high HR group (≥91 bpm) patients 256-slice dual source CT could provide good IQ [Table/Fig-5,6]. In all three groups mean IQ score was >3 which corresponds to good IQ [9]. On per-artery, per-segment basis the accuracy in this study compares favourably with results of published studies that used dual source CT [5,7,8]. Donnino R et al., reported that dual-source CT provides significantly better diagnostic IQ than single-source CT despite higher HRs without the use of beta blocker [10]. In an another similar study, Saad MAM and Azer HY, were able to achieve good to moderate IQ in 93% of segments [11].
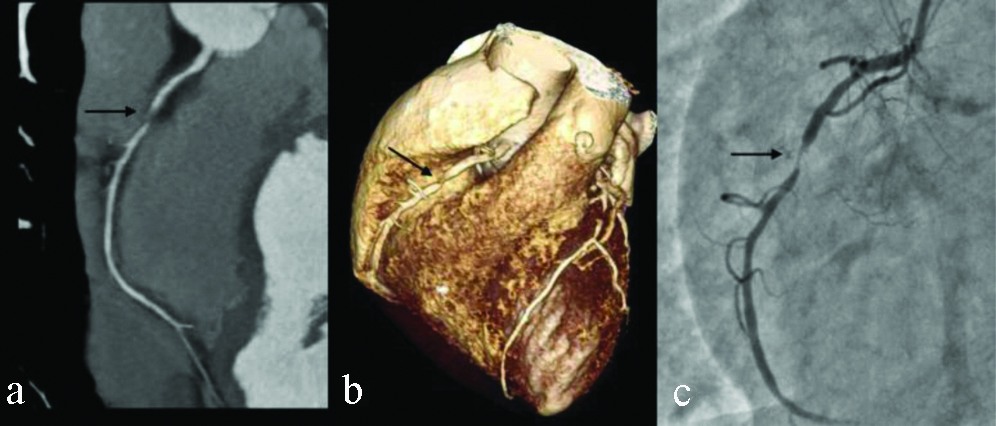
CT coronary angiography in a patient with HR 82 bpm. CT curved MIP (a) and VRT images (b) show an area of severe stenosis (arrow) in mid segment of right coronary artery. Conventional angiogram (c) image shows similar findings (arrow).
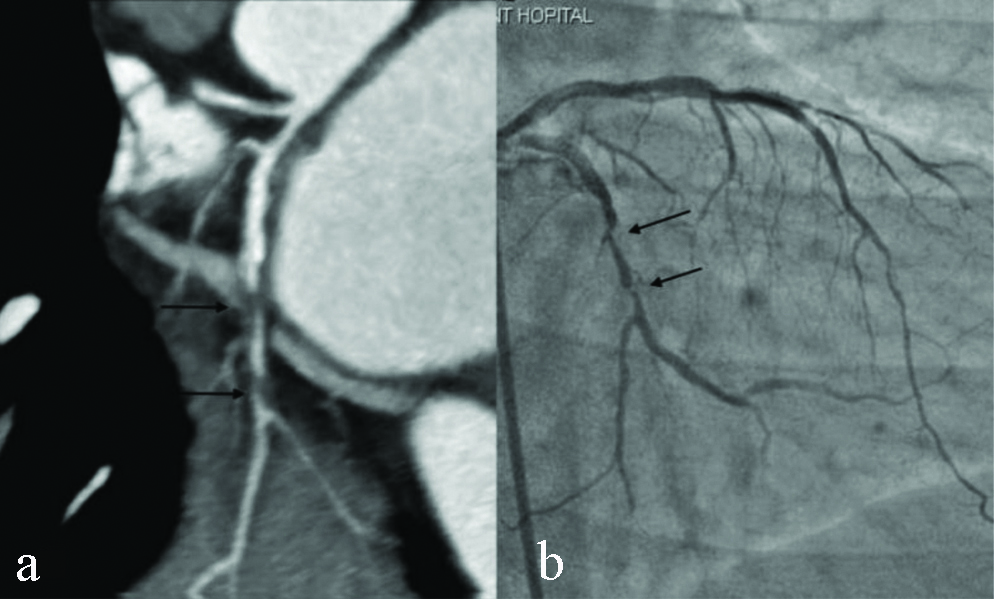
CT coronary angiography in a patient with HR 104 bpm. CT Curved MIP (a) image shows two discrete area of significant stenosis (≥50%) in LCX (arrows). Conventional angiogram (b) shows similar degree and site of stenosis in LCX (arrows).
This study demonstrated that 256-slice dual-source CT angiography can provide a high percentage of evaluable arteries and segments even if no beta blocker was used to reduce the HR. This observation might be a potentially important finding which can help us in its clinical application in those patients who cannot receive specific premedication to lower HR and also in patients whose HR cannot be lowered adequately despite the use premedications. The most likely mechanism for better performance of dual-source CT in patients with high HRs is its higher temporal resolution. The temporal resolution of 75 ms and 0.28 sec gantry rotation time of 256-slice dual source are much better, compared to those of 64 slice CT scanners viz., 120 ms and 330 ms, respectively. In addition 256-slice CT uses mono-segment reconstruction technique when compared to multi-segment reconstruction used by earlier 16 and 64 slice CT scanners.
Accuracy of Lesion Detection
In total, 675 evaluable segments the overall sensitivity, specificity and negative predictive value were 98.4%, 100%, 99.5 and 95.8%, 100%, 98.6% and 94.3%, 98.4%, 97.6% for three HR subgroups. The inter-reader Kappa values of the low, medium and high HR subgroups for RCA were 0.821, 0.948 and 0.889, respectively which reflect excellent agreement between DSCT angiography and conventional angiography in all three groups. Even patients with higher HRs also showed excellent agreement. The findings of this study were in agreement with the previously published studies using dual source CT scanners [12-14].
Several studies had compared the diagnostic accuracy of CT coronary angiography with the conventional catheter angiography [11,15,16]. Matsubara K et al., also reported high diagnostic accuracy of 128-slice DSCTA in the detection of coronary artery stenosis, however they did not correlate the findings with CCA [17].
This study showed significantly high sensitivity in detecting minimal and mild stenosis as compared to CCA mainly due to its improved spatial resolution and better delineation of nonstenotic atherosclerotic lesions. In 50-70, 71-90 and ≥91 HR groups a total of 12 coronary segments with minimal stenosis and three segments with mild stenosis on CT angiography were reported normal with conventional catheter angiography. CT angiography showed better depiction of arteries distal to complete occlusion, which helps the cardiologists in determining the length of stenotic segment in planning appropriate course of management. CT angiography due to its longer injection time and venous phase imaging provide better evaluation of segments distal to complete occlusion in comparison with conventional catheter angiography as venous phase imaging results in retrograde filling of distal segments via collateral circulation. In this study there were two patients with complete occlusion of RCA in whom CT coronary angiography was able to demonstrate distal RCA segments very well compared to conventional catheter angiography [Table/Fig-7,8]. The high temporal resolution of DSCT and improved IQ in patients with high HRs may be especially valuable in patients with acute coronary syndromes in whom there may be no time for HR lowering medication. Another situation where improved temporal resolution of 256-slice dual source CT scores over 16 slice and 64 slice CT scanners is the impaired IQ in presence of severe coronary artery calcification wherein motion and subsequent blurring of calcium leads to frequent false positives in the assessment of degree of stenosis.
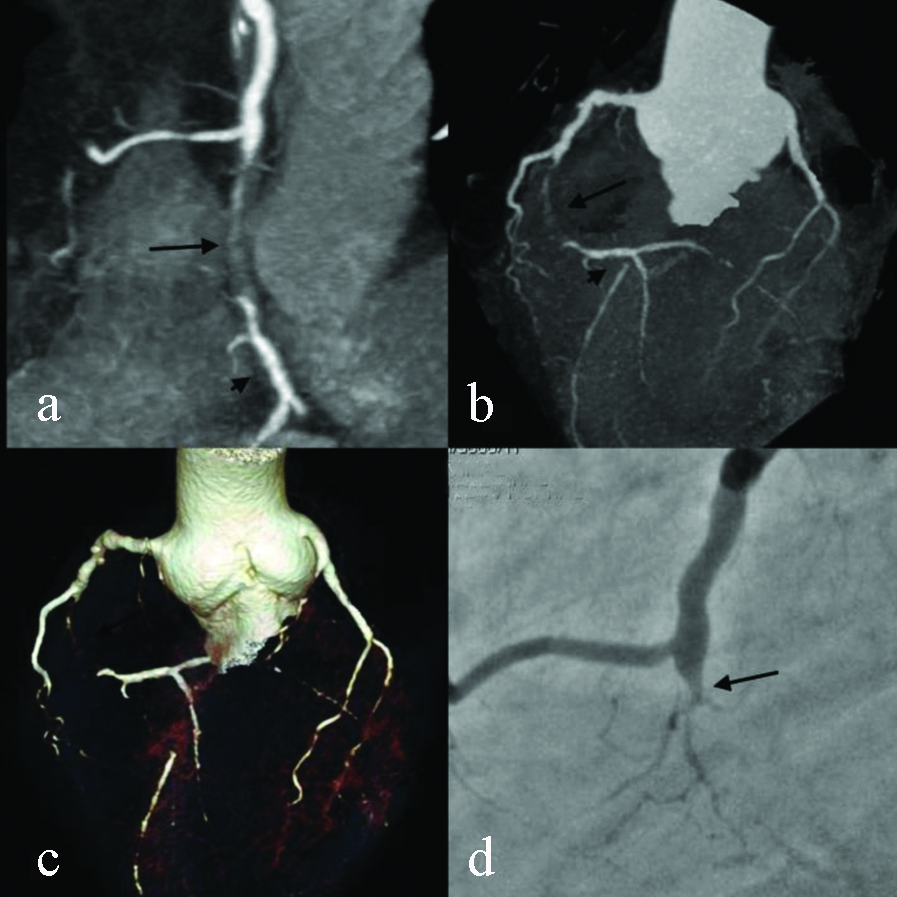
Coronary angiogram in a patient with HR 70 bpm. CT curved MIP (a), triple vessel MIP (b) and VRT (c) images show complete occlusion of mid segment of right coronary artery with soft plaque (arrow) with normal visualised distal RCA (arrow head). Conventional angiogram (d) image shows normal calibre proximal RCA with complete occlusion at same level (arrow) but distal RCA is not well visualised.
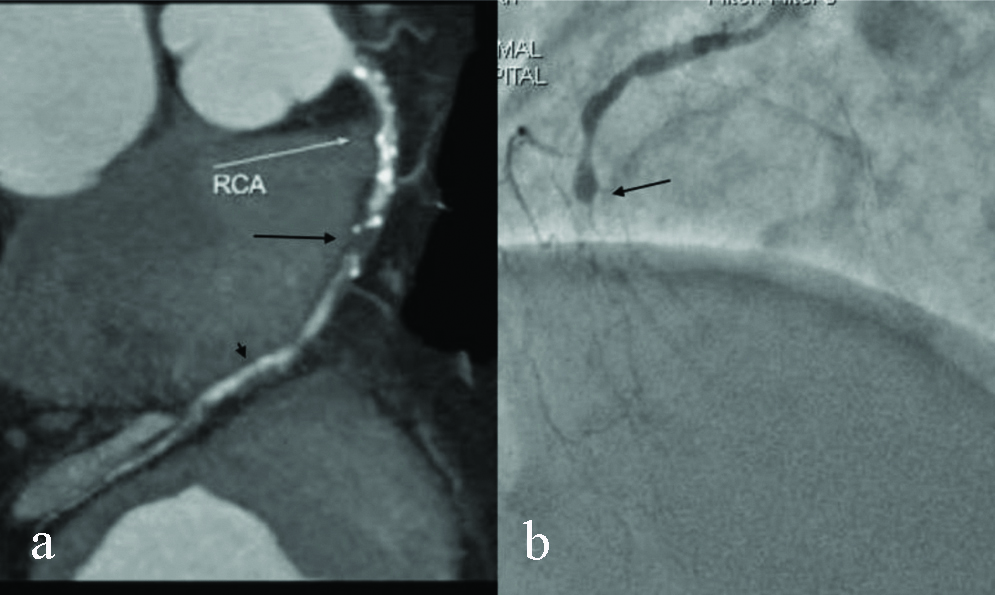
CT coronary angiogram in a patient with HR 97 bpm. CT curved MIP images (a) shows complete occlusion of mid segment of RCA with mixed density plaque (arrow) with normal visualisation of distal RCA (long arrow). Conventional angiogram image (b) shows complete occlusion of RCA at same level, while distal RCA is not visualised.
Limitation(s)
All patients were referred to our centre for catheter angiography; there was a considerable patient selection bias with a prevalence of CAD of 74%. This study excluded patients with acute coronary syndromes as these patients were directly taken up for conventional angiography. Further studies are needed to determine diagnostic accuracy of CT angiography in such patients. Patients with severe aortic and mitral valve stenosis and those with very low ejection fraction showed poor opacification of coronaries, although significant CAD was ruled out with high degree of confidence.
Conclusion(s)
The 256-slice dual source CT coronary angiography is an excellent imaging technique for the evaluation of CAD, which can provide comparable results with conventional catheter angiography in addition to high quality images without the need of beta blocker as a premedication in majority of patients.
Declaration: The abstract of the present manuscript is published in Radiological Society of North America 2012 Scientific Assembly and Annual Meeting, November 25-November 30, 2012, Chicago IL. http://archive.rsna.org/2012/12031989.html Accessed October 3, 2019.