Urethral stricture disease is fairly common in Indian population affecting mainly young to middle aged persons [1]. Aetiological factors include trauma, infection, inflammation and iatrogenic injury to the urethra [2]. BXO is an inflammatory disease of the anterior urethra which affects the prepuce and glans initially [3]. Then, it spreads proximally up to the bulbar urethra and causes severe narrowing of entire urethral lumen [4]. Sometime infective pathology, prior to surgery and repeated urethral dilatations can also cause narrowing of long segment of the urethra [5]. Surgery in the form of substitutional urethroplasty is the treatment of choice of these cases. It can be done either in single or two stage procedure utilising oral mucosal graft [6]. One stage procedure involves the opening of narrow urethra, application of graft and closure of urethra in one sitting; whereas two stage procedure requires completion of last step after a period of 3-6 months [2].
Materials and Methods
Study Design
A prospective observational study was conducted in the Department of Urology, NSCB Medical College, Jabalpur, from 2018 to 2020. Ethical committee approval was not taken, as the study involved observation of routine steps of a surgical procedure. No intervention of any kind or comparison with any other technique was involved. Declarations of Helsinki were followed. Confidentiality of data was maintained and identity of the patients was not disclosed. Patients gave their informed consent for their participation.
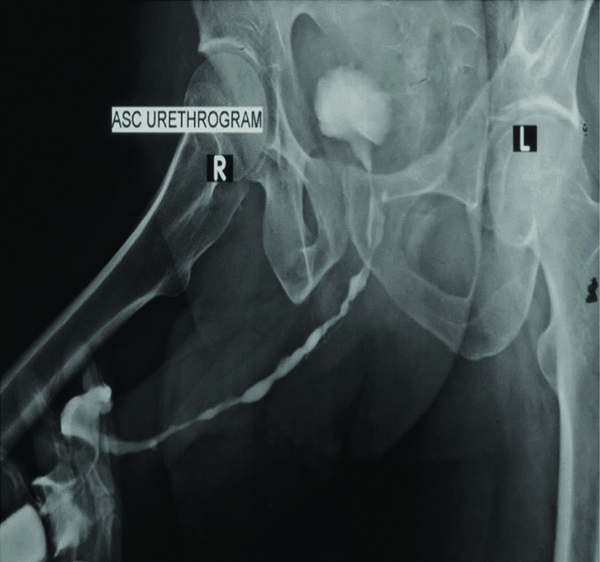
Inclusion criteria: Patients of obstructive voiding symptoms due to urethral stricture disease were included in the study. Forty such patients were screened by history, examination, uroflowmetry, ultrasound and Ascending Urethrogram (ASU). Patients with long segment anterior urethral stricture (>2 cm) on ASU were selected for substitutional urethroplasty with BM [Table/Fig-1].
Ascending urethrogram showing long segment severe narrowing of penile and bulbar urethra.
Exclusion criteria: (a) stricture length <2 cm; (b) planned non-substitutional urethroplasty; (c) planned substitutional urethroplasty with use of tissue other than BM. Finally, 18 patients were enrolled into the study. Data from both single and two stage procedure were taken.
Study Protocol
Baseline clinical data including age, nature of symptoms, duration of symptoms, history of prior surgery, tobacco consumption, aetiology and location of stricture, from all the patients were collected. Oral cavity was examined preoperatively for suitability of application of BMG. Mouth opening was assessed by inter-incisor distance [15]. BM was evaluated for appearance, texture, colour and for presence of any abnormal lesions or fibrous bands. Denture examination included presence of any loose teeth, staining and condition of gingival mucosa. Chlorhexidine mouth wash was given to all patients for cleaning of oral cavity thrice daily three days prior to surgery. Patients were asked to stop smoking or tobacco intake for at least 1 month prior to the surgery. Patients with poor oral hygiene or dental infection were treated by concerned specialist beforehand.
One-Stage Surgical Approach
This was selected based on the ability to insert a 6 Fr infant feeding tube from meatus upto the bladder. It rules out the presence of any tight circumferential stricture, as inferior outcomes have been reported with one-stage procedure in circumferential strictures [16,17]. Substitutional urethroplasty was started in lithotomy position under spinal anesthesia. Midline perineal incision was given. Bulbospongiosus muscle was freed from underlying urethra at one side. Urethra was mobilised from the underlying corpus cavernosa dorso-laterally, as per the Kulkarni technique [18,19]. Urethra was further mobilised upto peno-bulbar junction, depending on the presumed stricture area. If stricture extended into penile urethra also, then penile inversion was accomplished with dissection of penile urethra. Stricture ends were identified with the help of insertion of urethral dilators via both retrograde and antegrade manner. Stricture site was opened dorso-laterally and length of urethral defect was measured with the help of a surgical scale. BMG was applied dorso-laterally and fixed to the underlying corpora with Polyglactin, 4-0 suture. Few sutures for quilting were also placed. Mucosa to mucosa suturing was done on medial side of graft to the urethra; while a mucosa to cavernosal suturing was accomplished on another side, after placement of Foley’s catheter. Bulbospongiosus muscle was re-approximated and incision was closed.
Two-stage Approach
It was chosen in case of inability to pass a 6 Fr infant feeding tube upto the bladder or if there was complete obliteration of long segment of urethral segment on ASU image. These patients first underwent lay open urethroplasty [20]. In which, after the midline incision over penis or perineum, the stricture segment of the urethra was opened ventrally straightaway. A dorsal midline incision was given over the opened up urethra. Incision was deepened via blunt dissection to make space for the graft application. Length and width of the urethral defect were measured. By default, we added 10% in length of urethral defect to get desired BMG length (Preharvest length) in both approaches. Width of graft was taken in such a way to have a total urethral plate width of around 20 mm, in order to get a lumen of 20 Fr after tabularisation. Graft was applied over the dorsal incised part of the urethra. Both sides of opened-up urethra were sutured to the surrounding skin with Polyglactin, 4-0 suture. Periodic assessment of graft taken was done bi-monthly. After a period of 6 months, if graft intake was acceptable, patient was taken for a 2nd stage procedure. In which, two parallel incisions were given along the side of urethral plate to free it from the skin. They were deepened enough to mobilise the urethra. Tabularisation of the urethra was started proximally with Polyglactin, 4-0, round body, running sutures and progressed distally. Surrounding tissue was approximated in the midline to reinforce the urethral closure and skin was closed.
BMG Harvesting
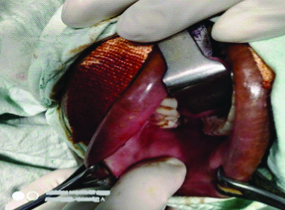
The patient was put under general anaesthesia and an endotracheal tube was kept opposite to the proposed site of BMG in oral cavity [Table/Fig-2].
Oral cavity being prepared, and site inspected for the position of stensen’s duct orifice and the probable donor area.
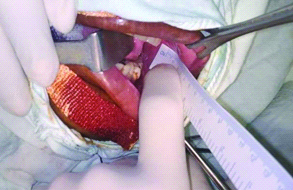
Anesthetist was asked to pack the posterior oro-pharyngeal cavity. After painting of mouth and oral cavity with Betadine 5% solution, draping was done. A desired length and width of BMG was measured over the BM with surgical scale and marked with a surgical pen [Table/Fig-3].
Measurement of BMG being taken over the ink marked area.
A 10 ml of 2% Xylocaine with Adrenaline was diluted with the equal amount of normal saline and the mixture was injected at the site of harvest for the hydro-dissection. BMG was incised along the marked margins and carefully freed from the underlying muscle. After harvesting from oral cavity, BMG was kept in a kidney tray filled with normal saline, until its placement over the urethra. Measurement of length and width of the graft were taken again with the surgical scale [Table/Fig-4].
Postharvest measurement of BMG.

Donor site defect length and width were also measured. Haemostatsis was secured with bipolar electrocautery for small bleeding points and with the under-running of base using Polyglactin, 4-0, RB, suture for large bleed. Donor site was packed with the wet gauze. A donor site closure was optional depending on the surgeon’s choice. It was closed with running sutures catgut 3-0 RB suture in case of an elliptical shaped defect, favouring the closure. Otherwise defect was left open to heal. BMG was defatted and applied over the dorsum of the urethra. Postoperatively, patients were asked to apply ice pack application over the side of cheek. Patients were instructed for repeated mouth wash with Chlorhexidine and to drink cold fluids from the next day morning. They were also instructed to start gentle tooth brushing after 2 days of surgery.
Statistical Analysis
Basic patient data as stated in the study protocol was assessed. Preharvest size of BMG was taken from the ink marked measurements over the BM. Postharvest BMG size was measured immediately after the graft removal with the surgical scale. Donor site defect area was also measured similarly. All three measurements were put in a tabulated form. Pre- and postharvest size of BMG as well as donor site were compared using a paired t-test. Alterations in tobacco and non-tobacco users were compared using an unpaired t-test. Descriptive data were presented in the form of mean, range, percentage and standard deviation. Statistical analysis was completed using Statistical Package for the Social Sciences (SPSS) software, version 21.0 (IBM Corp, NY, USA). Statistical significance was kept below 0.05.
Results
Baseline Characteristics
There were 18 patients finally available for analysis. Mean age of the study participants was 32.9±14.2 years. Two third of the patients had obstructive voiding symptoms for more than 6 months [Table/Fig-5]. BXO was the most common causative factor found in 61.1% of the cases. Three patients had a history of prior reconstructive surgery. Pan-anterior stricture was found in half of the cases. About 61% patients consumed tobacco in some form.
Baseline characters of the study population.
| Variables | Frequency (n=18) |
|---|
| Age (years) | 32.9±14.2 (16-65) |
| Duration of symptom (months) | 8.3±3.7 (3-18) |
| ≤6 months | 6/18 (33.3%) |
| >6 months | 12/18 (66.7%) |
| Symptoms |
| Poor flow | 16/18 (88.9%) |
| Straining | 12/18 (66.7%) |
| Incomplete emptying | 12/18 (66.7%) |
| Frequency | 10/18 (55.5%) |
| Nocturia | 8/18 (44.4%) |
| Aetiology |
| BXO* | 11/18 (61.1%) |
| Infectious origin | 4/18 (22.2%) |
| Iatrogenic | 2/18 (11.1%) |
| Repeated dilatations | 1/18 (5.5%) |
| Tobacco consumption | 11/18 (61.1%) |
| Prior surgery | 3/18 (16.7%) |
| Location of urethral stricture |
| Penile | 5/18 (27.8%) |
| Bulbar | 4/18 (22.2%) |
| Bulbo-penile | 9/18 (50.0%) |
*Balanitis xerotica obliterans
BMG Shrinkage Assessment
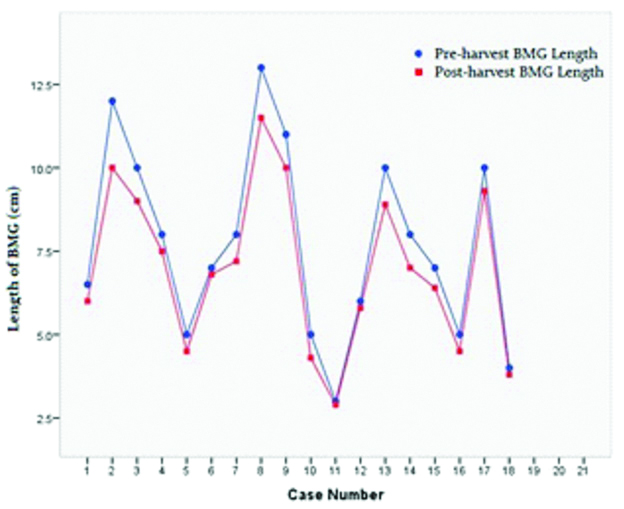
Single stage (dorso-lateral onlay) substitutional urethroplasty was performed in 10/18 cases. Rest eight underwent lay open urethroplasty. Mean pre and postharvest BMG sizes were 7.7×1.8 cm and 6.9×1.6 cm, respectively [Table/Fig-6].
Characteristics of BM graft and donor site area along with comparison of pre and postharvest measurements.
| Variables | Frequency (n=18) | p-value |
|---|
| Side of Inner cheek |
| Left | 8 (44.4%) | |
| Right | 5 (27.8%) | |
| Both | 5 (27.8%) | |
| Donor site closure |
| Yes | 5 (27.8%) | |
| No | 13 (72.2%) | |
| BMG thickness | 3.0±0.7 (2.0-4.2) | |
| Preharvest length of BMG# (cm) | 7.7±2.8 (3.0-13.0) | <0.001** |
| Postharvest length of BMG (cm) | 6.9±2.4 (2.9-11.5) |
| Overall | 8.8±3.8% |
| % Decrease in length of BMG after harvest | Tobacco user | 7.2±2.9% | 0.02* |
| Non-tobacco user | 11.3±3.7% |
| Preharvest width of BMG (cm) | 1.8±0.2 (1.5-2.0) | <0.001** |
| Postharvest width of BMG (cm) | 1.6±0.2 (1.2-2.0) |
| Overall | 10.8±5.7% |
| % Decrease in width of BMG after harvest | Tobacco user | 10.9±4.7% | 0.95 |
| Non-tobacco user | 10.7±7.5% |
| Preharvest donor site length (cm) | 7.7±2.8 (3.0-13.0) | 0.003** |
| Postharvest donor site length (cm) | 7.9±2.9 (3.1-13.4) |
| Preharvest donor site width (cm) | 1.8±0.2 (1.5-2.0) | <0.001** |
| Postharvest donor site width (cm) | 2.0±0.3 (1.6-3.0) |
| Preharvest donor site area (cm2) | 13.8±5.8 (4.5-26.0) | <0.001** |
| Postharvest donor site area (cm2) | 16.4±7.2 (5.0-31.0) |
| Overall | 18.5±14.8% |
| % Increase in donor site area after harvest | Tobacco user | 18.5±16.3% | 0.98 |
| Non-tobacco user | 18.4±13.4% |
Student t-test paired and unpaired; #Buccal mucosal graft (BMG); *Statistically significant;
**Statistically highly significant
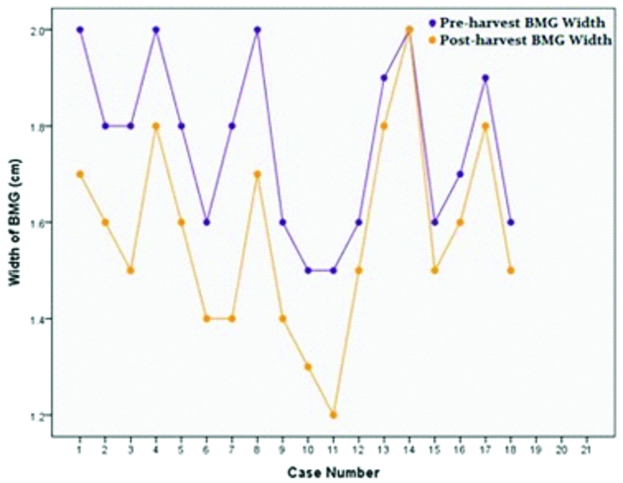
An 8.8% decrease in length and 10.8% decrease in width of BMG were discovered after harvesting, which were statistically significant (p<0.001) [Table/Fig-6]. Tobacco users had a lesser percentage decrease in length than non-tobacco users (7.2% vs 11.3%, p=0.02*), while no such difference was observed in width alteration (10.9% vs 10.7%, p=0.95). Donor site length and width were 7.9±2.9 and 2.0±0.3 cm, respectively. Increase in donor site area after graft harvesting (13.8 cm2 vs 16.4 cm2) was also statistically significant (p<0.001**). Similar degree of donor site alterations were not noted among tobacco and non-tobacco users (p=0.98). Line charts showing a decrease in postharvest length and width of the BMG [Table/Fig-7 and 8].
Line chart showing a decrease in postharvest length of the BMG.
Line chart showing a decrease in postharvest width of the BMG.
Discussion
Substitutional urethroplasty has changed the management of long segment stricture of urethra substantially [21]. Use of the grafts not only provides a replacement to the scarred and narrowed urethral lining, but also produces durable outcomes [22]. BMG has sustained its good efficacy, since its initial description in the urethroplasty in late 19th century by Kirill Sapezhko, from Ukraine [23]. But only after the reports of two pediatric surgeons Burger RA et al., and Dessanti A et al., it could gain popularity widely [24,25]. Postoperative shrinkage of BMG in urethra has been reported widely in follow-up studies. Barbagli G et al., reported a failure rate of 22.3% in his 282 patients of BMG urethroplasty after a median follow-up of 118 months [21]. Levine LA et al., found a failure rate of 19% in his 53 patients at median follow-up of 52 months [9].
Breyer BN et al., and Kessler TM et al., described many reasons for the sub-optimal result of BMG such as prior urethrotomies, prior surgery, smoking, history of urethral stent placement, etc., [26,27]. In present opinion, an undue intraoperative stretching of BMG during application may also be responsible for this partially. It may arise from the shrinkage of BMG immediately after harvesting. This graft over stretching can widen the urethral lumen initially, but in long term graft can shrink rapidly, especially after removal of the catheter. Prior knowledge of extent of immediate shrinkage of BMG can give the surgeon a thought to harvest an extra size of BMG. To some extent, shrinkage can be dealt by spreading and suture fixation of the graft. However, this can be challenging, if the size of urethral defect is large as the complexities of surgery increase with increasing stricture length [6,28,29].
In this study, an 8.8% decrease in length and 10.8% decrease in the width of the BMG. An extra 10% of the length of the graft due to the prior experiences with urethroplasty surgeries was already taken. Due to this, it was possible to place in a firm but relaxed position. An extra length can probably compensate for the shrinkage of BMG after harvesting. This was nearly equal to the percentage decrease in size of BMG, in present case. A significant degree of effect of tobacco consumption on alteration in graft length was noticed. Tobacco users showed lesser shrinkage in length than the non-tobacco users. Reason may be some amount of loss of elastic tissue in BMG, after prolonged tobacco consumption [30,31]. Zain RB et al., described various lesions of oral mucosa affected by tobacco chewing, such as chewer’s mucosa, submucous fibrosis, lichenoid lesions etc., [32].
An increase in donor size area after graft harvesting was also noticed. Reason may be the inherent elasticity of the BM. This might interfere with the closure of the donor site, along with the shape of the donor site area. Closure however mainly depends on the shape, as suggested by Barbagli G et al., [33]. An elliptical shape helps in the closure, while a rectangular shape doesn’t [33]. The present study only close it in their five out of 18 cases, due to the elliptical shaped defect. Reasons for non-closure in majority of present cases were more rectangular shaped defects and refraining from the closure with a tension over suture line. Recently, studies of Wood DN et al., and Rourke K et al., have supported the view of leaving the donor site open [34,35]. This can rather decrease the postoperative pain and lessen the restriction in mouth opening later. Reason for this may be the undue traction over the mucosa after closure of a large defect [36]. Leaving the donor site open saves the operative time. This approach can also allow the surgeon to take a little extra size of the graft, without worrying about the need for closure [35]. It is important, especially while contemplating around 10% of shrinkage of BMG after harvesting.
Limitation(s)
Limitations of this study were small sample size, lack of group comparisons and no correlation with the clinical outcome. Conclusive effect of tobacco on BMG shrinkage is also difficult to make due to limited number of cases, variation in duration and form of tobacco intake. A larger study with stratification of all these factors may give the right answer.
Conclusion(s)
Based on the findings of present study, it was found that BMG shrank to about 9% in the length and about 11% of the width, immediately after harvesting from the oral cavity. An increase in the donor area is also noted after the graft removal. This study suggested taking an extra 10% of the measured urethral defect size, in order to adjust for the expected shrinkage. Donor area can be left open, if repair is difficult and the suture line appears to be in tension.