Ostomy operations are often carried out for diversion related to colon cancer and inflammatory bowel diseases. Mostly, ileostomy and colostomy are applied and the application can be in the end or loop form. Even though stoma formation is considered technically simple, it can lead to very complex and serious complications. Specifically, in cancer patients, wound healing is seriously impaired due to sarcopenia resulting from tumour-related catabolism and hypoproteinaemia. In these patients, serious problems can be experienced in wound care of the wounds which are closely associated with ileostomy or colostomy [1,2]. The incidence of peristomal skin complications vary between 18 and 73% [1-4]. Loop ileostomies are particularly responsible for the majority of the peristomal skin complications [5]. Peristomal skin complications can occur in a variable spectrum such as peristomal dermatitis, parastomal ulceration, pyoderma gangrenosum, mucocutaneous separation, ostomy dehiscence and stercoral fistulas [6]. Although they usually occur within the first two weeks after the stoma formation, they may also emerge as late complications, months and even years after the first surgery. Even though the causes of peristomal skin complications change, the common issue is the leakage from the stoma bag. The risk of peristomal skin complications is higher in patients whose stoma are not placed properly (especially in obese patients) [7]. In particular, the development of the complications such as deep mucocutaneous separation, ostomy dehiscence and pyoderma gangrenosum in patients seriously affects their quality of life.
The VAC treatment is used commonly in closing the open abdominal wounds and in the treatment of stoma dehiscence [8]. VAC is a system which was first introduced in the literature by plastic and reconstructive surgeons in 1997 [9,10]. The VAC treatment is used in many diseases such as chronic leg ulcers, diabetic foot wounds, patients with burn injuries, postoperative trauma or wound infections after vascular surgery and open abdominal management [11]. The VAC system has many influential mechanisms such as reducing tissue oedema, bacterial colonisation and wound tension, increasing blood flow, wound granulation and angiogenesis in the wound by applying controlled negative pressure [12]. The complications in association with the VAC treatment are encountered very rarely and they are limited to pain and allergic reactions to the cover, if no analgesia is applied in case of superficial bleeding that usually occurs following the change of the sponge. Despite the available case report in the literature with respect to the use of the VAC system in parastomal wounds [8], there are no large-scale studies. In this study, the aim is to investigate the risk factors affecting the duration of wound healing in wounds related to stoma and resulting in problems in the stoma care and the effect of the VAC system on the duration of wound healing in cancer patients, who constitute a group open to infections and various complications.
Materials and Methods
Inclusion criteria: Total of 38 patients, were operated with the diagnosis of intra-abdominal malignancy in the department of surgical oncology between January 2010 to January 2018, underwent stoma formation and had parastomal wound development (such as deep mucocutaneous separation and ostomy dehiscence) were included.
Exclusion criteria: Among them seven patients with insufficient data were excluded. Hence, 31 patients were evaluated retrospectively. The study was approved by Ankara University, Faculty of Medicine, Human Research Ethics Committee (Decision Number: 11-32-20; date: January 16, 2020). The power of statistical tests, in which the effect of VAC treatment on wound healing time was examined, was determined as 0.76 {sample size: 31 (17 vs 14); df: 29; critical t: 2.04} in Gpower version 3.1.9.7 analysis.
A restrospective study was conducted. The patients’ demographic (age, gender, BMI) and clinical data, comorbidities (DM, COPD), stoma-related information (ileostomy, colostomy) and complications and the applied treatment methods were determined from the hospital database and patients’ files. The effect of the patient-related factors and the VAC treatment on the duration of wound healing was analysed.
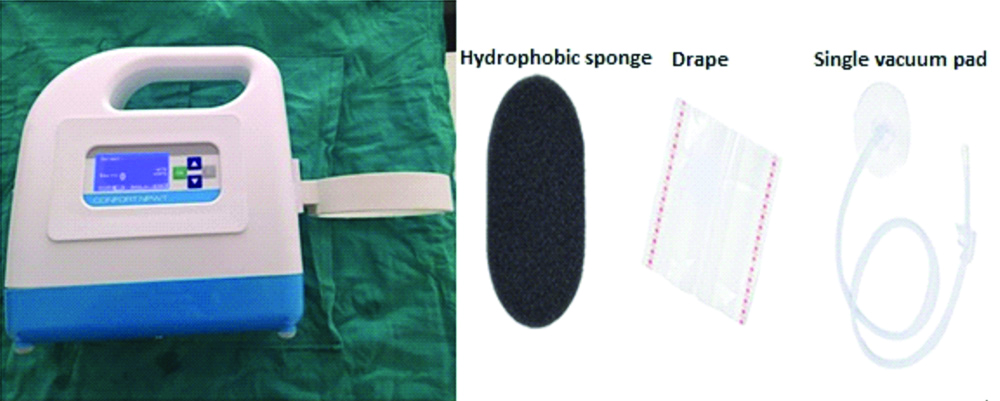
Method of VAC application: Wound was debrided, irrigated with normal saline and peri-wound skin was made dry. Sterile black foams (Polyurethane ether, lighter, hydrophobic with a pore size of 400-600 mm) was used for dressing in all cases. A fenestrated evacuation tube was fixed in the foam, which was connected to a vacuum pump. The wound was then sealed with an adhesive drape. The dressing was usually changed on the 3rd day. Low continuous negative pressure mode (50-75 mmHg) was used. The VAC device used in the study and its parts are shown in [Table/Fig-1].
VAC device and its parts.
The relation between clinical, demographic data, parastomal wound treatment methods (VAC and non-VAC conventional wound therapy) and the duration of wound healing were reviewed.
Statistical Analysis
All numerical data were expressed as mean±Standard Deviation (SD). For comparing the patient related factors and treatment type with wound healing duration, student t-test was used. All the p-values less than 0.05 were considered statistically significant. These analyses were performed using IBM Statistical Package for the Social Sciences (SPSS) statistical version 23.0.
Results
A total of 31 patients who were included in the study and developed parastomal wounds, 10 (32.2%) were men. The mean age was found as 51.77±15.23. There were 20 patients with ileostomy and 11 patients with colostomy. In the patient population, the diagnosis was colorectal cancer in 28 patients. In the remaining three patients, the diagnosis was ovarian cancer.
While the VAC treatment was applied to 14 (45.2%) patients, the others were applied conventional wound care methods. In patients who received the VAC treatment, minimum four and maximum eight sessions of treatment were applied.
The effect of being above 65 years of age (p=0.044), presence of DM (p=0.012) and having a BMI value of 25 or above (p=0.046) on the duration of parastomal wound healing was found to be statistically significant. Also, the effect of using VAC treatment (p=0.016; 95% CI: 1.37~12.23) instead of other conventional wound treatments on the duration of parastomal wound healing was found to be statistically significant [Table/Fig-2].
Demographic data and the relationship between treatment type and wound healing times.
| Variables | Total (n/%) | Wound healing time (days) (mean±standard deviation) | 95% CI† | p-value |
|---|
| Gender |
| Men | 10 (32.2) | 46.50±11.31 | - | 0.656 |
| Woman | 21 (67.7) | 44.52±11.48 |
| Age |
| >65 age | 8 (25.8) | 52.00±13.54 | 0.24~18.18 | 0.044 |
| <65 age | 23 (74.2) | 42.78±9.60 |
| COPD* |
| Present | 5 (16.1) | 44.00±10.24 | - | 0.806 |
| Absent | 26 (83.9) | 45.38±11.64 |
| DM** |
| Present | 11 (35.5) | 51.82±8.14 | 2.43~18.20 | 0.012 |
| Absent | 20 (64.5) | 41.50±11.23 |
| BMI (kg/m2) |
| >25 | 14 (45.2) | 49.57±12.93 | 0.14~15.93 | 0.046 |
| <25 | 17 (54.8) | 41.53±8.46 |
| Neoadjuvant therapy |
| Present | 9 (29) | 46.09±10.77 | - | 0.482 |
| Absent | 22 (71) | 42.89±12.80 |
| Treatment method |
| VAC | 14 (45.2) | 39.29±11.55 | 1.37~12.23 | 0.016 |
| Non-VAC | 17 (54.8) | 50.00±8.66 |
*COPD: Chronic obstructive pulmonary disease, **DM: Diabetes mellitus, †CI: Confidence interval
Student-t test was used for all variables; VAC: Vacuum-assisted closure; BKMI: Body mass index
The condition of the parastomal wound before VAC and the healing process after VAC use are shown in [Table/Fig-3,4].
Parastomal wound and VAC application.
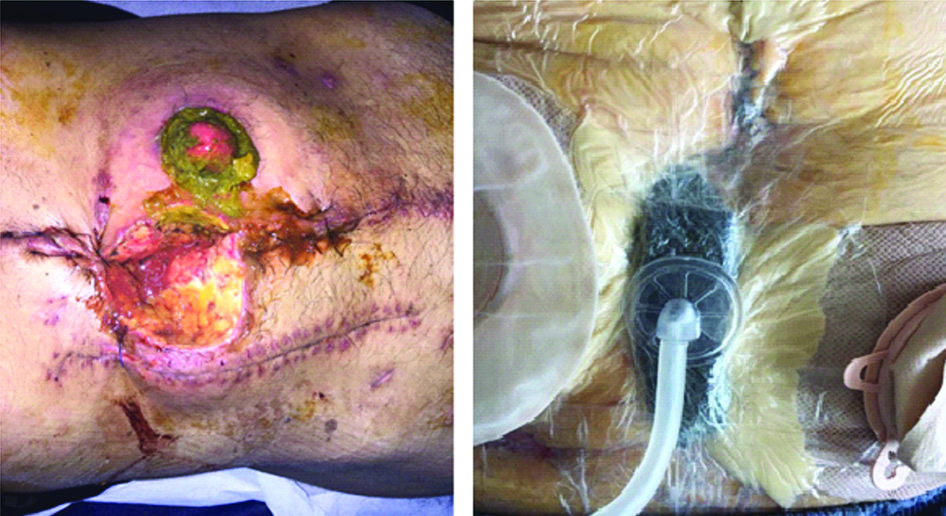
Healing process after VAC application.

Discussion
Colorectal cancer is the most common indication for the stoma formation [13-16]. Since stoma formation is technically a cheap procedure, it is carried out by young surgeons in general, however, various complications may occur, affecting the patient’s quality of life and increasing the financial costs in the healthcare system. Among these complications, parastomal skin complications come to the fore. Today, the VAC system is commonly used in closing open abdominal wounds and in the treatment of stoma dehiscence. In the literature, there are no studies conducted on the use of the VAC treatment in parastomal wounds which deteriorate the patients’ quality of life, such as mucocutaneous separation and stoma dehiscence. There is only one case report on this subject [8].
The effect of being above 65 years of age and having a BMI value of 25 and above on parastomal wound healing was found to be statistically significant. There are different results in the literature regarding the effect of age factor on the development of parastomal skin complications and wound healing duration. In some studies, it is seen that the age factor does not affect the development of parastomal wounds [17,18], and in other studies, patients below the age of 65 have more parastomal skin complications [5]. In this study, age above 65 had a negative impact on parastomal wound healing and wound healing lasted significantly longer in this group of patients. This result has been linked to the more difficult adaptation of elderly patients to stoma care. In this study, when the BMI was 25 and above, wound healing was negatively affected and parastomal wound healing in this group of patients lasted significantly longer. In line with this result, there are similar studies in the literature which suggest that when the BMI is 25 and above, the parastomal wound healing time is prolonged [19,20]. Although high obese patients, have high risk of wound and cardiopulmonary complications, they also have many difficulties in terms of stoma formation and management. In obese patients, stoma-related complications are as high as 36%, so obesity is considered an important risk factor for stoma failure [21]. In the study conducted by Thomas EJ et al., the rate of wound infection was found to be high in overweight patients undergoing abdominal surgery [22]. In their study, Leenen LP et al., reported more frequent stoma necrosis associated with the traction in the intestinal mesentery in obese patients [21]. The development of necrosis in the stoma is one of the most significant reasons causing mucocutaneous separation. In patients with high BMIs (especially obese), the improper placement of the ostomy device leads to ostomy retraction, leakage from ostomy, frequent exposure of the parastomal wound to the intestinal contents and consequently, prolonged wound healing time [7].
In present study, the effect of the presence of DM on parastomal wound healing was found statistically significant. Parastomal wound healing took a longer time in these patients. There is similar information in the literature stating that the presence of DM impairs wound healing and leads to mucocutaneous separation in stomata [7,19,23].
When the VAC treatment and other conventional wound treatment methods were compared, the length of hospital stay was found to be short statistically and significantly in the VAC group. Traditional wound care treatments such as frequent changing of the dressings, resuscitation of the ostomy that underwent dehiscence, debridement of the wound and the use of paste or powder to protect the wound were applied to the patient group without the VAC treatment for parastomal wound management. Regarding deep parastomal wound (deep mucocutaneous separation) management, there is information in the literature about various methods such as calcium alginate or hydrofibre wound dressings, simple wound care, debridement or abscess drainage. However, there are unfortunately no studies comparing the effectiveness of these methods. In the treatment of deep mucocutaneous separation, calcium alginate or hydrofibre wound dressings have also been recommended recently for filling the dead space in the wound bed [24]. Alginate and hydrofibre wound dressings turn into a soft material that provides debridement when they contact exudate and allows for granulation by providing a moist environment. There are many studies available in the literature on the use of the VAC-assisted treatment that positively affects complex wound healing [25-29]. In the studies, for difficult wound management, the VAC treatment is considered superior in reducing the wound depth and volume, shortening the treatment duration and decreasing the costs compared to the conventional wound care [30]. The application of negative pressure diminishes the wound oedema and bacterial burden, improves the tissue perfusion and stimulates the granulation tissue and angiogenesis. Cirocchi R et al. stated that there was a significant decrease in the duration of intensive care and 30-day mortality rate of the patients who received the VAC treatment in the open abdominal technique, and their rate of complications such as enteroatmospheric fistula, postoperative abscess and bleeding reduced [31]. In the present study, the length of hospital stay was found to be short statistically and significantly in the VAC-applied group. Thus, the advantage of the VAC treatment is that, it protects the parastomal wound area from the ostomy content which irritates it and quickens the formation of the granulation tissue.
Limitation(s)
This study has some limitations. Firstly, this study is not a prospective randomised study, but a retrospective monocentre analysis. Secondly, the sample size is small. Because the stomas were formed by different surgeons, the complication rates may have been influenced by this fact as well.
Conclusion(s)
Presence of DM, age above 65, BMI of 25 and above negatively affect the duration of parastomal wound healing in malignant patients and prolongs the duration of parastomal wound healing. VAC treatment is an easy method and can be used effectively in parastomal wounds. Parastomal wound healing duration in patients with VAC is shorter than in other conventional methods. The results of this study can be used to predict parastomal skin complications and to improve the management of these complications. Although the present study sheds light on this issue, further studies with randomised, prospective and more sample size are needed to discuss the effectiveness of VAC treatment in the process of parastomal wound healing.
*COPD: Chronic obstructive pulmonary disease, **DM: Diabetes mellitus, †CI: Confidence interval
Student-t test was used for all variables; VAC: Vacuum-assisted closure; BKMI: Body mass index