External Root Resorption (ERR) is a pathological condition that can lead to tooth loss if not diagnosed and treated correctly. Calcium Hydroxide Ca(OH)2 is an intracanal medicament, which is used in cases of teeth with pulp necrosis, peri-radicular lesions and ERR. This paper describes the endodontic management of a tooth with severe ERR using injected non-setting Ca(OH)2 paste. A 28-year-old patient was referred for endodontic evaluation of tooth 47, which presented an extensive composite resin restoration and was negative to cold test. Panoramic and periapical radiographs revealed the presence of a filled pulp chamber, calcified root canals, ERR on the mesial and distal roots, and apical periodontitis in the mesial and distal roots. The diagnosis of asymptomatic apical periodontitis and severe ERR was established, and conventional root canal treatment combined with non-setting Ca(OH)2 dressing was chosen. After five months, no more discharge from the root canal was observed, and a decrease in the size of the periapical lesion and arrest of ERR was detected. The root canal was filled, and the patient was referred for restoration. At the 6-months follow-up, radiographic examination evidenced periapical repair and containment of the ERR process. Chemomechanical root preparation in association with a non-setting Ca(OH)2 dressing protocol allows positive outcomes during the management of severe ERR associated with pulp necrosis and periapical inflammation.
Case Report
A 28-year-old male patient was referred for endodontic evaluation of tooth 47. The referral was made after a panoramic radiographic examination for planning third molar removal, revealed the presence of apical radiolucency around the mesial root of tooth 47 [Table/Fig-1a]. The patient’s previous medical history was noncontributory. The patient reported that the tooth 47 had undergone root canal treatment nearly 15 years ago, and no symptoms had been noted since then.
(a) Initial radiographic examination showing an unerupted and impacted lower right third molar (tooth 48) and a lower right second molar (tooth 47) with filled pulp chamber and periapical pathology associated to external root resorption ERR; (b) Clinical view of tooth 47 showing an extensive composite resin restoration; (c) Radiograph of tooth 47 showing calcified root canals, periapical lesion in both roots, and severe apical resorption in the mesial root.
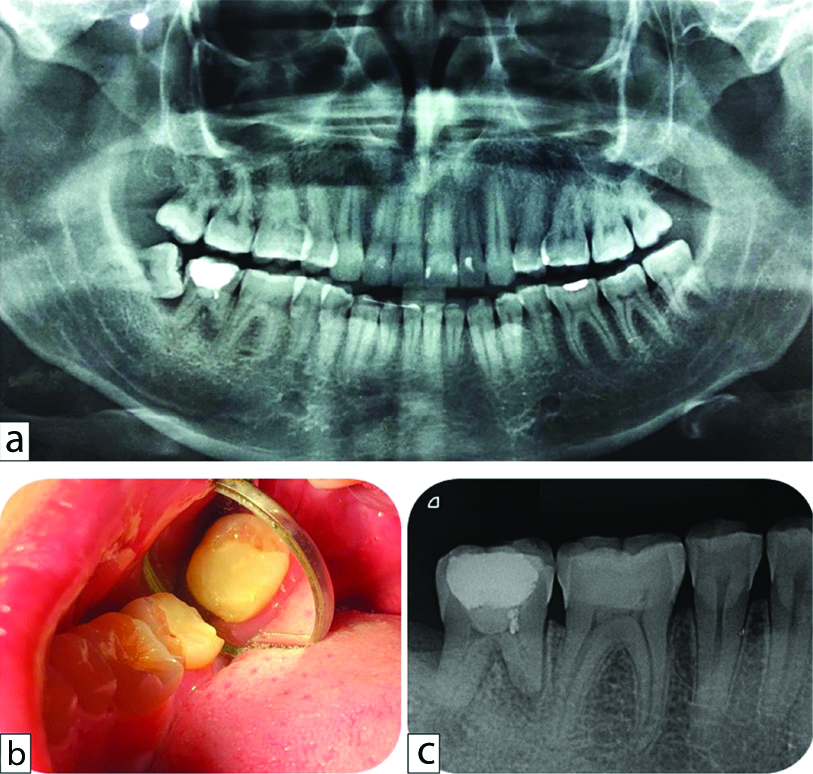
On intraoral analysis, tooth 47 presented healthy gingival tissues, and the periodontal probing depths were in the normal range with no mobility. Palpation and percussion tests induced no discomfort or pain. There was no evidence of a swelling or sinus tract. Cold test using Endo Ice (Maquira Indústria de Produtos Odontológicos SA, Maringá, PR, Brazil) elicited no response on tooth 47. Moreover, the tooth 47 presented an extensive direct composite resin restoration with no visible leakage or caries and no noticeable discolouration [Table/Fig-1b]. The history of a previous trauma was negative.
A panoramic radiograph showed that tooth 48 was unerupted and impacted by the adjacent second molar. No involvement of the distal root of the tooth 47 was observed. Tooth 47 presented a pulp chamber filled with a radiopaque material and periapical radiolucencies associated with ERR of the mesial and distal roots [Table/Fig-1a].
A diagnosis of horizontal impaction was established for tooth 48, while a diagnosis of asymptomatic chronic apical periodontitis and ERR were established for tooth 47. Removal of the tooth 48, followed by root canal treatment of the tooth 47 was decided.
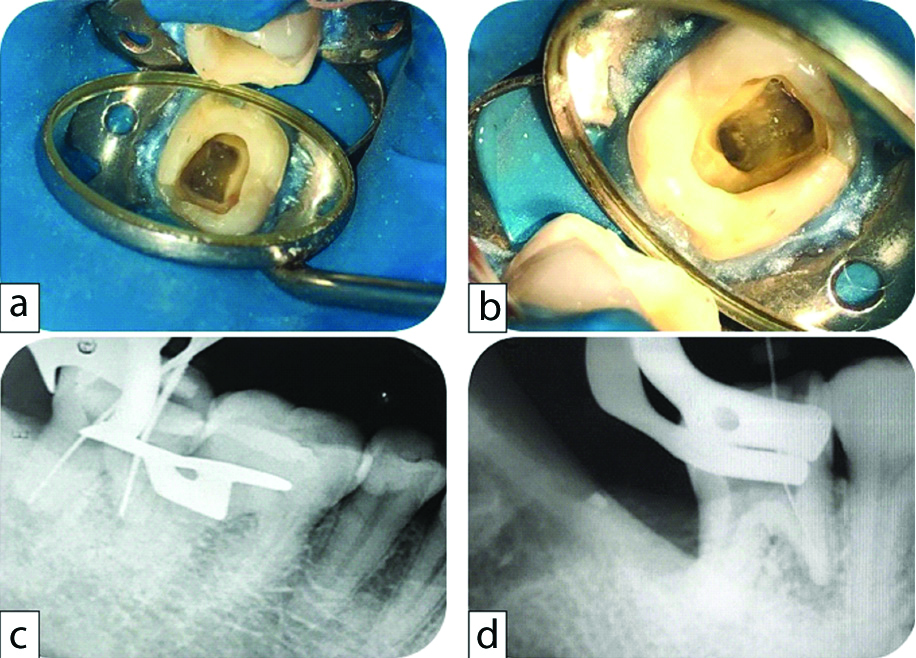
At the first appointment, ten days after the removal of tooth 48, a complementary radiographic examination was performed. The periapical radiograph of tooth 47 revealed signs suggestive of pulpotomy. Moreover, calcified root canals, severe ERR of the mesial root, and periapical radiolucencies in the mesial and distal roots were also highlighted [Table/Fig-1c]. The area of tooth 47 was anaesthetised with 2% lidocaine with 1:100.000 epinephrine (DFL Indústria e Comércio, Rio de Janeiro, RJ, Brazil) and the tooth was isolated with a rubber dam. The restorative material was removed with a spherical diamond #1013 bur (KG Sorensen, Barueri, SP, Brazil). Clinical exploration of the pulp chamber floor with an endodontic explorer revealed the presence of internal hard tissue. No root canal orifice was found [Table/Fig-2a]. The internal hard tissue was removed with an ultrasonic tip (E6D; Helse Dental Technology, Santa Rosa do Viterbo, SP, Brazil) at power setting 3 of an ultrasonic unit (EMS PM 200; EMS – Electro Medical Systems S.A., Nyon, Switzerland). Three root canal orifices were identified, Mesiobuccal (MB), Mesiolingual (ML) and Distal (D) [Table/Fig-2b]. Preflaring for all root canals was performed with an SX instrument (Dentsply Maillefer). The Working Length (WL) was established using an electronic apex locator (Propex II; Dentsply Maillefer) followed by radiographic confirmation [Table/Fig-2c,d]. The WL was found to be 18 mm in D canal, 15 mm in MB canal and 13 mm in ML canal. Cleaning and shaping was performed using nickel-titanium (WaveOne Gold; Dentsply Maillefer) and stainless-steel hand (K-Files; Dentsply Maillefer) files. The MB and ML canals were instrumented up to a size #35.06 and the D canal up to a size #60.02. The canals were irrigated with 2.5% sodium hypochlorite (NaOCl, Vic Pharma by Schülke, Taquaritinga, SP, Brazil), followed by a final flush with 17% EDTA (Biodinâmica, Ibiporã, PR, Brazil) and neutralisation with 2.5% NaOCl. All irrigant solutions were agitated with the EasyClean instrument (#25.04) (Easy Dental Equipment, Belo Horizonte, MG, Brazil). Three irrigant agitation steps of 20 seconds each were performed. A slight exudate from the apical region of the ML root canal was observed. The canals were dried, as much as possible, using paper points (Tanari, Manaus, AM, Brazil) and dressed with a non-setting Ca(OH)2 paste (UltraCal® XS, Ultradent Productions, Inc., South Jordan, UT, USA). The injectable application was via a 29-gauge disposable tip (NaviTip, Ultradent Productions, Inc., South Jordan, UT, USA) placed 2 mm short of the apex and slowly withdrawn. The radiographic image was taken to observe the quality of the placed Ca(OH)2 [Table/Fig-3a]. The access cavity was sealed with glass ionomer cement (Maxxion R, FGM Produtos Odontológicos, Joinville, SC, Brazil). The patient received information about the need to return for the scheduled appointments. Instructions to take analgesic medication if needed for any postoperative discomfort were also given. The non-setting Ca(OH)2 paste was renewed every three weeks for five months until no more exudate was observed and a decrease in the size of the periapical lesion and arrest of ERR was detected.
(a) Clinical view of the pulp chamber floor showing an internal hard tissue; (b) Clinical view of the pulp chamber floor after the use of ultrasonic tip and burs; (c,d) Radiographs showing root canal lengths determination.
(a) Radiograph confirming the adequate placement of calcium hydroxide dressing; (b) Radiograph taken immediately after root canal obturation; (c) 6-month follow-up radiograph, with evidence of periapical repair and containment of the inflammatory root resorptive process.
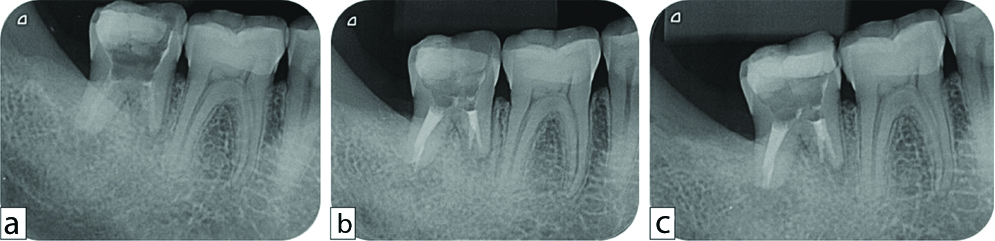
At the final visit, 5 months after beginning treatment, the root canal filling was performed. After rubber dam placement, access was obtained, and the canals were irrigated and re-prepared using the same protocol used during the first appointment. Then, the root canals were dried with sterilised absorbent paper points (Tanari, Manaus, AM, Brazil) and filled by lateral compaction of gutta-percha (Tanari) and Sealapex sealer (Sybron Endo, Orange, CA, EUA). The access cavity was again restored with glass ionomer cement (Maxxion R) [Table/Fig-3b] and the patient was referred for permanent restorative procedures.
Six months after treatment, the patient returned and was asymptomatic. The tooth had been restored with composite resin. Radiographic examination showed evidence of periapical repair and containment of the ERR process [Table/Fig-3c].
Discussion
ERR is a pathological condition, which can lead to tooth loss if not diagnosed and treated correctly [1]. It may arise as a complication of traumatic dental injury, orthodontic treatment or chronic infection of the pulp or periodontal tissues [1,2]. In this case report, root canal infection after the necrosis of pulp tissue stimulated an inflammatory response in the periapical tissues. It led to a severe resorptive process of the root.
Pulpotomy in mature permanent teeth is still a matter of debate [3-5]. Although many authors have stated that it’s very successful technique [3,5,6], postoperative complications have been observed [4]. The failure of pulpotomy is related to an inflammatory process or a bacterial infection [4], and it is characterised by the presence of tenderness to apical palpation and percussion, presence of a sinus tract, peripheral periodontal probing, swelling inspection and palpation and radiographic signs of periapical radiolucencies and ERR [6]. In this case, tooth 47 presented radiographic findings suggestive of pulpotomy (filled pulp chamber), chronic irreversible pulpitis of the radicular part of the pulp (calcified root canals and periapical radiolucency), and pulp infection (ERR) [4].
The management of ERR is dependent on its aetiology [2]. When ERR is associated with intracanal infection and inflammation of the periapical tissues, proper root canal sanitisation is essential [1,2]. The presence of eroded and resorbed areas in the interior of the root canal [7,8] offers technical difficulties to the complete disinfection of the root canal system [8,9]. The EasyClean system consists of a #25.04 plastic instrument in the shape of an “aircraft wing” [10]. This instrument optimises cleaning and disinfection by the mechanical agitation of the irrigant solution and by the mechanical drag of adhered debris [9]. Cesario F et al., compared the capacity of different irrigation protocols for debris removal from artificial grooves and observed good results with the use of Easy Clean [8].
Ca(OH)2 has been commonly used as an intracanal medicament in cases of teeth with pulp necrosis, peri-radicular lesions, and severe ERR [1,2]. Its biological and bacteriological properties are associated with the dissociation of calcium and hydroxyl ions [10], which can be influenced by both the vehicle used and additives. A wide range of manufactured Ca(OH)2 products is available for use in Endodontics, including non-setting formulations [7,11-13]. UltraCal XS is a syringe-delivery system consisting of 35% Ca(OH)2, 19% barium sulphate, 3% propylene glycol, and 2% methylcellulose [12]. The ability of this system to arrest and repair inflammatory ERR has been attributed to its alkalinising effect since the action of inflammatory and clastic cells is enhanced by an acidic pH [11]. The aqueous methylcellulose base of UltraCal XS appears to enhance the diffusion of Ca(OH)2 ions through dentin [11]. This diffusion is also facilitated by the geometry of the smaller particles present in the paste [12]. Komabayashi T et al., stated that the Ca(OH)2 particles inside the dentin tubules might act as a direct and continuing source of dissociated Ca(OH)2, which may result in a high and prolonged local pH [12]. Unfortunately, the use of non-setting Ca(OH)2 paste is not free from unpleasant complications [13]. Shahravan A et al., described a case involving an iatrogenic overextension of non-setting Ca(OH)2 during root canal treatment and presented a literature review of similar reports. For the authors caution should be taken when using syringe-delivery Ca(OH)2 systems [13]. In the present case, no extrusion of Ca(OH)2 was observed. Ca(OH)2 was injected using a 29-gauge disposable tip (NaviTip) following to the manufacturer’s instruction. It is important to select the correct size of the application tip, since the binding of the Ca(OH)2 syringe to the root canal may lead to the extrusion of the paste [11,13].
Although the information obtained through the Cone Beam Computed Tomography (CBCT) can assist in planning, diagnosis, treatment and prognosis in Endodontics [1], but in the present case report, it was not used since panoramic and periapical radiographs allowed the diagnosis and monitoring of the ERR. CBCT images have been suggested only when diagnostic tests and conventional radiographs or other imaging methods fail to disclose important diagnostic and clinical information [14].
One concern discussed in several studies relates to the effect of short and long-term use of Ca(OH)2 on the fracture strength of dentine [15,16]. It has been advocated that the alkalinity of Ca(OH)2 may weaken the root [16]. Yassen GH and Platt JA performed a systematic review to identify and analyse studies related to the effect of non-setting Ca(OH)2 on root fracture and mechanical properties of radicular dentine. The authors reported that, although most laboratory studies showed reduction in the mechanical properties of radicular dentine after use of Ca(OH)2, no clinical studies that support this correlation were found in the literature [15]. Further longitudinal high-level studies should be developed to clarify this subject.
The control of the intracanal discharge, decrease in the size of the periapical lesion, and arrest of ERR observed in this case were obtained after five appointments. Similar results were observed in previous published reports [Table/Fig-4] [17-22].
Review of previous published case reports.
| Author | Tooth/Teeth | Condition associated to external root resorption | Intracanal medicament | Outcome |
|---|
| Saad AY [17] | 11 | Pulp necrosis | Calcium Hydroxide mixed with distilled water | Formation of calcific tissue filling in the resorptive defect after 1 year |
| Bhat SS et al., [18] | 21 | Avulsion | Non-setting Calcium Hydroxide paste (Vitapex paste) | Healing of the inflammatory resorption after 12 months |
| Lamping R et al., [19] | 11 | Chronical apical periodontitis | Calcium Hydroxide mixed with polyethyleneglycol | Root resorption stagnation process after 6 months |
| Herrera H et al., [20] | 48 | Auto-transplantation | Non-setting Calcium Hydroxide paste (Calen paste) | Healing of the areas of resorption after 6 months |
| Cunha RS et al., [21] | 21 | Avulsion | Calcium Hydroxide mixed with propylene glycol | Resorption process arrested after 60 days |
| Fernandes M et al., [22] | 34 and 35 | Orthodontic treatment | Calcium Hydroxide mixed with distilled water | Normal root architecture of the root apices after 5 months |
| Current study | 47 | Chronic Apical periodontitis | Non-setting Calcium Hydroxide paste (UltraCal® XS) | Arrested ERR after 6 months |
Conclusion(s)
Chemomechanical root preparation in association with an injectable non-setting Ca(OH)2 dressing protocol allows positive outcomes during the management of severe ERR.
[1]. Estrela C, Guedes OA, Rabelo LE, Decurcio DA, Alencar AH, Estrela CR, Detection of apical inflammatory root resorption associated with periapical lesion using different methodsBraz Dent J 2014 25(5):404-08.10.1590/0103-644020130243225517775 [Google Scholar] [CrossRef] [PubMed]
[2]. Fuss Z, Tsesis I, Lin S, Root resorption- diagnosis, classification and treatment choices based on stimulation factorsDent Traumatol 2003 19(4):175-82.10.1034/j.1600-9657.2003.00192.x12848710 [Google Scholar] [CrossRef] [PubMed]
[3]. Kunert GG, Kunert IR, da Costa Filho LC, de Figueiredo JAP, Permanent teeth pulpotomy survival analysis: a retrospective follow-upJ Dent 2015 43(9):1125-31.10.1016/j.jdent.2015.06.01026144188 [Google Scholar] [CrossRef] [PubMed]
[4]. Zanini M, Hennequin M, Cousson PY, A review of criteria for the evaluation of pulpotomy outcomes in mature permanent teethJ Endod 2016 42(8):1167-74.10.1016/j.joen.2016.05.00827339631 [Google Scholar] [CrossRef] [PubMed]
[5]. Linsuwanont P, Wimonsutthikul K, Pothimoke U, Santiwong B, Treatment outcomes of mineral trioxide aggregate pulpotomy in vital permanent teeth with carious pulp exposure: the retrospective studyJ Endod 2017 43(2):225-30.10.1016/j.joen.2016.10.02728041685 [Google Scholar] [CrossRef] [PubMed]
[6]. Asgary S, Fazlyab M, Sabbagh S, Eghbal MJ, Outcomes of different vital pulp therapy techniques on symptomatic permanent teeth: A case seriesIran Endod J 2014 9(4):295-300. [Google Scholar]
[7]. Sirén EK, Kerosuo E, Lavonius E, Meurman JH, Haapasalo M, Ca(OH)2 application modes: In vitro alkalinity and clinical effect on bacteriaInt Endod J 2014 47(7):628-38.10.1111/iej.1219924330189 [Google Scholar] [CrossRef] [PubMed]
[8]. Cesario F, Hungaro Duarte MA, Duque JA, Alcalde MP, de Andrade FB, Reis So MV, Comparisons by microcomputed tomography of the efficiency of different irrigation techniques for removing dentinal debris from artificial groovesJ Conserv Dent 2018 21(4):383-87.10.4103/JCD.JCD_286_1630122818 [Google Scholar] [CrossRef] [PubMed]
[9]. Kato AS, Cunha RS, da Silveira Bueno CE, Pelegrine RA, Fontana CE, de Martins AS, Investigation of the efficacy of passive ultrasonic irrigation versus irrigation with reciprocating activation: An environmental scanning electron microscopic studyJ Endod 2016 42(4):659-63.10.1016/j.joen.2016.01.01626906240 [Google Scholar] [CrossRef] [PubMed]
[10]. de Oliveira RL, Guerisoli DMZ, Duque JA, Alcalde MP, Onoda HK, Domingues FHF, Computed microtomography evaluation of calcium hydroxide-based root canal dressing removal from oval root canals by different methods of irrigationMicrosc Res Tech 2019 82(3):232-37.10.1002/jemt.2316430614119 [Google Scholar] [CrossRef] [PubMed]
[11]. Zmener O, Pameijer CH, Banegas G, An in vitro study of the pH of three calcium hydroxide dressing materialsDent Traumatol 2007 23(1):21-25.10.1111/j.1600-9657.2005.00447.x17227376 [Google Scholar] [CrossRef] [PubMed]
[12]. Komabayashi T, Ahn C, Spears R, Zhu Q, Comparison of particle morphology between commercial- and research-grade calcium hydroxide in endodonticsJ Oral Sci 2014 56(3):195-99.10.2334/josnusd.56.19525231145 [Google Scholar] [CrossRef] [PubMed]
[13]. Shahravan A, Jalali S, Mozaffari B, Pourdamghan N, Overextension of nonsetting calcium hydroxide in endodontic treatment: Literature review and case reportIran Endod J 2012 7(2):102-08. [Google Scholar]
[14]. Durack C, Patel S, Cone beam computed tomography in endodonticsBraz Dent J 2012 23(3):179-91.10.1590/S0103-6440201200030000122814684 [Google Scholar] [CrossRef] [PubMed]
[15]. Yassen GH, Platt JA, The effect of nonsetting calcium hydroxide on root fracture and mechanical properties of radicular dentine: A systematic reviewInt Endod J 2013 46(2):112-18.10.1111/j.1365-2591.2012.02121.x22970899 [Google Scholar] [CrossRef] [PubMed]
[16]. Kahler SL, Shetty S, Andreasen FM, Kahler B, The effect of long-term dressing with calcium hydroxide on the fracture susceptibility of teethJ Endod 2018 44(3):464-69.10.1016/j.joen.2017.09.01829254817 [Google Scholar] [CrossRef] [PubMed]
[17]. Saad AY, Calcium hydroxide in the treatment of external root resorptionJ Am Dent Assoc 1989 118(5):579-81.10.14219/jada.archive.1989.00712715544 [Google Scholar] [CrossRef] [PubMed]
[18]. Bhat SS, Sharan SS, Madan I, Healing of root resorption: A case reportJ Clin Pediatr Dent 2003 27(3):235-38.10.17796/jcpd.27.3.5n213546817741x712739683 [Google Scholar] [CrossRef] [PubMed]
[19]. Lamping R, Maekawa LE, Marcacci S, Nassri MRG, External inflammatory root resorption: Clinical case description using calcium hidroxide pasteRSBO 2005 2(1):44-48. [Google Scholar]
[20]. Herrera H, Herrera H, Leonardo MR, de Paula e Silva FW, da Silva LA, Treatment of external inflammatory root resorption after autogenous tooth transplantation: Case reportOral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 102(6):e51-54.10.1016/j.tripleo.2006.05.02717138168 [Google Scholar] [CrossRef] [PubMed]
[21]. Cunha RS, Abe FC, Araujo RA, Fregnani ER, Bueno CE, Treatment of inflammatory external root resorption resulting from dental avulsion and pulp necrosis: Clinical case reportGen Dent 2011 59(3):e101-04. [Google Scholar]
[22]. Fernandes M, de Ataide I, Wagle R, Tooth resorption part II- external resorption: Case seriesJ Conserv Dent 2013 16(2):180-85.10.4103/0972-0707.10821623716975 [Google Scholar] [CrossRef] [PubMed]