Anal canal is a terminal part of alimentary canal with primary function to maintain continence by its complex sphincters comprising of internal and external sphincters [1]. The internal anal sphincter maintains the anal tone [2] by being in a continuous state of partial contraction and relaxation in response to rectal distension while, the external sphincter is a voluntary muscle. The sphincters like any other muscles in human body are prone to stress and spasm, mostly caused during heavy bowel movement, excessive pressure on sphincter in chronic constipation, passing dry bowel or surgery. These are a few conditions that might lead to a painful condition caused by a tear or split in the outermost skin of anal canal, called anal fissure [3]. Usually, people diagnosed with fissure present with pain and small amounts of bright red rectal bleeding.
Fissures are differentiated on the basis of the time taken to heal, size or shape, location and volume of tear and splits. The fissures located in the posterior or anterior position and having benign effect are defined as ‘Primary fissures’ while, lateral or multiple tears often indicate a more serious underlying pathology and are classified as ‘Secondary fissures’ [4].
Management of anal fissures are also as diverse as the disorder, and range from non-operative techniques of dietary changes, topical ointments, Botulinum toxin injections to sitz baths, however surgery can be the ultimate resolution in case of therapies and medicines proving to be ineffective and inefficient.
Acute fissure is defined as a tear in the fragile skin at the anal outlet lasting for less than four weeks [5] and treated by dietary changes, laxatives and topical ointment aimed at reducing anal pressure [6] whereas, the chronic anal fissure “non-healing fissure” [7] is defined as a tear of epithelium below dentate line and lasting for more than four weeks and it requires medicine and sometimes surgical interventions for management [8].
More recently, topical nitroglycerins and hydrochlorides of diltiazem have gained popularity in clinical practice and have been found highly efficient in reducing pain and quick healing [9]. Management of chronic anal fissure is still difficult with available treatment options, therefore needs further study on other types of medical management options.
The present study was aimed to evaluate and compare the efficiency of topical glycerine nitrate (0.2%) with topical diltiazem (2%) in patients with anal fissures.
Materials and Methods
The present prospective interventional study was carried out from February 2018 to December 2019. Informed patient consent and approval from Institutional Ethics Committee, Era University, Lucknow were taken before initiating the study (vide letter no. ELMC/R_Cell/EC/2018/68 dated 09/02/2018). The study population comprised of a suburban and rural population of Lucknow, India.
Inclusion criteria: Patients aged >18 years presenting to the Surgery OPD and Emergency with anal fissure.
Exclusion criteria:
Patients with anal fissure due to other diseases like inflammatory bowel disease, tuberculosis, malignancy, sexually transmitted diseases.
Patients who had associated haemorrhoids, fistula, pregnant/lactating females and patients with significant cardiovascular condition
Patients advised/seeking surgical intervention.
Sample size calculation: Sample size was calculated by using the formula:
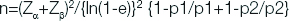
Where p1=0.7187 (71.87%)
p2=0.6823 (68.23%), the proportions of complete tissue healing
e=0.3
Type I error α=5%
Type II error β=10% for detecting results with 90% power of study
The sample size came out to be n=100, divided in two Groups I and II 50 each.
Methodology: The demographic information, duration and nature of complaints were noted. All the patients were clinically examined and basic laboratory and necessary radiographic investigations (x-ray chest, abdominal Ultrasound) were done before treatment. Patients were divided by using Sequentially Numbered, Opaque Sealed Envelopes (SNOSE) system into two groups for administration of one of the study drugs [10].
Patients were either given topical 2% diltiazem or topical 0.2% glyceryl trinitrate and followed for a period of six weeks (weekly follow-up) to evaluate the healing effect of above two topical ointments. Patients were followed at three months to look for recurrence.
Scale of pain: Pain was assessed on a 0 to 10 point scale, where 0 is indicative of “no pain” and 10 as worst pain. Score 1-3 mild pain (interferes little with activities of daily living), score 4-6 moderate pain (interferes more with activities of daily living) whereas score 7-10 severe pain (unable to perform activities of daily living).
Statistical Analysis
The statistical analysis was done using SPSS (Statistical Package for Social Sciences) Version 15.0 statistical Analysis Software. The values were represented in Number (%) and Mean±SD. The following statistical tests were used:
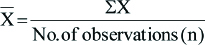
Mean: The individual observation is denoted by the sign X, number of observation denoted by n, and the mean by X̄.
Standard deviation: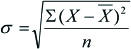
Chi-square test: Where O=Observed frequency, E=Expected frequency
Where O=Observed frequency, E=Expected frequency
Student t-test: To test the significance of two means the student t-test was used
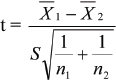
where, X̄1, X̄2 are means of Group 1 and Group 2
n1, n2 are number of observation Group 1 and Group 2
SDI, SD2 are standard deviation in Group 1 and Group 2
Level of significance: “p” is level of significance
p<0.05 Significant
Results
Out of 100 patients of anal fissure, 50 (50.0%) were selected for treatment with topical application of 2% Diltiazem (Group I) while rest 50 were selected for topical application of 0.2% Glyceryl trinitrate (Group II).
Difference in age of patients of above two groups was not found significant [Table/Fig-1]. Difference in duration of symptoms between two groups was not found statistically significant [Table/Fig-2].
Comparison of Demographic profile between two groups.
| SN | Characteristics | Group I (n=50) | Group II (n=50) | Statistical significance |
|---|
| 1. | Mean Age+SD (Years) | 40.06±15.44 (18-87) | 39.56±15.49 (18-80) | p=0.872 |
| | No. (%) | No. (%) | ‘p’ |
| 2. | Sex |
| Male | 24 (48.0) | 24 (48.0) | 1.000 |
| Female | 26 (52.0) | 26 (52.0) |
Demographic profile and Baseline characteristics between two groups.
| SN | Characteristics | Group I (n=50) | Group II (n=50) | Statistical significance |
|---|
| No. (%) | No. (%) | ‘p’ |
|---|
| 1. | Blood in stool | 37 (74.0) | 38 (76.0) | 0.817 |
| 2. | Skin tag around anus | 7 (14.0) | 8 (16.0) | 0.779 |
| 3. | Duration of symptoms |
| ≤7 days | 17 (34.0) | 17 (34.0) | 0.923 |
| 7 days-1 month | 30 (60.0) | 29 (58.0) |
| >1 month | 3 (6.0) | 4 (8.0) |
At follow-up of one week, majority of the patients had moderate level of pain during defecation (n=54.0%) and itching/bleeding were present in (75.0%). Swelling was observed in 46.0% and muscles were visible in minority of cases (3.0%) but these differences were not found statistically significant between the two groups [Table/Fig-3].
Follow-up assessment at 1 week.
| SN | Characteristics | Group I (n=50) | Group II (n=50) | Statistical significance |
|---|
| No. (%) | No.(%) | ‘p’ |
|---|
| 1. | Pain during defecation |
| Mild pain | 1 (2.0) | 2 (4.0) | 0.837 |
| Moderate pain | 27 (54.0) | 27 (54.0) |
| Severe pain | 22 (44.0) | 21 (42.0) |
| 2. | Itching/Bleeding | 38 (76.0) | 37 (74.0) | 0.817 |
| 3. | Swelling | 23 (46.0) | 23 (46.0) | 1.000 |
| 4. | Visibility of muscles | 2 (4.0) | 1 (2.0) | 0.558 |
At follow-up visit on Week 2 and 3, on comparing the pain during defecation, itching/bleeding and swelling were not statistically significant between the two groups. Proportion of patients of Group I was higher as compared to Group II with lower order of pain i.e., no pain (2.0% vs. 0.0%) and mild pain (38.0% vs. 18.0%) while proportion of patients of Group II was higher as compared to Group I having higher order of pain i.e., moderate (80.0% vs. 60.0%) and severe pain (2.0% vs. 0.0%). Though complaints of itching/bleeding were reported higher in Group II as compared to Group I (44.0% vs. 26.0%). Swelling was observed in higher proportion of cases of Group II as compared to Group I (40.0% vs. 20.0%).
On follow-up visit at Week 4, significant difference between Group I and Group II were observed for Pain during defecation, incidence of Itching/bleeding and swelling. Visibility of muscles was found to be similar in both the groups [Table/Fig-4].
Follow-up assessment at week 4.
| SN | Characteristics | Group I (n=50) | Group II (n=50) | Statistical significance |
|---|
| No. (%) | No. (%) | ‘p’ |
|---|
| 1. | Pain during defecation |
| No pain | 11 (22.0) | 3 (6.0) | 0.023 |
| Mild | 30 (60.0) | 29 (58.0) |
| Moderate | 9 (18.0) | 18 (36.0) |
| 2. | Itching/Bleeding | 4 (8.0) | 16 (32.0) | 0.003 |
| 3. | Swelling | 2 (4.0) | 9 (18.0) | 0.025 |
| 4. | Visibility of muscles | 1 (2.0) | 1 (2.0) | 1.000 |
On follow-up at Week 6, No pain during defecation was observed in higher proportion of cases of Group I as compared to Group II (88.0% vs. 68.0%) while proportion of patients of Group II were higher as compared to Group I having mild pain (26.0% vs. 12.0%) and moderate pain (6.0% vs. 0.0%) during defecation. This difference was found statistically significant. Complaints of itching/bleeding were reported by significantly higher proportion of patients of Group II as compared to Group I [Table/Fig-5].
Follow-up assessment at week 6.
| SN | Characteristics | Group I (n=50) | Group II (n=50) | Statistical significance |
|---|
| No. (%) | No. (%) | ‘p’ |
|---|
| 1. | Pain during defecation |
| No pain | 44 (88.0) | 34 (68.0) | 0.032 |
| Mild pain | 6 (12.0) | 13 (26.0) |
| Moderate pain | 0 (0.0) | 3 (6.0) |
| 2. | Itching/Bleeding | 0 (0.0) | 4 (8.0) | 0.041 |
| 3. | Swelling | 0 (0.0) | 1 (2.0) | 0.315 |
| 4. | Visibility of muscles | 0 (0.0) | 0 (0.0) | - |
Full cure was observed in significantly higher proportion of cases of Group I as compared to Group II (88.0% vs. 68.0%), rest of the patients of both the groups had Partial cure [Table/Fig-6].
Comparison of Outcome between two groups.
| SN | Outcome | Group I (n=50) | Group II (n=50) | Statistical significance |
|---|
| No. (%) | No. (%) | ‘p’ |
|---|
| 1. | Full cure | 44 (88.0) | 34 (68.0) | 0.016 |
| 2. | Partial cure | 6 (12.0) | 16 (32.0) |
Majority of the patients of both the groups did not observe any side effect (Group I-94.0% and Group II-84.0%). Difference in side effects of patients of above two groups was found statistically significant [Table/Fig-7].
Comparison of Side effects between two groups.
| SN | Side effects | Group I (n=50) | Group II (n=50) | Statistical significance |
|---|
| No. (%) | No. (%) | ‘p’ |
|---|
| 1. | None | 47 (94.0) | 42 (84.0) | 0.004 |
| 2. | Headache | 0 (0.0) | 8 (16.0) |
| 3. | Itching | 3 (6.0) | 0 (0.0) |
None of the patients of anal fissure treated irrespective of treatment mode had reported recurrence the follow-up of three months.
Discussion
Studies have found various non-operative therapies which are effective in management and treatment of anal fissures. Some of these techniques include topical gels/cream/ointments etc. Of the various medicines and topical gels used for management of the disorder, some of the prime methods that have been identified are: topical gels derived from Glyceryl Trinitrate, Diltiazem Hydrochloride, combination of Nifedipine (NIF), Lidocaine Hydrochloride (LDH) and Betamethasone Valerate (BMV), oral and topical calcium blockers, Botulinum toxin injection.
In the present study, the Diltiazem group was found to have significantly improved as compared to the Glyceryl Trinitrate group, with 78 (78%) of patients being cured overall; 88% patients in Diltiazem arm were cured as compared to 68% patients in the Glyceryl trinitrate arm. In contrast to Bansal AR et al., study where complete healing was observed in 80% in Diltiazem group vs. 72% patients in Glyceryl trinitrate group at the end of six weeks [11]. It was concluded that both 0.2% glyceryl trinitrate and 2% Diltiazem ointment were equally effective in chronic anal fissure treatment. They evaluated pain relief, healing and recurrence, but found headache as a side effect in people treated with glyceryl trinitrate ointment. In another study conducted by Khan MS et al., it was found that complete healing of fissure was observed in 71.2% patients, among which 80.4% people belonged to Diltiazem group while 62% to Glyceryl Trinitrate group [12]. A significant association was found only between healing outcome and duration of symptoms.
Blood in stool was the most popular baseline characteristics of the disease. Similar frequency of symptom of the disease have been reported by studies conducted by Venkatesh S et al., who reported healing in 80% patients treated with Diltiazem and in 76% of patients in Glyceryl Trinitrate group by the sixth week end follow-up [13].
The decreasing pain scores and swelling along with other complications of the disorder align with other contemporary studies like: Khan MS et al., showed an overall outcome in terms of healing to be 71.2%, among which 80.4% were from Diltiazem group while 62% in Glyceryl Trinitrate group, they found Diltiazem to have better outcomes in terms of healing and reduction in symptoms [12].
On studying the side-effects of the two treatment options in the present study, it was found that most of the patients had no side effect of the therapy. The itching related side effects were more in the Diltiazem group whereas patients in the Glyceryl trinitrate regime had higher side effects all in form of headaches. Khalique A et al., reported similar differences in Glyceryl Trinitrate group having more occurrence of headache than diltiazem group (30% vs. 7.5%) [14]. Khalique A et al., have also reported in their study that 5% patients in their study had to abandon the treatment due to severe headaches [14]. Tomar V and Saxena A also found headaches to be more common in patients treated with Glyceryl trinitrate, they reported that almost half of the population using Glyceryl trinitrate developed severe headaches as compared to rare cases in the diltiazem arm [15]. Moreover, they found perianal itching and recurrence rate (followed upto six months) to be similar amongst the two arms.
Various topical, oral and surgical methods have been invented to heal anal fissures, but it is important to note that with the mixed demographic and economic status of the patients, it is difficult to track the best alternative treatment. However, topical ointments have become the popular choice because of their inexpensive nature and moreover, due to managing the social embarrassment associated with the disease. Of these, topical ointments Diltiazem; a calcium channel blocker and Glyceryl trinitrate; a nitroglycerin has emerged to be most commonly used. The difference in the working of drugs, bring with itself the side effects associated with them, where Diltiazem is known to cause itching and uneasiness because of contact allergic dermatitis [16] whereas Glyceryl trinitrate is known to cause headaches due to systemic absorption of the topical glyceryl trinitrate which can result in vasodilation and severe headaches [17]. Thus, making Diltiazem as the first line of treatment in patients with anal fissures and specifically making it the treatment of choice due to better healing capabilities, low risk of side effects, faster decrease in pain and no cost advantage.
Limitation(s)
The limitation of study was that the duration of the treatment was quite long with topical agents, hence causing less patient compliance because during follow-up, six patients complained of long duration treatment but they continued the follow-up on counselling.
Conclusion(s)
Findings of the present study indicated that topical diltiazem (2%) was more effective as compared to glyceryl trinitrate (0.2%) (88.0% vs. 68.0%) for conservative treatment of anal fissure. Diltiazem group reported side effects of Itching (6.0%) while glyceryl trinitrate group reported headache as side effect (16.0%).