Correlation of Erectile Dysfunction and Lower Urinary Tract Symptoms among Men at Urology Clinic of a Tertiary Care Institute in South-East Nigeria
Joseph Amauzo Abiahu1, Timothy Uzoma Mbaeri2, Jideofor Chukwuma Orakwe3, Alexander Maduaburochukwu Ekwunife Nwofor4
1 Lecturer, Department of Surgery, Nnamdi Azikiwe University, Nnewi Campus, Nnewi, Anambra, Nigeria.
2 Senior Lecturer, Department of Surgery, Nnamdi Azikiwe University, Nnewi Campus, Nnewi, Anambra, Nigeria.
3 Professor, Department of Surgery, Nnamdi Azikiwe University, Nnewi Campus, Nnewi, Anambra, Nigeria.
4 Professor, Department of Surgery, Nnamdi Azikiwe University, Nnewi Campus, Nnewi, Anambra, Nigeria.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Joseph Amauzo Abiahu, Department of Surgery, Nnamdi Azikiwe University, Nnewi, Anambra, Nigeria.
E-mail: jabiahu2000@yahoo.com
Introduction
Available literature suggests an association between Lower Urinary Tract Symptoms (LUTS) and sexual dysfunction especially Erectile Dysfunction (ED). LUTS, either alone or in combination with ED, represents a considerable problem for ageing men. An understanding of correlation between LUTS and ED in these ageing men will be useful in their routine care.
Aim
To determine the incidence of ED and its correlation with LUTS in adult male patients attending the Urology clinic in a Tertiary Care Hospital.
Materials and Methods
This was a cross-sectional study of 110 consecutive patients with LUTS recruited from the urological clinic. The data were collected, while ED and LUTS were assessed with the 5-Item Version of the International Index of Erectile Function (IIEF-5) and International Prostate Symptom Score (IPSS) questionnaire forms respectively. Findings were subjected to linear regression and Pearson’s chi-square tests, using Statistical Package for Social Sciences (SPSS) version 17.
Results
The mean age of patients was 65.8±7.95 years. The incidence of ED among LUTS patients was 63.6%. There was positive correlation between ED scores and voiding phase, filling-storage phase and total LUTS scores. The severity of ED and graded LUTS score revealed no significant association between the severity of ED and that of voiding phase and filling-storage phase LUTS. Conversely, severity of ED was significantly related to the severity of total LUTS score.
Conclusion
ED is common amongst adult patients with LUTS. Its severity worsens with worsening LUTS. The management of patients with LUTS should therefore involve evaluation and treatment for ED. This calls for increased awareness of these conditions to both the doctor and the patient.
Association, International index of erectile function, International prostate symptom score
Introduction
LUTS is a constellation of filling/storage phase symptoms and voiding phase symptoms often as a result of increased bladder outlet resistance to outflow of urine or less frequently due to neuromyopathic bladder. The causes are variable and common among older men, increasing in incidence with age [1-5]. In the early 2000, an association was suggested between LUTS and sexual dysfunction especially ED. Also, both the conditions are strongly associated with age [1,3-7].
ED is defined as the persistent inability to achieve and/or maintain an erection sufficient for satisfactory sexual intercourse [1,8-12]. This gained tremendous attention following the discovery of Nitric Oxide (NO) in the human body [10,13]. LUTS, either alone or in combination with ED, represents a considerable problem for the ageing men due to negative impact it has on their quality of life [1,2,4,5,7,10-12,14,15]. In the Multinational Survey of the Ageing Male-7 (MSAM-7), a survey of over 14,000 men aged 50 years to 80 years from the USA, UK, France, Germany, Netherlands, Italy and Spain, the number of sexual activities per month was decreased by about half in men with LUTS compared to those without LUTS [6]. ED affects over 152 million men worldwide [16]. It was estimated that ED affects 20-30 million men in the USA [8,9]. Studies in some African, Arabic or Islamic countries with different socio-cultural and religious characteristics found a prevalence of 54.9% in Egypt, 50.7% in Nigeria, 64.3% in Turkey, and 53.6% in Morocco [15].
With the current ageing trends in the global population, the prevalence of ED is likely to increase significantly during the next 20 years [17]; with predominance in developing countries that have expanding populations and increasing life expectancies [9,12,18]. This can have both physical and psycho-social effects, and economic impacts. In the last few years, several studies have explored the association between LUTS and ED while controlling the co-morbidities like Diabetes, Hypertension and Heart disease [1,4,6,11,15,19-21]. Other risk factors like sedentary lifestyle and obesity have also been associated with increased risk of ED [4,22,23]. These co-morbidities increase with age and can directly or indirectly worsen the erectile function in ageing men.
This hospital based study with LUTS patients as the study population will give insight into the incidence of ED in a Nigerian hospital population; and aim to demonstrate the correlation between ED and LUTS in this study population.
Materials and Methods
This was a one year cross-sectional study, carried out from 1st of May 2012 to 31st April 2013. A total of one hundred and ten new patients ≥40 years with LUTS were recruited by purposive criterion sampling method from Urological Outpatient Clinic of Nnamdi Azikiwe University Teaching Hospital.
The sample size was calculated based on the statistical formula nf=n/1+n/N [24] where nf is the desired sample size when population is less than 10,000, n is the desired sample size when population is more than 10,000 and N is the estimate of the population size which is averagely 281 derived from a retrospective review of the cohort over a year period. This value (281) justifies the choice of this statistical formula for calculation of the sample size nf.
Ethical approval with reference number NAUTH/CS/66/Vol.3/86 was obtained from the research and ethics committee of the institution. Written informed consents were obtained from patients that met the inclusion criteria.
Inclusion criteria: Subjects included in the study were all new patients ≥40 years attending the urology clinic of the institution with clinical features of LUTS, who gave their consent to take part in the study.
Exclusion criteria: Patients on treatment for ED or LUTS, those with clinical features of UTI, those with major psychiatric disorders, and those with penile anatomical disorders were excluded.
The socio-demographic data were collected while ED and LUTS were assessed with the 5-Item Version of the IIEF-5 questionnaire form [25] and IPSS questionnaire form [26], respectively.
Statistical Analysis
Findings were subjected to linear regression and Pearson’s chi-square tests, where applicable and analysis was done using Statistical Package for Social Sciences version 17 with p-value <0.05 as significant.
Results
A total of 110 patients were studied. The age ranged from 43 years to 80 years with a mean age of 65.8±7.95 years. The peak age group was in age range 71-75 years with 34 patients (30.9%), followed by 56-60 years with 24 patients (21.8%).
The mean total LUTS and ED scores were 15.18±7.52 and 16.90±6.45, respectively. Other graded LUTS scores are represented in [Table/Fig-1].
LUTS and ED scores for patients (n=110).
| LUTS and ED scores | Range | Mean±SD |
|---|
| LUTS score (Voiding phase) {0-15} | 0-19 | 7.6±5.11 |
| LUTS score (Filling and storage phase) {0-20} | 1-15 | 8.12±3.67 |
| Total LUTS score {0-35} | 2-33 | 15.81±7.52 |
| ED score {0-25} | 8-25 | 16.90±6.45 |
LUTS- Lower Urinary Tract Symptoms; ED- Erectile Dysfunction
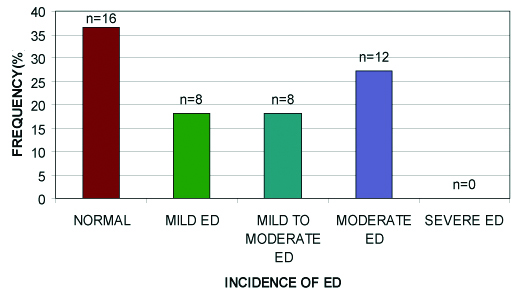
Among the 110 patients, only 44 (40%) had sexual intercourse within the preceding month. The reasons for non-attempt of sexual intercourse by the remaining 66 (60%) could not be ascertained. However, using ED scores to assess the LUTS patients that had sexual intercourse, majority [16 (36.4%)] had normal sexual function (ED score >21). Thus a total of 28 (63.6%) LUTS patients had some form of ED without any severe ED [Table/Fig-2].
Distribution of ED among LUTS patients that had sexual intercourse over the past one month.
ED- Erectile Dysfunction
Relationship between Severity of ED and LUTS
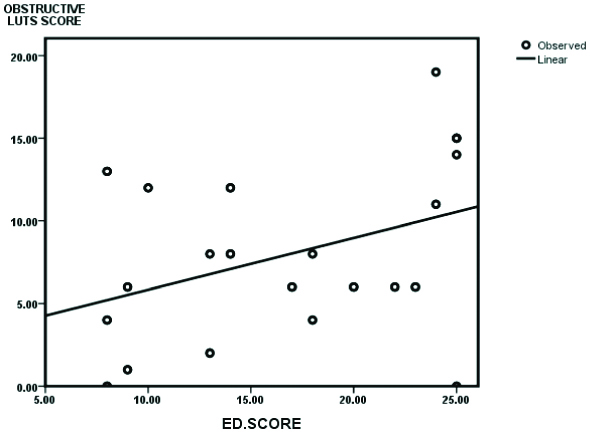
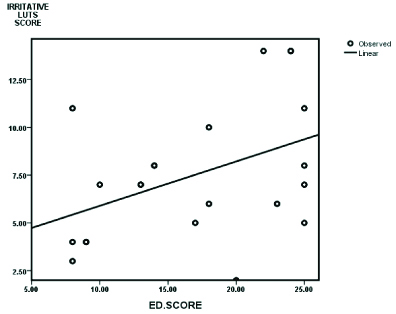
A linear regression between ED scores and LUTS scores indicated a significant relationship between ED scores and voiding phase, filling-storage phase, and total LUTS scores, respectively [Table/Fig-3,4,5 and 6].
Pearson’s bivariate correlation test between ED scores and LUTS scores.
| ED score vs. | Regression coefficient | p-value |
|---|
| Voiding phase LUTS score | 0.388 | 0.009 |
| Filling-storage phase LUTS score | 0.428 | 0.004 |
| Total LUTS score | 0.445 | 0.002 |
LUTS- Lower Urinary Tract Symptoms; p-value <0.05 significant
Scatter plot between voiding phase (Obstructive) LUTS and ED scores.
Scatter plot between filling-storage phase (Irritative) LUTS and ED scores.
Scatter plot between total LUTS and ED.
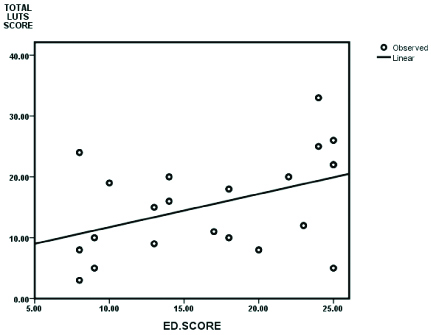
This positive correlation thus shows that the higher the LUTS scores (voiding phase, filling-storage phase and total), the higher the ED scores. However, Pearson’s chi-square analysis of severity of ED and graded LUTS score revealed no significant association between the severity of ED and that of voiding phase and filling-storage phase LUTS while severity of ED was significantly related (p=0.0001) to the severity of total LUTS score [Table/Fig-7].
Relationship between the severity of ED and graded LUTS scores.
| Severity of ED vs. | Pearson’s chi-square value | p-value |
|---|
| Graded voiding phase LUTS score | 6.33 | 0.096 |
| Graded filling-storage phase LUTS score | 7.11 | 0.068 |
| Graded Total LUTS score | 26.15 | 0.0001 |
LUTS- Lower Urinary Tract Symptoms; p-value <0.05 significant
Discussion
The peak age range of 71 years to 75 years and mean age of 65.8±7.95 years in this study supports the predominance of LUTS among the ageing population, as reported by other studies [2,4,5,8,23,27].
Ngai KH et al., studied ED and LUTS in a Hong Kong primary health care setting [8]. They reported median age of 65 years with age range of 25-85 years and overall prevalence of LUTS as 68% with higher prevalence among older men (>80% in men >50 years). Elliott SP et al., did a hospital based study to find the correlation between obstructive LUTS and ED [23]. They noted peak age range of 70-80 years with mean age of 68.2 years. Hoesl CE et al., reported mean age of 63.4±8.5 years [27]. They studied ED prevalence, bothersomeness and diagnosis in patients consulting urologists for Benign Prostatic Syndrome (BPS). The age ranges and mean ages in these studies are similar to the age range and mean age in this study.
In this study, there was a strong positive relationship (r=26.15, p=0.0001) between severity of ED and severity of total LUTS without adjustment for the age or co-morbidities. This is in agreement with several epidemiological studies [1,4,5,6,23]. Sara TB et al., studied the relationship between LUTS and ED in a Boston community and noted that LUTS worsened as prevalence and severity of ED also worsened [1]. However, the p-values were not stated. They further evaluated the association of specific LUTS with ED and noted that nocturia was the only symptom individually associated with ED. Thus, this theoretically translates to only filling-storage phase LUTS being associated with ED. This is not in keeping with our finding and that of Elliott SP et al., [23]. However, the possibility of false association exists, considering that other components of filling-storage phase LUTS had no association with ED in the study. Cayan S et al., reported a significant correlation of LUTS and the presence and severity of ED (p<0.001) [4]. Also, Dumbraveanu I et al., in their study among men from the republic of Moldova, reported direct correlation between ED and LUTS regardless of age or other comorbidities [5]. A multinational survey of the ageing male, [6] on LUTS and male sexual dysfunction, noted that the ED scores decreased with worsening LUTS across the studied age groups. When controlled for age, it was noted that LUTS severity was the strongest predictor of ED. Conversely, Elliott SP et al., worked on correlation between voiding phase LUTS and ED. They reported a correlation between ED and voiding LUTS (r=-0.20, p=0.006), but not the total LUTS (r=0.17, p=0.023) [23]. In the present study, no correlation was noted with graded voiding phase LUTS (p-value 0.096, Pearson’s chi-square 6.33). This difference might be due to the study method. Elliott SP et al., were more objective in further assessment of voiding phase LUTS by uroflowmetric study and ultrasound determinant of postvoid residual urine volume [23]. This may have added higher positive values and tendency of significance compared with this study where the study was depended only on subjectivity with tendency to underreport.
Limitation(s)
The IPSS and IIEF were designed to be self administered. Also, many of the subjects were not well educated, thus the researcher assisted in filling of the questionnaire. This could introduce bias in the study. The study population was also selective. Thus, the findings may not be directly applicable to the general population.
Conclusion(s)
ED is prevalent amongst adult patients with LUTS. Its severity worsens with worsening LUTS. Since LUTS is age-related, a rise in overall incidence of ED is expected with the current drift in population dynamics towards the older population. Thus, the present study recommend that the management of patients with LUTS should involve a thorough evaluation and treatment for ED. It is therefore important to increase the awareness of these conditions to the doctor and the patient. However, further research to elucidate the causal basis for this relationship between ED and LUTS is also needed.
LUTS- Lower Urinary Tract Symptoms; ED- Erectile Dysfunction
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 06, 2020
Manual Googling: Mar 31, 2020
iThenticate Software: Jun 26, 2020 (16%)
[1]. Sara TB, Carol LL, Jenny LD, John BM, John BM, Relationship between lower urinary tract symptoms and erectile dysfunctionJ Urol 2008 179:250-55.10.1016/j.juro.2007.08.16718001787 [Google Scholar] [CrossRef] [PubMed]
[2]. Kupelian V, Wei JT, O’Leary MP, Kusek JW, Litman HJ, Link CL, Prevalence of lower urinary tract symptoms and effect on quality of life in a racially and ethnically diverse random sample: Boston Area Community Health (BACH) SurveyArch Intern Med 2006 166:2381-87.10.1001/archinte.166.21.238117130393 [Google Scholar] [CrossRef] [PubMed]
[3]. Kevin M, Lower urinary tract symptoms and sexual dysfunction: Epidemiology and patholophysiologyBr J Urol Int 2006 97(2):23-28.10.1111/j.1464-410X.2006.06102.x16507050 [Google Scholar] [CrossRef] [PubMed]
[4]. Cayan S, Kendirci M, Yaman O, Asci R, Orhan I, Usta M, Prevalence of erectile dysfunction in men over 40 years of age in Turkey: Result from the Turkish Society of Andrology Male Sexual Health Study GroupTurk J Urol 2017 43(2):122-29.10.5152/tud.2017.2488628717533 [Google Scholar] [CrossRef] [PubMed]
[5]. Dumbraveanu I, Ceban E, Banov P, Lower urinary tract symptoms and erectile dysfunction in men from the Republic of MoldovaJournal of Medicine and life 2018 11(2):153-59. [Google Scholar]
[6]. Rosen R, Altwein J, Boyle P, Kirby R, Lukacs B, Meuleman E, Lower urinary tract symptoms and male sexual dysfunction. The Multinational Survey of the Aging Male (MSAM-7)Eur Urol 2003 44:637-49.10.1016/j.eururo.2003.08.01514644114 [Google Scholar] [CrossRef] [PubMed]
[7]. Seftel AD, De la Rosette J, Birt J, Porter V, Zartotsky V, Viktrup V, Coexisting lower urinary tract symptoms and erectile dysfunction: A systematic review of epidemiological dataIJCP 2013 67(1):32-45.10.1111/ijcp.1204423082930 [Google Scholar] [CrossRef] [PubMed]
[8]. Ngai KH, Kwong AS, Wong AS, Tsui WW, Erectile dysfunction and lower urinary tract symptoms: Prevalence and risk factors in a Hong Kong primary care settingHong Kong Med J 2013 19(4):311-16.10.12809/hkmj13377023603776 [Google Scholar] [CrossRef] [PubMed]
[9]. Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, Mckinlay JB, Impotence and its medical and psychosocial correlates: Result of the Massachusetts Male Ageing StudyJ Urol 1994 151:54-61.10.1016/S0022-5347(17)34871-1 [Google Scholar] [CrossRef]
[10]. Nwofor AME, Yeboa ED, Dogunro AS, Sidenafil Citrate (VIAGRA TM) in the treatment of Male Erectile Dysfunction. A 6 week Flexible Dose Evaluation of Efficacy and SafetyNig J of Health and Biomed. Sc 2002 1:45-48. [Google Scholar]
[11]. Shaeer KZM, Osegbe DN, Siddiqui SH, Razzaque A, Glasser DB, Prevalence of erectile dysfunction and its correlates among men attending primary care clinics in three countries: Pakistan, Egypt, and NigeriaInt J Impot Res 2003 15(1):08-14.10.1038/sj.ijir.390097112825103 [Google Scholar] [CrossRef] [PubMed]
[12]. Levinson IP, Khalaf IM, Shaeer KZM, Smart DO, Efficacy and Safety of Sidenafil Citrate (ViagraR) for treatment of erectile dysfunction in men in Egypt and South AfricaInt J Impot Res 2003 15(1):25-29.10.1038/sj.ijir.390097012825106 [Google Scholar] [CrossRef] [PubMed]
[13]. Burneeti AL, Nitric Oxide in the penis: Physiology and PathologyJ Urol 1997 157:320-24.10.1016/S0022-5347(01)65369-2 [Google Scholar] [CrossRef]
[14]. Kirby M, Chapple C, Jackson G, Eardley I, Edwards D, Hackett G, Erectile dysfunction and lower urinary tract symptoms: A concensus on the importance of co-diagnosisInt J Clin Pract 2013 67:599-600.10.1111/ijcp.1217623617950 [Google Scholar] [CrossRef] [PubMed]
[15]. Berrada S, Kadril N, Mechakra-Tahiri S, Nejjari C, Prevalence of erectile dysfunction and its correlates: A population-based study in MoroccoInt J Impot Res 2003 15(1):03-07.10.1038/sj.ijir.390096812825102 [Google Scholar] [CrossRef] [PubMed]
[16]. Aytac IA, Mckinlay JB, Krane RJ, The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequenciesBJU Int 1999 84:50-56.10.1046/j.1464-410x.1999.00142.x10444124 [Google Scholar] [CrossRef] [PubMed]
[17]. Mckinlay JB, The worldwide prevalence and epidemiology of erectile dysfunctionInt J Impot Res 2000 12:610.1038/sj.ijir.390056711035380 [Google Scholar] [CrossRef] [PubMed]
[18]. United Nations World Population Prospectus 1996. United Nations Population Division; New York: Department of Public Information Publications Department, 1997 [Google Scholar]
[19]. Braun MH, Sommer F, Haupt G, Mathers MJ, Reifenrath B, Engelmann UH, Lower urinary tract symptoms and erectile dysfunction: Co-morbidity or typical “Aging Male” symptoms? Result of the “Cologne Male Survey”Eur Urol 2003 44:588-94.10.1016/S0302-2838(03)00358-0 [Google Scholar] [CrossRef]
[20]. Boyle P, Robertson C, Mazzetta C, Keech M, Hobbs R, Fourcade R, The association between lower urinary tract symptoms and erectile dysfunction in four centres: The UrEpik studyBr J Urol Int 2003 92:719-25.10.1046/j.1464-410X.2003.04459.x14616454 [Google Scholar] [CrossRef] [PubMed]
[21]. Blanker MH, Bohnen AM, Groeneveld FP, Bernsen RM, Prins A, Thomas S, Correlation for erectile and ejaculatory dysfunction in older Dutch men: A community-based studyJ Am Geriatr Soc 2001 49:436-42.10.1046/j.1532-5415.2001.49088.x11347788 [Google Scholar] [CrossRef] [PubMed]
[22]. Aytac IA, Araujo AB, Johannes CB, Kleinman KP, McKinlay JB, Socioeconomic factors and incidence of erectile dysfunction: Findings of the longitudinal Massachusetts Male Aging StudySoc Sci Med 2000 51:771-78.10.1016/S0277-9536(00)00022-8 [Google Scholar] [CrossRef]
[23]. Elliot SP, Gulati M, Pasta DJ, Spitalny GM, Kane CJ, Yee R, Obstructive lower urinary tract symptoms correlate with erectile dysfunctionUrology 2004 63:1148-52.10.1016/j.urology.2004.01.03915183969 [Google Scholar] [CrossRef] [PubMed]
[24]. Araonye MO, Research methodology with statistics for health and social sciences 2004 1st editionOdo-Okun Sawmill Ilorin, NigeriaNathadex Publishers:115-121. [Google Scholar]
[25]. Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Pena BM, Development and evaluation of an abridged 5-item version of the International Index of Erectile Function (IIEF) as a diagnostic tool for erectile dysfunctionInt J Impot Res 1999 11:319-26.10.1038/sj.ijir.390047210637462 [Google Scholar] [CrossRef] [PubMed]
[26]. Barry MJ, Evaluation of symptoms and quality of life in men with BPHUrol 2001 5:25-32.10.1016/S0090-4295(01)01300-0 [Google Scholar] [CrossRef]
[27]. Hoesl CE, Woll EM, Burkart M, Altwein JE, Erectile dysfunction is prevalent, bothersome and underdiagnosed in patients consulting Urologists for Benign Prostatic Syndrome (BPS)European Urol 2005 47(4):427-68.10.1016/j.eururo.2004.10.02915774251 [Google Scholar] [CrossRef] [PubMed]