A New Non-touch Technique (Partha’s Technique) of Administering Spinal Anaesthesia in Paediatric Age Group- A Pilot Study
S Parthasarathy1, Indubala Maurya2
1 Professor, Department of Anaesthesiology, Mahatma Gandhi Medical College and Research Institute, Sri Balaji Vidyapeeth, Puducherry, India.
2 Assistant Professor, Department of Anaesthesia, Super Speciality Cancer Institute and Hospital, CG City, Lucknow, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. S Parthasarathy, Professor, Department of Anaesthesiology, Mahatma Gandhi Medical College and Research Institute, Puducherry, India.
E-mail: painfreepartha@gmail.com
Introduction
Paediatric spinal anaesthesia is often the technique of choice in many short duration surgeries. However, the failure rate is higher with spinal anaesthesia in children than in adults.
Aim
To evaluate if a non-touch technique of paediatric spinal anaesthesia can reduce anaesthetic failure.
Materials and Methods
A pilot study was done in 10 paediatric patients from January 2018 to July 2018 in Mahatma Gandhi Medical College and Research Institute, Puducherry, India. Ten children posted for infra-umbilical surgeries in the age group of 4-10 years were given a sedative premedication with a combination of Pethidine and Midazolam They were kept in lateral position with the back much inside the edge of the table so that there was a considerable space between the table edge and the baby. Identification of the L3-L4 space was done by touching the patient. The 25-gauge quincke needle was pricked and the hub was held with the hand in the table without touching the patient.
Results
The anaesthesia was successful with adequate level in all the patients; T8 in five patients and T10 in the other five patients. There were no significant side effects.
Conclusion
From this pilot study on 10 patients, it can be suggested that the novel non-touch Partha’s technique is feasible and more successful with absent failure rate when administering spinal anaesthesia in the paediatric age group.
Anaesthetic failure, Paediatric spinal anaesthesia, Sedation
Introduction
Spinal anaesthesia in paediatrics is effective and useful in children where general anaesthesia is thought to be with risks. Numerous indications of such procedure have come up in recent years. Still achieving a sedated non-moving child needs addition of inhalational agents or parenteral ketamine [1]. This produces added airway risks and needed additional skilled personnel. The failure rate of adult spinal anaesthesia ranges between 1-2% while the corresponding incidence in children [2] is around 4-11%. One of the causes of such higher incidence as we theorised was a patient moving during injection of the drug. The percentage of such a cause for failed spinal anaesthesia in children is so not far described in literature. In children, during administration of the drug during spinal anaesthesia, there is a discrepancy caused by needle length and the difficulty in holding the hub. It may be difficult to achieve a motionless dexterity in hub holding. Hence, a non-touch technique was devised where the patient was not touched during intrathecal drug administration. This was an initial pilot study done on only 10 patients where we followed this method (Partha’s technique) to administer successful spinal anaesthesia in paediatrics.
Materials and Methods
The first 10 paediatric patients in the age group of 4-10 years, whose parents accepted for a routine spinal anaesthetic with a different technique for an infra-umbilical surgeries were selected for the study. It was a pilot study with an already established anaesthetic technique with a minimal modification in administration. This study was just a feasibility study of a non-touch technique with an initial 10 patients. The study was done from January to July 2018 in Mahatma Gandhi Medical College and Research Institute, Puducherry, India, and the human research guidelines from the declaration of Helsinki were followed.
Any patient with local infection, spinal abnormalities, coagulation abnormalities were excluded. Oral Midazolam 0.5 mg/kg was given one hour before. After a sedation was established, the children were separated from parents, an intravenous access was established with ringer lactate on flow. Inj. Glycopyrrolate (0.1-0.2 mg), Inj. Pethidine (1 mg/kg) and an additional dose of Midazolam were administered intravenously. Pulse oximetry, Electrocardiogram, Non-invasive blood pressure with adequately sized cuff was used for monitoring all the patients. The patients were put on any lateral position without much flexion of the neck. The back of all the patients were not at the tip of the table as in adults [Table/Fig-1,2]. Spines and the L3-L4 interspinous space were felt. Injection 2% lignocaine was injected without touching the patient. After one minute, without touching the patient, 25-gauge spinal quincke needle was inserted in the designated L3-L4 interspace to get free flow of cerebrospinal fluid. With the inner side of the fist [Table/Fig-3], in the table, the hub was held and the hyperbaric bupivacaine was administered according to Partha’s formula [3], of paediatric spinal anaesthesia (Dose of hyperbaric bupivacaine in mL=Age/5 or Dose of hyperbaric Bupivacaine in mg equivalent to age). The onset meant that there was some sensory loss anywhere in the lower limb. Regression of level below two segments or onset of pain or vigorous movement of the lower limb was taken as duration from the time of administration of intrathecal anaesthetic drug.
Showing adults with patient at the tip of the table and dorsum of hand touching back (drawn by authors).
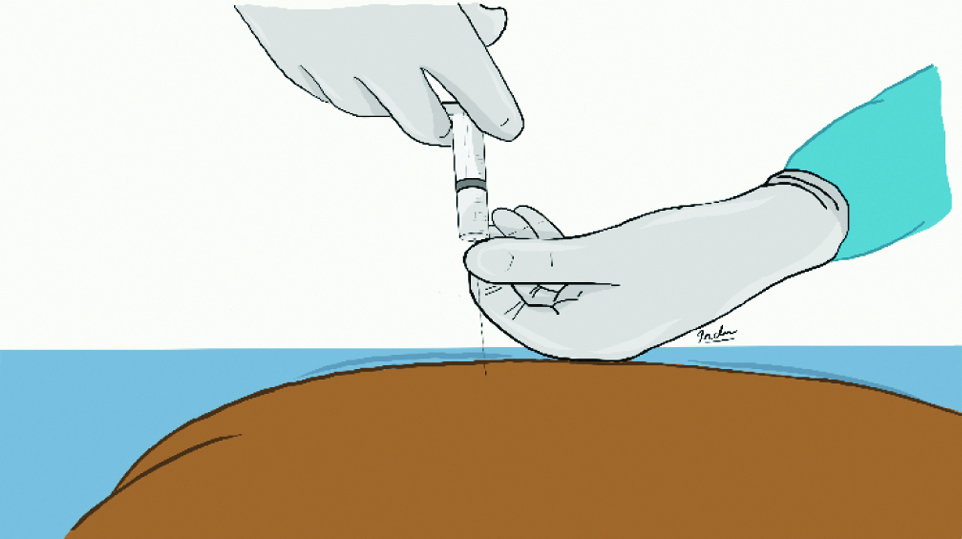
Showing children with table space (drawn by authors).
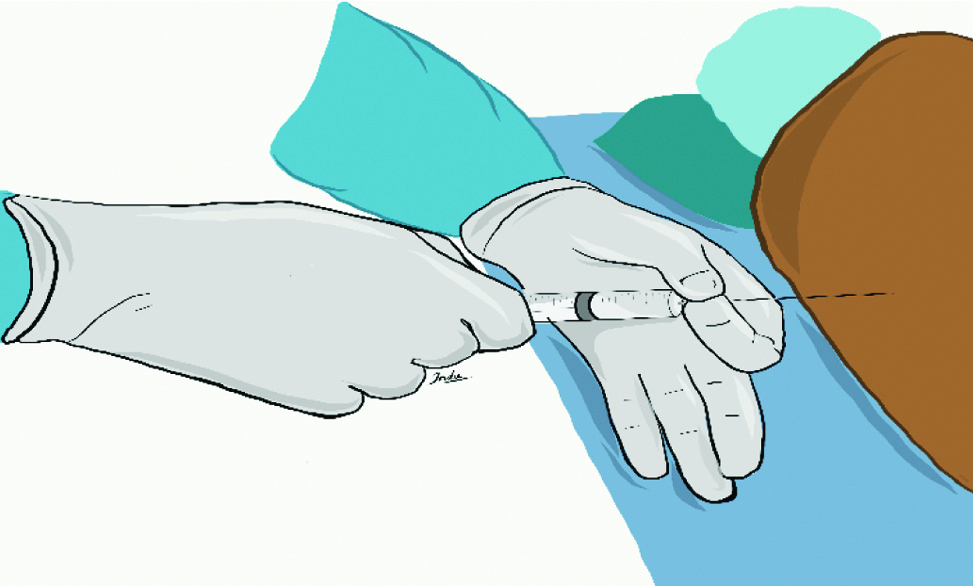
Showing the administration technique.

Routine monitoring, the onset, sensory level and the duration of action were noted. Any level below T12 was taken as failed spinal. All the other decisions regarding the additional sedatives or inhalational agents was decided by the attending anaesthesiologist and was noted. All side effects were noted.
Results
The onset of sensory block was instantaneous in all the cases. There was a fall in the lower limb which occurred within a minute in all the cases. The clear-cut demarcation between the onset of sensory and motor block was difficult to differentiate in this age group. There were no failure rates. All patients were given spinal anaesthesia in the first attempt with a single pass with two in three passes. No patient received either ketamine or inhalational agent for administering spinal anaesthesia. Hence, the sedation of the child was so precise that all the children responded to oral commands and were not unconscious. It was presumed that the technique used (Partha’s technique) may be responsible for this success with less sedation. There were no complications. There was no incidence of any hemodynamic imbalance. None of the children needed extra anaesthetics [Table/Fig-4].
Demographic data with anaesthesia details.
| S. no. | Age (years) | Sex | Surgery | Dose (mg) of Hyperbaric Bupivacaine | Onset | Level | Duration (minutes) | Other drugs |
|---|
| 1 | 4 | F | Orthopedic limb | 4 | Immediate | T10 | 60 | Nil |
| 2 | 8 | M | Orthopedic limb | 8 | Immediate | T10 | 60 | Nil |
| 3 | 10 | F | Orthopedic limb | 10 | Immediate | T10 | 75 | Nil |
| 4 | 8 | M | Herniotomy | 8 | Immediate | T8 | 60 | Nil |
| 5 | 5 | M | Herniotomy | 5 | Immediate | T8 | 60 | Nil |
| 6 | 6 | M | Orchiectomy | 6 | Immediate | T8 | 60 | Nil |
| 7 | 4 | M | Herniotomy | 4 | Immediate | T10 | 50 | Nil |
| 8 | 8 | F | Appendicectomy | 8 | Immediate | T8 | 60 | Nil |
| 9 | 5 | M | Urology | 5 | Immediate | T8 | 60 | Nil |
| 10 | 5 | F | Orthopedic limb | 5 | Immediate | T10 | 60 | Nil |
M: Male; F: Female
Discussion
Administration of spinal anaesthesia in children still remains an art. There are a lot of anatomical and physiological changes associated with its administration. The failure rate associated with its administration is more in children than in adults [4]. We believed that this extra incidence of failure may be due to movement of patients during the drug administration. This movement of the child can be prevented by making the patient more unconscious or by not touching the back of the child. No inhalational agent or anaesthetics were given in the present study and nil failure rate was achieved with this technique. Verma D et al., have described successful spinal anaesthesia in infants with two attempts [2]. No infants were included but the age group was a more uncooperative one. The description for adults is that intrathecal administration of the entire planned volume has been confirmed by avoiding needle movement by putting one handfirm against patient’s back, while attaching the syringe with the hub of the spinal needle. This is likely to make the child twist the hip and alter the position. Hence, this technique of no touch was suggested to ensure the full drug was inside the space.
Usually, adults are placed with the back in the tip of the table. We purposely avoided this so that there is some place on the table to rest the left hand. This ensured the tight fit of the needle and the syringe and the control of the hub. As the doses were precisely administered to get the needed level, added sedation was not required and there were no side effects.
The causes of failed spinal anaesthesia are well described in adults [5], while clear-cut problem-based approach in paediatrics is not published yet. Hence, this study attempted to counter one basic problem. Calm and a relaxed patient is more likely to assume and maintain the described position and it needs a gentle, unhurried handling even in adults for success in subarachnoid block. Hence in paediatrics, even a touch in the back may make the position incorrect. Thus, in present pilot study, we have established such a non-touch technique being very effective in administering spinal anaesthesia in children.
Limitation(s)
The study was limited to 10 patients and needs a larger sample size for further validation with controlled trials having established sampling methods.
Conclusion(s)
A novel non-touch Partha’s technique is easier, feasible and more successful with absent failure rate when administering spinal anaesthesia in the paediatric age group. As this being a pilot study, it needs comparative evaluation with established techniques.
M: Male; F: Female
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? No (an already established anaesthetic technique with a minimal modification in administration)
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 27, 2020
Manual Googling: Apr 24, 2020
iThenticate Software: Jun 24, 2020 (12%)
[1]. Gupta A, Saha U, Spinal anaesthesia in children: A reviewJ Anaesthesiol Clin Pharmacol 2014 30(1):10-18.10.4103/0970-9185.12568724574586 [Google Scholar] [CrossRef] [PubMed]
[2]. Verma D, Naithani U, Gokula C, Harsha Spinal anaesthesia in infants and children: A one year prospective auditAnaesth Essays Res 2014 8(3):324-29.10.4103/0259-1162.14312425886329 [Google Scholar] [CrossRef] [PubMed]
[3]. Parthasarathy S, Senthilkumar T, Age-based local anaesthetic dosing in paediatric spinal anaesthesia: Evaluation of a new formula- A pilot study in Indian patientsAnaesth Essays Res 2017 11(3):627-29.10.4103/aer.AER_246_1628928560 [Google Scholar] [CrossRef] [PubMed]
[4]. Tobias JD, Spinal anaesthesia in infants and childrenPaediatric Anaesthesia 2000 10:05-16.10.1046/j.1460-9592.2000.00460.x10632903 [Google Scholar] [CrossRef] [PubMed]
[5]. Fettes PDW, Jansson JR, Wildsmith JAW, Failed spinal anaesthesia: Mechanisms, management, and preventionBritish Journal of Anaesthesia 2009 102(6):739-48.10.1093/bja/aep09619420004 [Google Scholar] [CrossRef] [PubMed]