Case Report
A 23-year-old male patient was admitted from casualty department with complaints of severe generalised headache and photophobia since one week and four episodes of GTCS with post-ictal confusion and drowsiness since two days. Patient also had difficulty in recognising his relatives after an episode of GTCS. There was no history of hypertension, diabetes mellitus, tuberculosis, head injury, sinusitis, otalgia and diminution of vision, recent travel to any hill station or prolong flight. There was no other significant history. On examination: pulse-90/min regular, normal volume; BP-110/90 mmHg; no pallor, icterus, cyanosis, clubbing, no signs of meningeal irritation. On systemic examination: cardiovascular system, respiratory system and abdominal system were normal. He was conscious, oriented, having 4/5 power in right upper and lower limbs in all group of muscles, extensor plantar reflex in right foot and fundus examination showed no evidence of papilloedema.
MRI brain was done which was suggestive of left frontal region haemorrhagic venous infarct with superior sagittal sinus and cortical vein thrombosis. Investigations in the form of Complete Blood Count (CBC), Prothrombin time (PT), International Normalised Ratio (INR), activated Partial Thromboplastin Time (aPTT), liver, kidney and thyroid function test, Erythrocyte sedimentation rate, cerebrospinal fluid examination, antinuclear antibody, Antiphospholipid and anticardiolipin antibodies were performed and all were found to be normal. Further investigations to know the cause of CVT in young adult male were done, like Protein C, Protein S, anti-thrombin III and serum homocysteine level, which were also found to be within normal limits.
He was admitted in Intensive Care Unit (ICU) and anti-convulsant, antibiotic, mannitol and anticoagulation therapy in the form of Low Molecular Weight Heparin (LMWH) was started under strict monitoring of INR values. Patient improved over the period of five days. He was shifted on oral medications (warfarin, Diamox, amoxicillin-clavulanic acid and folic acid) in the ward.
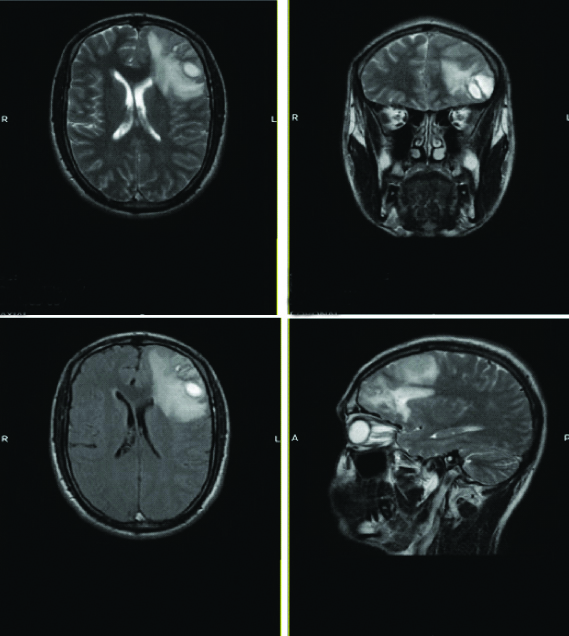
On day seven, patient complained of severe headache, for which urgent fundus examination was performed, which was suggestive of papilloedema in both eyes. Magnetic Resonance Imaging (MRI) with Magnetic Resonance Venography (MRV) brain was done, suggestive of left frontal region evolving haemorrhagic venous infarct with superior sagittal sinus and cortical vein thrombosis [Table/Fig-1].
MRI brain showing left frontal region evolving haemorrhagic venous infarct with superior sagittal sinus and cortical vein thrombosis.
Patient was shifted to ICU again and further investigations to address the aetiology of CVT were re-thought. As majority of other possible investigations had been done and patient belonged to sickle cell belt, he was tested sickling and Haemoglobin (Hb) electrophoresis. Late sickling came positive and Hb electrophoresis was confirmatory for sickle cell trait (Hb-AS) pattern.
Hydration in the form of intravenous fluids was increased. Dose of warfarin was increased from 5 mg to 7 mg as patient’s symptoms and findings were not improving, Syrup. Glycerol, Tab. Sodium bicarbonate and Tab. Hydroxyurea were added to treatment.
Patient’s condition improved during the hospital stay, headache and photophobia decreased and no seizure episode was recorded. He was discharged on day 14. Patient came for follow-up after one month and he was symptom free during this period and no new complaints were present.
Discussion
CVT or Cerebral Sinus Venous Thrombosis (CSVT) is a rare form of Venous Thromboembolism (VTE) [1,2]. It generally affects young population with female predominance [2,3]. But some studies reported the male predominance in last two decades in India [3-5]. The most common risk factor identified worldwide for VT is often a prothrombotic condition [3]. Unlike arterial strokes, it presents with extremely varied clinical presentations (headache being the most common), predisposing factors, imaging findings and outcomes and thus can be extremely challenging to diagnose [1,6].
Headache is associated with or without cranial nerve involvement (except for the olfactory nerve), seizures, signs of Intra Cerebral Haemorrhage (ICH), focal brain injury from venous ischemia/infarction or haemorrhage, or mix of them, papilloedema, diplopia, visual deficits, aphasia, altered mental state, and stupor or coma. Septic CVT presents with cephalea, fever and ophthalmoplegia, as orbital cellulitis is the most common cause of septic CVT [1,6].
Index patient had headache, seizures, signs of ICH and drowsiness. Later, he also developed papilloedema, but no cranial nerves were involved. Neuroimaging in the form of CT, MRI and MRV may be required for the diagnosis [1,6]. MRV is an excellent method of visualising the dural venous sinuses and larger cerebral vein [1,6].
To know the cause, CBC, PT, INR, aPTT, liver, kidney and thyroid function test, erythrocyte sedimentation rate, cerebrospinal fluid examination, antinuclear antibody, antineutrophil cytoplasmic antibodies, Antiphospholipid and anticardiolipin antibodies are done [2,3,6]. Sickling test and Hb electrophoresis should be performed for Sickle Cell Anemia (SCA) [6,7].
Even the sickle cell trait can present with crisis and thrombotic phenomenon [7]. In a study conducted by Khalid K and Patil MM, all female patients of sickle cell trait had developed crisis, with maximum numbers in the age group of 21-30 years, whereas 75% of SCA patients who had developed crisis were males [7]. In this case, CVT was diagnosed by MRI and rest of the investigations to establish the cause were normal except for the sickle cell trait.
Many authors have mentioned that sickle cell disease (SS pattern) is usually found to be associated with thrombotic phenomenon like CSVT [1,4,8,9]. But to the best of our knowledge, the association of CSVT with sickle cell trait (AS pattern) has not been reported in any literature yet.
Treatment of CSVT aims at reducing intracranial tension, thrombosis, headache and seizures in form of anticoagulant therapy (heparin unfractionated or low molecular weight followed by warfarin therapy for 3-6 months), anticonvulsants, NSAID’s, antioedema measures and haematoma evacuation or decompressive hemicraniectomy or thrombolytic therapy by using urokinase [1,8,9]. Whereas treatment options for sickle cell disease include hydroxyurea, folic acid, sodium bicarbonate, exchange transfusion and bone marrow transplantation, etc., [7,8].
As this was a case of sickle cell trait with CSVT so the patient was managed with adequate hydration, anticonvulsant, antibiotic, anticoagulation therapy (low molecular weight followed by warfarin therapy), antioedema measures and hydroxyurea.
Now-a-days, CSVT have a lower case fatality compared to arterial strokes [2,3]. Predictors of poor outcome include presence of fever, deep venous thrombosis, presence of multiple comorbidities and pro-thrombotic risks factors, uncontrolled seizures, prolonged unconsciousness and focal neurological deficits [2-4].
Conclusion(s)
SCA and even the sickle cell trait should be searched and sought routinely during evaluation of the case especially in India and Asian countries. This report documented a rare case of a young male with sickle cell trait (undiagnosed previously) presenting first time with CSVT and recurred within a week during hospital stay, successfully managed with hydration, antibiotics, antiepileptics, anticoagulants with hydroxyurea and sodium bicarbonate.
[1]. Bousser MG, Crassard I, Cerebral venous thrombosis, pregnancy and oral contraceptivesThromb Res 2012 130(1):S19-22.10.1016/j.thromres.2012.08.26423026652 [Google Scholar] [CrossRef] [PubMed]
[2]. Moscote-Salazar L, Alcala-Cerra G, Alvis-Miranda H, Castellar-Leones S, Cerebral sinus venous thrombosisJ Neurosci Rural Pract 2013 4(4):42710.4103/0976-3147.12023624347950 [Google Scholar] [CrossRef] [PubMed]
[3]. Dash D, Prasad K, Joseph L, Cerebral venous thrombosis: An Indian perspectiveNeurol India 2015 63(3):31810.4103/0028-3886.15819126053803 [Google Scholar] [CrossRef] [PubMed]
[4]. Narayan D, Kaul S, Ravishankar K, Suryaprabha T, Bandaru VC, Mridula KR, Risk factors, clinical profile and long-term outcome of 428 patients of cerebral sinus venous thrombosis: Insights from Nizam’s Institute Venous Stroke Registry, Hyderabad (India)Neurol India 2012 60(2):154-59.10.4103/0028-3886.9638822626695 [Google Scholar] [CrossRef] [PubMed]
[5]. Pai N, Ghosh K, Shetty S, Hereditary thrombophilia in cerebral venous thrombosis: A study from IndiaBlood Coagul Fibrinolysis 2013 24(5):540-43.10.1097/MBC.0b013e32835fad1e23518830 [Google Scholar] [CrossRef] [PubMed]
[6]. McElveen W A, Keegan A P, “Cerebral Venous Thrombosis.”Emedicine Medscape. Medscape, Updated Oct 09, 2018 Available from: https://emedicine.medscape.com/article/1162804-overview [Google Scholar]
[7]. Khalid K, Patil MM, Study of renal profile in patients of sickle cell diseaseInternational Journal of Scientific Research (IJSR) 2018 7(4):01-07. [Google Scholar]
[8]. Kassim AA, Galadanci NA, Pruthi S, DeBaun MR, How I treat and manage strokes in sickle cell diseaseBlood 2015 125(22):3401-10.10.1182/blood-2014-09-55156425824688 [Google Scholar] [CrossRef] [PubMed]
[9]. Yelwatkar S, Jain VV, Update on management of cerebral sinus venous thrombosis-Review ArticleJMGIMS 2012 17(2):13-16. [Google Scholar]