Health Strategies that could Boost Industrial Productivity in India Amidst the COVID-19 Crisis
Hemant Jain1, Kaushik Bharati2, Aarti Garg3, Sunanda Das4
1 Chief Editor, Journal of Clinical and Diagnostic Research, New Delhi, India.
2 Public Health Consultant, New Delhi, India.
3 Deputy Editor in Chief, Journal of Clinical and Diagnostic Research, New Delhi, India.
4 Senior Editor and Head of Editorial Services, Journal of Clinical and Diagnostic Research, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hemant Jain, No: 3, 1/9 Roop Nagar, G.T. Road, Delhi-110007, India.
E-mail: drhemantjain@jcdr.net
Corona, Economy, Industry, Prevention strategies
Introduction
The Coronavirus Disease-2019 (COVID-19) pandemic is currently wreaking havoc across the globe and has affected 213 countries and territories [1]. This has led to widespread lockdowns that are having a dramatic impact on the society, which has in effect, come to a grinding halt. The livelihoods of daily wage earners and deprived and underprivileged people from the economically weaker strata of society have been particularly affected.
Job cuts have become the norm and are likely to become much worse in the near future. For example, as per the data available from the Centre for Monitoring Indian Economy (CMIE) in Mumbai, unemployment reached the highest level of 27.1% in the week that ended on 3 May 2020. The wage labourers and small businesses have been worst hit by the lockdown. A staggering 90 million people in India lost their livelihoods within a span of just one month [2].
Impact of Lockdowns on Indian Industry
The lockdowns have led to a complete shutdown of many industries, which could jeopardise the Indian economy. However, some industries are in the process of being reopened in a phased manner during the current Lockdown 4.0. However, an industrialist known to the authors has highlighted the problems associated with operating a factory during the current COVID-19 crisis. As per the recommendations of the Ministry of Labour and Employment, Government of India, currently the maximum limit of industrial workers who can be employed is 33% of the total workforce [3]. However, he further added that the remaining 67% of employees would still need to be paid their full salary, despite the fact that they may not be working. This would greatly increase the financial burden of companies and could even lead to bankruptcy.
In order to troubleshoot these and other problems associated with reopening industries, representatives of 12 employer’s associations, including CII, FICCI and ASSOCHAM, interacted with the Labour Minister through video-conferencing to make some headway in the discussions [4].
In the meantime, Labour Law Reforms have led the Ministry of Home Affairs (MHA), Government of India to relax workplace norms, which is likely to benefit both the industries, as well as the workforce [2,5].
Health Strategies to Protect Industrial Employees
This editorial proposes some strategies from a health perspective to overcome some of the hurdles associated with re-opening factories and help industrialists to optimise their workflow. Some of these health strategies are discussed below.
Using Personal Protective Equipment (PPE) [
6]
Personal Protective Equipment (PPE) are protective gears designed to safeguard the health of employees by minimising the exposure to biological agents. Components of PPE include coveralls, goggles, face shields, masks, gloves and head covers.
Coveralls: Coveralls are designed to protect the entire body of an individual from exposure to chemicals or infectious agents, such as the current Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2), the causative agent of COVID-19. Coveralls provide 360-degree protection by covering not just the torso and limbs, but also the head and feet. Hence, potentially harmful pathogens are prevented from gaining entry into the body.
Coveralls that are currently being used by medical professionals for protection against SARS-CoV-2 infection, but are unlikely to be suitable for industrial purposes. Firstly, medical coveralls are made of non-woven materials, such as polyester or polyethylene, which makes the wearer feel very hot. Considering the fact that factories are naturally much hotter than medical settings, the heat inside the coverall is likely to be unbearable for the wearer, thereby drastically reducing work efficiency. Secondly, since these coveralls are disposable (single-use) and cost anywhere between INR 200 and INR 1,000, these would be much too expensive and therefore infeasible for use in industrial settings [7].
An alternative solution is to use coveralls that are specifically designed for industrial use. Firstly, these are made of woven materials, usually 100% cotton fabric, thereby appreciably reducing the temperature inside the coverall. Secondly, these are washable and therefore can be re-used, without having to discard after a single use. Moreover, these are also comparatively cheaper, with an average price ranging between INR 300 and INR 800 [8]. These combined factors, multiple-use and low cost, will significantly bring down the overall running cost of the factory. Images of typical medical and industrial coveralls are presented below [Table/Fig-1].
a) Medical coverall; b) Industrial coverall.
Goggles and face shields: SARS-CoV-2 is transmitted through airborne droplets and aerosols generated by coughing or sneezing of an infected individual. When these droplets/aerosols containing the infectious virus come in contact with mucous membranes of the eyes, nose and mouth, an unaffected person becomes infected. This is how the infection spreads in the community, similar in fashion to a chain reaction. Therefore, protecting the mucous membranes of the eyes, nose and mouth by wearing goggles and face shields can effectively stop the virus from entering the body. By way of design, the frame of the goggles should be flexible and provide a tight seal with the skin around the eyes and surrounding areas of the face.
N95 respirator masks: SARS-CoV-2 and other respiratory viruses mainly infect the upper and lower respiratory tracts. Therefore, preventing the entry of infectious droplets or aerosols into the respiratory tract can prevent infection. In this regard, the role of masks is crucial for halting transmission through the respiratory route.
The N95 respirator facemasks would be most effective for industrial employees. These masks are so called because they are ‘not resistant to oil’ (hence ‘N’) and filters out 95% of airborne particles (hence ‘95’). In case of factories where employees may be exposed to oil fumes, R95 masks, which are ‘resistant to oil’ would be better suited than N95 masks.
The very high efficiency of these facemasks is capable of protecting against respiratory droplet or aerosol-mediated transmission of the virus. These masks are designed in such a way that they are (i) close-fitting, (ii) provide good breathability due to fitted expiratory valves, (iii) possess a cup-shaped structure so that they don’t collapse against the mouth, (iv) possess nose clips to ensure a good seal and (v) have clearly demarcated inner and outer surfaces, so that the wearer doesn’t make any mistake while putting on the mask.
Gloves: If a person touches a surface contaminated with SARS-CoV-2 from an infected person, the virus can spread by inadvertently touching the eyes, nose or mouth. Here, gloves play a vital role in preventing viral transmission. Importantly, the gloves will not only provide protection against the virus, but also against industrial toxicants.
The type of gloves that should be used will vary according to the type of industry. Employees who perform tasks involving bulky machinery would need to wear heavy duty gloves that are hardy and resistant to wear and tear. However, in case of tasks that require fine dexterity, close-fitting rubber gloves akin to surgical gloves would be more suitable. Ideally, these should be made of nitrile, rather than latex. Nitrile gloves are more suitable because they are resistant to chemicals, including disinfectants such as chlorine. On the other hand, the major disadvantage of latex gloves is that they can cause allergic reactions in susceptible individuals due to contact dermatitis. Moreover, non-powdered gloves are more preferable than powdered gloves.
Head covers: Industrial coveralls generally don’t have a head cover. So, a separate head cover that covers the head and neck will be needed. It should be ensured that all the hair fits inside the head cover.
Practicing Personal Hygiene
Hand washing or hand sanitization: Adequate hand washing facilities and alcohol-based hand sanitizers should be made available to the employees, which should be used after taking off gloves, especially before eating. In this context, it may be mentioned that the lunchtime needs to be staggered over an extended period of time in order to prevent overcrowding of the canteen, so that social distancing measures are not compromised.
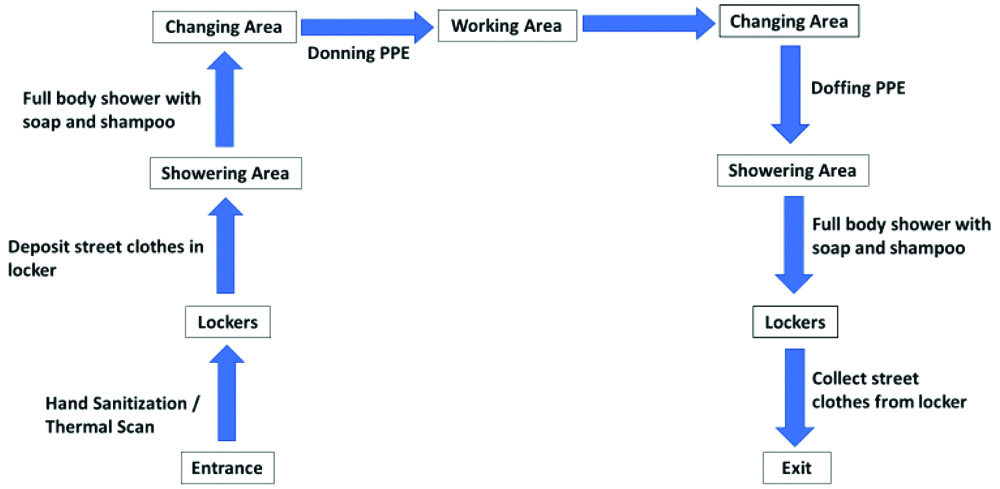
Showering: Showering facilities should be installed so that employees can take a shower before donning and after doffing PPEs, especially coveralls. Male and female employees should have separate showering areas. Personal lockers designated for each employee should be present for storing their clothes to prevent cross-contamination.
Other Strategies
Thermal scanners: Installation of thermal scanners or hand-held temperature monitors at the entry-point of the factory will play a vital role in screening employees for fever, which is a common primary symptom of COVID-19. A medical officer may be present for supervision.
Quarantining boxes containing consignments: Since COVID-19 can be transmitted by touching contaminated surfaces, it is important that the employees don’t unnecessarily touch packages. Packages and crates are generally made of cardboard and wood respectively. It has been scientifically proven that SARS-CoV-2 survives on cardboard for 24 hours and wood for up to 4 days [9]. Therefore, keeping packages under quarantine for the specified time period, would ensure that they are safe to handle and also alleviate the need for sanitization by spraying disinfectants.
In-house laundry facility: Since hygiene and sanitation are of the utmost importance for tackling COVID-19, the employee’s coveralls should be scrupulously cleaned after single-use. Hence, an in-house laundry facility should be available to carry out this vital task.
An overview of how the factory workers are expected to conduct themselves within the factory premises by maintaining the highest standards of personal hygiene is depicted in the flowchart [Table/Fig-2].
Flowchart showing the steps to be followed by factory workers.

Administration, Communication and safety
Administration, communication and safety issues should be handled by staff designated for the purpose, as highlighted below:
Administrative health officer: An administrative health officer should be appointed, who will be responsible for the overall supervision and smooth running of the facility. He will oversee the activities of the workers, as well as look after their general health and wellbeing. He will also dedicate his time for properly documenting the day-to-day activities in the factory. He will maintain a log book that will contain all information, pertaining to the daily functioning of the factory in minute detail, so that nothing is missed. This record will be proof that the factory is operating as per government norms and regulations. In case of any untoward incident, he will be answerable to the higher authorities. Moreover, if any litigations are filed against the factory, the onus will lie with him to tackle the associated legal issues.
Communication intermediary: A person should be appointed to act as an intermediary between the employees and the manager, who would monitor the progress of work remotely. The intermediary will don the same PPE that medical professionals wear, thereby offering maximal protection against the virus. Additionally, he will wear a helmet fitted with a camera, headphone and mouthpiece, by means of which he will be able to transmit all audio-visual data to the manager, who would be situated within the safety of his office. The importance of the intermediary lies in the fact that it relieves the manager to do his paperwork, without having to shuttle between the factory floor and his office. This would be a logistical nightmare as it would require repeatedly donning and doffing PPE as these are mandatory on the factory floor, while at the same time, unnecessary and impractical to wear within the office. Another added advantage of having an intermediary is that the manager could monitor the factory activities remotely through video, even from the comfort of his home, given the difficulty of commuting during the lockdown.
Safety officer: A safety officer should be appointed, who will be responsible for all occupational health and safety issues. Some of the areas that he will handle include management, monitoring, advising and reporting of all issues pertaining to the safety of all the employees. He will also be responsible for training of factory personnel through orientation programs so that they become more engaged and aware about safety issues at the workplace. Depending on the unit size and available resources, the safety officer and administrative health officer can be the same person. In this regard, one of the personnel from the Human Resource Department could take on this role.
Major Impediments in The Implementation of Protective Strategies
The two major impediments in implementation of the protective strategies are the cost and the size of the operating units.
Cost-factor: The cost-factor involved in implementing the protective measures could be a major impediment. However, in case of protection of employees against COVID-19, the investment will be worthwhile, as ‘all’ the employees can be employed at the same time, which would reduce running costs in the long-term. Moreover, it may be argued that industries invest heavily on fire-fighting equipment to ensure safety of its employees, then why not for COVID-19? Fire-fighting equipment doesn’t come cheap. In fact, a price analysis indicates that the cost of installation of fire sprinklers in India is approximately INR 2,500 per sq. feet. Also, fire extinguishers cost approximately INR 6,000 per piece. Besides these, there are additional costs for smoke detectors (INR 2,400 per piece) and alarm systems (INR 10,000 per piece), among other minor fire-fighting accessories [10].
With reference to COVID-19, another important health aspect needs to be kept in mind while deciding whether to invest in purchasing protective equipment. This is on the issue of rapid transmission of COVID-19. In the absence of protective gear, there is a real possibility that if a single employee becomes infected, then everyone could become infected due to working in close proximity. This could lead to closure of the factory, which would cause huge financial losses for the company.
Size of the operating units: The economic and human resource costs of this strategy may be easier to bear for very large units. However, the relative marginal costs associated with these measures can be onerous for micro, small and medium enterprises (MSME). Bathrooms and locker areas may pose problems for mid-size units (having around 50 workmen). Washing or sanitation areas may be difficult to carve out in small units with 30 or less workmen. These small and medium size units make up a large proportion of the labour and workforce and hence some innovation is required to scale these solutions down to their levels (perhaps by creating shared facilities for them or units pooling in resources to create such common complex). Government officials and regulators should aid the adoption of these measures and also provide incentives to smaller units for their implementation.
Major Benefits of Implementation of Protective Strategies
Alleviation of the need for social distancing: By ensuring that all protective measures are in place, all the employees will be able to work in close proximity without any danger of becoming infected. Therefore, these measures will ensure that stringent social distancing protocols will no longer be mandatory within the factory.
Optimal utilisation of workforce: The suggested protective measures will enable employers to utilise the maximal workforce. This will increase output by optimising the workflow. Moreover, this will mean lesser job cuts.
Profits: In the long-run, profits are likely to rise due to increase in productivity arising from utilisation of the full strength of the workforce.
Such precautions are not only going to help ward off risk of COVID-19 but will also work against other infectious diseases [11]. This will lead to a healthier workforce.
Conclusion(s)
It is quite evident that implementation of health interventions in Indian industries is likely to benefit all stakeholders- employers, employees and the Indian economy at large. Importantly, the major employer’s associations, including CII, FICCI and ASSOCHAM have suggested that the workforce should be increased from the existing 33% to 50%, upon reopening of the factories. The authors are optimistic that by implementing the health strategies highlighted in this editorial, it would be plausible to increase the workforce well above the 50% mark- may be even as high as 100%, thereby leading to workflow optimisation, increasing productivity, as well as helping to boost the Indian economy. Hence, this will be a “win-win” situation for everyone.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 19, 2020
Manual Googling: May 30 2020
iThenticate Software: Jun 08, 2020 (3%)
[1]. COVID-19 coronavirus pandemic. Worldometer. Available at: https://www.worldometers.info/coronavirus/; Accessed on 19.05.2020 [Google Scholar]
[2]. Are India’s labour law reforms only a gift for factories, or will workers benefit too? Available at: https://www.financialexpress.com/economy/are-indias-labour-law-reforms-only-a-gift-for-factories-or-will-workers-benefit-too-migrant-worker-up-coronavirus-lockdown-industry/1952368/; Accessed on 19.05.2020 [Google Scholar]
[3]. Lockdown-hit industry demands suspension of labour laws for 2-3 yrs. Available at: https://economictimes.indiatimes.com/news/economy/policy/lockdown-hit-industry-demands-suspension-of-labour-laws-for-2-3-yrs/articleshow/75633578.cms?from=mdr; Accessed on 19.05.2020 [Google Scholar]
[4]. Coronavirus lockdown: Suspend labour laws for 2-3 years, employers’ associations urge government. Available at: https://www.thehindu.com/news/national/coronavirus-lockdown-suspend-labour-laws-for-2-3-years-employers-associations-urge-government/article31537997.ece; Accessed on 19.05.2020 [Google Scholar]
[5]. Govt relaxes workplace norms for firms allowed to operate during lockdown. Available at: https://www.business-standard.com/article/economy-policy/govt-relaxes-workplace-norms-for-firms-allowed-to-operate-during-lockdown-120050101449_1.html; Accessed on 19.05.2020 [Google Scholar]
[6]. Novel Coronavirus Disease 2019 (COVID-19): Guidelines on rational use of personal protective equipment. Ministry of Health and Family Welfare, Government of India. Available at: https://www.mohfw.gov.in/pdf/GuidelinesonrationaluseofPersonalProtectiveEquipment.pdf; Accessed on 19.05.2020 [Google Scholar]
[7]. Hazmat suit, IndiaMARTAvailable at: https://dir.indiamart.com/impcat/hazmat-suit.html; Accessed on 02.06.2020 [Google Scholar]
[8]. Industrial coverall. IndiaMART. Available at: https://dir.indiamart.com/impcat/industrial-coverall.html; Accessed on 02.06.2020 [Google Scholar]
[9]. How long will coronavirus survive on surfaces? Cleveland Clinic, Ohio, USA. Available at: https://health.clevelandclinic.org/how-long-will-coronavirus-survive-on-surfaces/; Accessed on 20.05.2020 [Google Scholar]
[10]. Cost of fire-fighting equipment. IndiaMART. Available at: https://dir.indiamart.com/impcat/fire-fighting-equipments.html; Accessed on 20.05.2020 [Google Scholar]
[11]. Jain H, Bharati K, Garg A, Das S, Will the COVID-19 pandemic have a silver lining? An Indian perspectiveJ Clin Diagn Res 2020 14(5):AB04-AB07.Available at: https://www.jcdr.net/articles/PDF/13732/12624_F(SL)_PF1(AG_KB_SL)_GC(KB_SL)_PN(SL).pdf; Accessed on 08.06.2020 [Google Scholar]