DM is a complex metabolic disorder. Countries that account for the highest number of Diabetic patients are India (31.7 million) followed by China (20.8 million) and the United States (17.7 million) [1]. The latest estimates shows that global prevalence of Diabetes is expected to rise to 592 million by 2035 [2]. DM is characterised by chronic hyperglycaemia which affects many organs due to microvascular and macrovascular complications like neuropathy, retinopathy, nephropathy etc., [3].
The most commons manifestation of diabetic macrovascular complication is cardiovascular disease. Diabetic patients have 2- to 4-fold increased risk for developing coronary artery disease. The prevalence of microvascular complications in diabetic patients is seen commonly in people who suffer from this illness for chronic duration, patients with poor glycaemic control and when associated with other co-morbid conditions such as hypertension and obesity. The microvascular complications include retinopathy, nephropathy and neuropathy [4]. Increased risk of thrombotic complications is noted in diabetics and it is due to hyperglycaemia contributing to platelet hyperreactivity, hyperfibrinogenemia, increased thrombin formation and reduced fibrinolysis [5].
Diabetic patients are not routinely screened for assessing their thrombotic status. As a consequence, they usually approach clinician when they manifest with the complications after the organs are exposed to the brunt of the disease. In spite of the vigorous management, recovery of the damaged organs to normal is questionable.
Very few studies have compared the coagulation profile of diabetic patients based on HbA1c levels with contradictory results. The study conducted by Arpaci D et al., on diabetic patients belonging to regulated diabetic group (HbA1c <7.0) and dysregulated diabetic group (HbA1c ≥7.0), concluded that no significant differences were noted in PT, APTT and fibrinogen levels [6]. Bleeding time, platelet count and d-Dimer was not included in the study.
This study was conducted to compare the coagulation profile in patients with Type 2 DM with good glycaemic control (HbA1c <7.1) and poor glycaemic control (HbA1c ≥7.1) and to evaluate the association of coagulation profile and glycaemic control in diabetic patients.
Materials and Methods
A cross-sectional study was conducted in a SRM Medical College Hospital and Research Centre Potheri, Kancheepuram district Tamil Nadu, India on 84 Diabetic patients of which 42 patients with HbA1c <7 were considered as Group 1 and 42 patients with HbA1c ≥7 were considered as Group 2. This study was conducted between March 2018 to August 2019 after getting approval from SRM Institutional Scientific and Ethical committee (Ethical clearance number: 1380/IEC/2018).
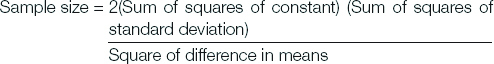
Sample size was calculated using the formula,
Inclusion criteria: HbA1c <7 is one of the glycaemic recommendations for non-pregnant adults with diabetes [7].
Good glycaemic control is defined as HbA1c <7.1 [8].
Hence, in this study, Diabetic patients with HbA1c <7 was considered as Group 1 and Diabetic patients with HbA1c ≥7 was considered as Group 2.
Exclusion criteria: Patients with septicaemia, bleeding disorders, liver disease, cancer, pregnancy, postoperative patients, Type 1 Diabetic patients and patients on anticoagulants were excluded from the study.
Under aseptic precautions, venepuncture was done and 5 mL of blood was collected from the individuals of both groups (1 and 2). Blood samples were analysed for coagulation profile including Bleeding Time, Platelet Count, PT, APTT, fibrinogen and d-Dimer.
Statistical Analysis
Statistical analysis was done by unpaired student’s t-test using SPSS 21.0.
Results
Total 84 patients were included in the study with 42 in each group (Group 1 and Group 2). The mean age of Group 1 was 52 and the mean age of Group 2 was 55. No significant variation was noted in the number of males and females included in each group [Table/Fig-1]. Pregnant women were excluded from the study. All females included in the study had uneventful history of pregnancy. No history of Diabetes or Hypertension was noted during the time of pregnancy. Significant changes were observed in Bleeding time, APTT and fibrinogen levels when the two groups were compared [Table/Fig-2].
The number of males and females in the study.
| Males | Females | p-value |
|---|
| Group 1-24 | Group 1-22 | 1.0 |
| Group 2-18 | Group 2-20 |
Comparison of bleeding time, platelet count, prothrombin time, activated partial thromboplastin time, fibrinogen and d-Dimer of Group 1 and Group 2.
| Group 1 (HbA1c <7) | Group 2 (HbA1c ≥7) | p-value |
|---|
| Mean | SEM | Mean | SEM |
|---|
| Bleeding time (sec) | 171.19 | 7.75 | 203.19 | 11.38 | 0.02 |
| Platelet count | 276295 | 20879.6 | 302869 | 18309.6 | 0.341 |
| PT test | 13.81 | 0.41 | 14.86 | 0.68 | 0.189 |
| aPTT test | 31.74 | 0.33 | 33.83 | 0.49 | 0.0007 |
| Fibrinogen | 277.08 | 11.17 | 358.11 | 12.69 | 0.0001 |
| d-Dimer | 560.01 | 12.55 | 675.34 | 16.11 | 0.86 |
SEM: Standard error of mean
Discussion
In DM, vascular endothelium, which is the primary defense against thrombosis is abnormal. The production of nitric oxide is inhibited in hyperglycaemia by blocking the activation of endothelial Nitric Oxide Synthase (eNOS) and also by elevated levels of reactive oxygen species, most commonly superoxide anion. The superoxide anion combines with nitric oxide to form peroxynitrite ion. Peroxynitrite decreases the production of prostacyclin which is a vasodilator. Increased production of free fatty acids from adipose tissue due to insulin resistance in turn leads to impairment of nitric oxide production [9].
Diabetes augments the capability of coagulation. Increased level of plasminogen activator inhibitor-1 leads to impaired fibrinolysis in Type 2 diabetes. Increased expression of tissue factor and coagulation factors along with decrease in endogenous anticoagulants such as protein C, antithrombin 3 is seen in diabetes. Thus, there is an increased tendency for coagulation combined with impaired fibrinolysis in patients with Type 2 diabetes [9].
The present study was aimed at comparing the coagulation profile between two groups of Type 2 Diabetic people, one with HbA1c <7 and the other with HbA1c ≥7 and to observe whether significant changes were noted in the coagulation profile among the two groups. The study was also aimed at whether HbA1c has a direct relationship with the coagulation profile.
Bleeding time was increased in Group 2 (203.19 sec) when compared to Group 1 (171.19 sec) and was statistically significant.
In this study, the mean platelet count was found to be increased in Diabetics in Group 2 (302869/cu.mm) when compared to Diabetics in Group 1 (276295/cu.mm) which was statistically insignificant. Variation in platelet count with increasing glycaemic levels were noted in a study done by Shetty A et al., [10]. The increase in platelet count is due to thrombopoietin and nitric oxide generated during diabetes [11]. In contrary, a study conducted by Kaur N et al., showed that platelet counts were not influenced by the glycaemic levels of the patient [12].
In this study, no significant changes in PT were noted between Diabetics in Group l (13.81 sec) and Diabetics in Group 2 (14.86). Arpaci D et al., observed that there was no significant difference in PT of people in regulated diabetic group (HbA1c ≤7.0%) and people in dysregulated diabetic group (HbA1c ≥7.0%). The mean PT in regulated diabetics in their study was 10.23±1.4 and dysregulated diabetics was 10.24±1.3 [6]. In contrary to this were the findings of Abdulrahaman Y and Dallatu MK, where PT was increased in untreated diabetics when compared to that of treated diabetics. The increase in PT is due to the conversion of inactive factor VII to active factor VII which triggers the extrinsic pathway [13].
Marked increase in aPTT was noted in diabetics in Group 2 (33.83 sec) when compared to Diabetics in Group 1 (31.74 sec). Mard-Soltani M et al., hypothesised in their study that decrease in factor VIII activity is the cause for prolonged aPTT. aPTT indicates the integrity of intrinsic pathway [14]. Factor VIII is a cofactor for factor IXa in intrinsic pathway, hence decrease in factor VIII could alter aPTT. Endothelial abnormalities in diabetes contribute to increase in factor VIII. Abdulrahaman Y and Dallatu MK in their study observed that there was marked increase in aPTT levels (58.460±4.146) in untreated diabetics when compared to treated diabetics (43.260±5.587) and non-diabetic controls (41.380±4.295) [13].
In this study, it was observed that patients in Group 2 have increased fibrinogen levels (358.11 mg/dL) than diabetics in Group 1 (277.08 mg/dL). Dhawale S et al., observed that serum fibrinogen levels were significantly increased in diabetic patients having high HbA1c levels. It was observed in their study that serum fibrinogen level increased progressively with increase in HbA1c level [15]. Arpaci D et al., observed no significant increase in fibrinogen levels among people in regulated diabetic group (323.42 mg/dL) and people in dysregulated diabetic group (342.36 mg/dL) [6]. Sapkota B et al., hypothesised that in diabetes free radicals activate thrombin formation, so oxidative stress may be a possible link between hyperfibrinogenaemia and diabetes [16].
In this study, among the diabetic people, there was no significant variation in d-Dimer levels of patients in Group 1 (560.01 ng/mL) and Group 2 (675.34 ng/mL). Nwose EU et al., in their study observed that plasma d-Dimer levels showed a gradual increase based on the progression of prediabetes to diabetes and to diabetes with complications. The increased levels of d-Dimer are attributed to increased formation of fibrin clot and its breakdown [17].
Limitation(s)
The variations in the coagulation test results (Platelet Count, PT, aPTT, Fibrinogen, d-Dimer) observed among the studies could be due to differences in the sample size, race and geographical region. The exact reason for the contradiction among different studies is not known. Follow-up of the patients and the development of microvascular and macrovascular complications could not be done due to irregular hospital visits by the patients.
Conclusion(s)
The present study showed that, among the diabetic people, those with HbA1c ≥7 revealed marked variations in coagulation profile when compared to Type 2 Diabetics with HbA1c <7. Consistent changes were noted in aPTT, fibrinogen and Bleeding Time in relationship to glycaemic levels which shows that these tests should be given priority in diabetic patients who suffer from the disease for long period of time. Increase in Bleeding Time and aPTT shows the increased tendency for haemorrhagic complications and increased fibrinogen levels point towards thromboembolic complications.
To reduce the incidence and prevalence of vascular burden and to improve the quality of life, in Type 2 Diabetic patients, coagulation profile should be considered as one of the routine screening test in diabetic patients.
SEM: Standard error of mean