Effectiveness of the Greater Palatine Nerve Block for Anaesthetising Anterior Palate: A Prospective Study
Gopinath Thilak Parepady Sundar1, Tripthi Prakash Shetty2, Bhanuprakash Bylapudi3, Vikram Shetty4, Chrysl Castellino5, Ashish Rai6, Arvind Karikal7, Pratiksha Shetty8
1 Reader, Department of Oral Surgery, A B Shetty Memorial Institute of Dental Sciences, Mangalore, Karnataka, India.
2 Reader, Department of Oral Surgery, A B Shetty Memorial Institute of Dental Sciences, Mangalore, Karnataka, India.
3 Clinical Observer, Department of Head and Neck Oncology, Apollo Cancer Institutes, Hyderabad, Telangana, India.
4 Professor, Department of Oral Surgery, A B Shetty Memorial Institute of Dental Sciences, Mangalore, Karnataka, India.
5 Assistant Professor, Department of Oral Surgery, Father Muller Hospital, Mangalore, Karnataka, India.
6 Reader, Department of Oral Surgery, A B Shetty Memorial Institute of Dental Sciences, Mangalore, Karnataka, India.
7 Professor, Department of Oral Surgery, A B Shetty Memorial Institute of Dental Sciences, Mangalore, Karnataka, India.
8 Reader, Department of Oral Surgery, A B Shetty Memorial Institute of Dental Sciences, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Tripthi Prakash Shetty, Department of OMFS, 6th Floor, A B Shetty Dental College, Derlakatte, Mangalore, Karnataka, India.
E-mail: tripthisurgeon@gmail.com
Introduction
Local Anaesthesia (LA) is the mainstay of any routine dental extraction. Accomplishing optimum anaesthesia with least pain and anxiety to patients is a challenge. Hence, modification of technique and application of routine dental LA to enhance patient comfort is the need of the hour. In this pursuit, a prospective cohort study was carried out to evaluate the effectiveness of greater palatine nerve block as an alternative to nasopalatine nerve block in anaesthetising the anterior palatal mucosa and to achieve optimum palatal anaesthesia.
Aim
The primary outcome variable is to assess the extent of the anaesthetic effect of greater palatine nerve block in maxillary anterior palatal region.
Materials and Methods
A total of 100 patients scheduled for the extraction of ipsilateral anterior and posterior maxillary teeth were included in this prospective study between June 2017 to June 2019. Palatal anaesthesia for all the extractions done was achieved only with greater palatine nerve block. After an interval of five minutes, the extent of palatal anaesthesia from the posterior palatal tissue to the anterior region was evaluated for both subjective and objective symptoms. Pain on the palatal mucosa was assessed using Numerical rating scale of 0-10. Post-evaluation, depending on the proposed tooth of extraction, buccal anaesthesia was achieved with Posterior superior alveolar nerve block for posterior teeth and infraorbital nerve block for anterior teeth.
Results
Of the 100 patients administered with greater palatine nerve block, it was observed that in 36 patients (36%) had effectiveness in anaesthesia till central incisor, 28 (28%) patients had effectiveness in anaesthesia till lateral incisor, 20 (20%) patients had effective in anaesthesia till the canine and 16 (16%) patients anaesthetic effects were limited to posterior teeth. Overall, 84% had varied degree of positive anterior anaesthesia with greater palatine nerve block alone.
Conclusion
Greater palatine nerve block was effective in providing anaesthesia to the posterior region till the premolars, with the extended complete anaesthesia in the anterior region with similar action as the nasopalatine nerve block administered to anaesthetise the anterior palate for extraction of the anterior teeth.
Exodontia, Lignocaine, Local anaesthesia, Palatal anaesthesia
Introduction
Local Anaesthesia (LA) plays a prime role in controlling oro-facial pain during any minor surgical procedure. LA agents have been introduced for pain control with different composition and systemic effects. They prevent the eliciting and conduction of nerve impulses by setting up a chemical roadblock between the source of impulse and the brain [1].
Tooth extraction is a skillful procedure, where the dental surgeon should be able to manage the patient’s perception of pain as well as be well-trained in the techniques of administration of LA and exodontia. A failure in LA block can be defined as inadequate depth and/or duration of anaesthesia to begin or to continue a dental procedure [2]. Various techniques of injecting LA have been followed with good success rates. However, it is said to be painful in certain anatomical areas in the oral cavity, especially the nasopalatine region [3].
The Nasopalatine nerve traverses through the incisive foramen to supply palatal mucosa. Its distribution varies in extent in different subjects, but always includes the gingival margins of the central incisors and the incisive papilla. In some individuals, the receptive field of the nasopalatine nerve extended back as far as the first premolar teeth [4]. The relationship of Nasopalatine Nerve with anterior (Greater) Palatine nerve, as well as its course and innervations has always been debatable [5].
The greater palatine nerve is the principle branch supplying the hard palate. It emerges onto the hard palate through the greater palatine foramen and transverses in a groove almost up to the incisor teeth where it communicates with the terminal filaments of the nasopalatine nerve [6].
Nasopalatine nerve blocks are infamous as very painful and technique sensitive block. In routine dental practice, anaesthetic solutions are injected into tissues of widely varying distensibilities under a variety of pressures. In an extensive study done by Pashley EL et al., showed highest maximum injection pressures in incisive papilla (18,224 mmHg) in comparison to hard palate (11,322 mmHg) [7]. Nasopalatine nerve block produces significantly more severe pain when compared to the anterior local infiltration and greater palatine nerve block [3].
The administration of such blocks could also distress the dental surgeon leading to use of alternative measures like infiltration with multiple pricks. A modification in the nerve anaesthesia will help to prevent excess pain and increases the success in overall pain management.
The goal of this study was to evaluate the effectiveness of the greater palatine nerve block as an alternative to nasopalatine nerve block in anaesthetising the anterior palatal mucosa and to achieve optimum palatal anaesthesia for anterior tooth extraction.
Materials and Methods
This prospective study involved 100 patients indicated for extraction of the ipsilateral anterior and posterior maxillary teeth (N=100) who had presented to the Oral and Maxillofacial Surgery unit at AB Shetty Memorial Institute of Dental Sciences Mangalore, Karnataka, India between June 2017 to June 2019 after obtaining proper approval from Institutional Ethics Committee (Approval number: ABSM/EC10/2016). A pilot study was done which found that greater palatine nerve block lead to anterior region anaesthesia in 50 percent of the subjects. Based on this, sample size estimation was done. Out of the initial 100 patients recruited for the study, six of them were excluded as they underwent an additional minor surgical procedure (Alveoplasty). Therefore, a further six patients were included in the study. The minimal number of teeth planned for extraction was one from posterior region (molars or premolars) supplied by greater palatine nerve and one from anterior region (canine and incisors) supplied by nasopalatine nerve. If the patient gave consent for multiple extractions in requirement of complete denture then multiple teeth from the anterior as well as posterior region ipsilaterally were planned. The sequence of extraction proceeded from posterior most teeth first followed by anterior teeth.
Inclusion criteria: Patients above 18 years of age requiring extraction of anterior and posterior maxillary teeth of the same quadrant were included in the study.
Exclusion criteria: Patients requiring extraction of maxillary anterior teeth only or mandibular teeth or other minor surgical procedures and patients with neurological diseases, psychiatric problems, history of drug allergy, moderate to severe uncontrolled systemic conditions which required close observation and follow-up were excluded from the study.
All extractions were done by a single well-qualified oral surgeon, having good knowledge and skill in nerve block techniques and exodontia. Informed consent was taken from the patients before subjecting them to LA.
After positioning and draping the patient, the greater palatine foramen was palpated and the area was cleaned and dried with sterile gauze. A 2% Lignocaine gel (LOX-2% Gelly) was applied with a cotton swab at that region. After two minutes of topical anaesthetic (Lidocaine topical Aerosol USP 15%, ICPA) application, 0.4 ml of 2% lignocaine with 1:80,000 Epinephrine (LIGNOX 2% A, Indoco remedies Ltd.,) was injected using a 25-gauge short needle (DISPO VAN 2ml) from the opposite side of mouth to block the Greater Palatine nerve.
After an interval of five minutes, the anaesthetic effect on the palatal region from the last molar to the anterior most teeth was examined for each tooth with a Molts No: 9 periosteal elevator. The patients were examined for positive objective symptoms. Pain on the palatal mucosa was assessed using Numerical rating scale [8] of 0-10, (NRS; scale 0-10; 0=no pain, 5=moderate pain, 10=worst possible pain) as a tool for measuring its severity. NRS above 3 in any of the patients was administered with nasopalatine nerve block for the removal of the proposed anterior teeth.
Depending upon the effectiveness of anaesthesia on the palatal region reflection of the soft tissue could be carried out. A score of 0-3 was considered to be effective block; the score above 3 could elicit moderate pain during reflection referring to the failure of adequate anaesthesia. In such case where the effectiveness was questionable, the nasopalatine nerve block was carried out to further anaesthetise the anterior palate. Accordingly, 4 patients requiring central incisor extraction, 2 patients requiring lateral incisor extraction and one patient requiring canine extraction had to be supplemented with nasopalatine nerve block.
Once palatal anaesthesia was evaluated and recorded, infraorbital & posterior superior nerve block were then administered to block buccal tissues depending on the teeth indicated for removal. There were no additional blocks administered in the palatal region.
Results
The study population consisted of 100 patients (45 males and 55 females) with mean age of 52 years, underwent extraction of anterior and posterior maxillary teeth of the same quadrant.
For the palatal anaesthesia only greater palatine nerve block was administered without blocking the nasopalatine nerve. Posterior superior nerve block, infraorbital or buccal field block was administered to anaesthetise the buccal tissues for posterior and anterior teeth respectively. A total of 119 anterior teeth and 143 posterior teeth were extracted.
Out of the 100 patients administered with greater palatine nerve block, it was observed that in 36 patients, the anaesthetic effect of the greater palatine nerve block extended up to the distal papilla of central incisors thereby anaesthetising the central incisors, lateral incisors, canines, premolars and molars of that side. The anaesthetic effect extended till lateral incisors in 28 patients and till canines in 20 patients. Anaesthetic effect was limited up to premolars and molars in 16 patients [Table/Fig-1].
Pictorial representation of extent of the anaesthetic effect of greater palatine nerve block.
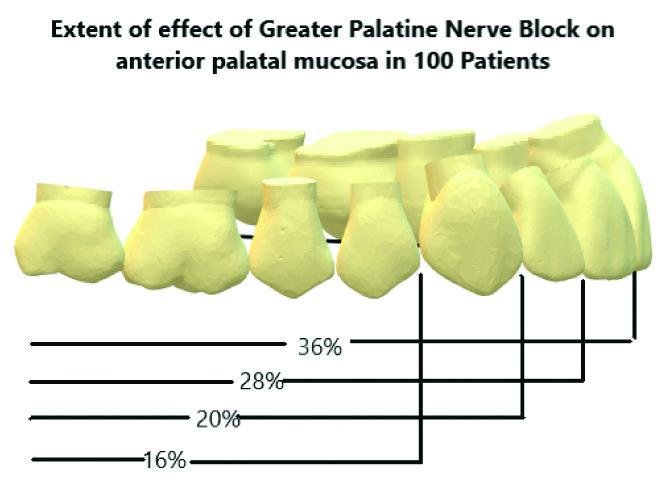
All the 100 patients (100%) had effective posterior palatal anaesthesia after administration of the greater palatine nerve block. In only 16% of the cases the greater palatine block couldn’t supply the anterior palate required for anterior tooth removal. The remaining 84 patients (84%) had effective anterior anaesthesia.
Discussion
Safe and effective pain control is essential for today’s dental practice. Our current techniques for delivery of LA to the maxilla and mandible are usually adequate for most clinical situations [9]. The maxilla is considered to be porous when compared to the more cancellous and denser mandible. Hence, maxillary nerve blocks have been very effective in providing complete anaesthesia when compared to the mandibular nerve blocks. The operator can manipulate the techniques by administering infiltrations or field blocks in the maxillary arch due to high absorption rate that adds to the painless extraction of the teeth [10].
Nerve block or infiltration in the palatal region is proven to be painful due to the close proximity of the mucosa to the bone. As per literature [11], the greater palatine and nasopalatine nerve blocks are considered to be effective for the complete anaesthesia of the palate. The patient’s perception to pain is twice in nasopalatine nerve block when compared to the greater palatine nerve block. The nasopalatine nerve block is considered to be more technique sensitive compared to the greater palatine nerve block. The relationship of the incisive papilla with respect to the central incisors and the angulation of the canal make this block more difficult. This has led to the improper usage of the technique in the form infiltrations or painful removal [10].
The results of the present study showed that, in 64 out of 100 patients considered for the study, the greater palatine nerve block successfully anaesthetised the anterior and posterior teeth including the lateral incisors, canines, premolars and molars. In 36 patients, it was observed that the anaesthetic effect of the block had extended even more anteriorly till the distal papilla of central incisors.
It was also observed that the anaesthetic effect did not reach till the interdental papilla between the two central incisors in any of the patients which may be because of the contralateral nerve supply from the opposite side. This is later confirmed in one patient, in whom bilateral greater palatine nerve blocks were administered as the patient needed bilateral teeth removal. The papilla between the central incisors was successfully anaesthetised when the block was administered bilaterally.
This study has confirmed the extended action of greater palatine nerve block in providing anterior palatal anaesthesia by anaesthetising till the anterior most area of the palate that is the central incisor.
Limitation(s)
The sample size was small and renders potential for further studies with bigger sample size.
Conclusion(s)
The outcome of this study is to update and revise the techniques in exodontia for the benefit of the clinicians who have to administer multiple injections. It could also decrease the need for painful nasopalatine blocks by substituting it with a more comfortable greater palatine nerve block. This study highlights that greater palatine nerve block is similar to nasopalatine nerve block in anaesthetising the anterior palate and provides the desirable anterior palatal anaesthesia.
Adopting this practice can benefit patient compliance as well operative ease for the clinician. The trend towards evidence-based dentistry dictates that our techniques and therapies are grounded on sound clinical experiences whenever possible. However, when electing to improve his or her local anaesthetic arsenal, the clinician must be knowledgeable and clinically accurate to obtain the desired results.
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jan 17, 2020
Manual Googling: May 07, 2020
iThenticate Software: Jun 10, 2020 (9%)
[1]. Covino BG, Vassallo HG, Local Anaesthesia mechanism of action and clinical use 1976 New YorkGrune & Stratton [Google Scholar]
[2]. Alam MN, Chandrasekharan SC, AMSA (Anterior Middle Superior Alveolar) Injection: A boon to maxillary periodontal surgeryJournal of Clinical and Diagnostic Research 2011 5(3):675-78. [Google Scholar]
[3]. Aminabadi NA, Farahani RMZ, Oskouei SG, Site-specificity of pain sensitivity to intraoral anaesthetic injections in childrenJournal of Oral Science 2009 51(2):239-43.10.2334/josnusd.51.23919550092 [Google Scholar] [CrossRef] [PubMed]
[4]. Langford RJ, The contribution of the nasopalatine nerve to sensation of the hard palateBr J Oral Maxillofac Surg 1989 27(5):379-86.10.1016/0266-4356(89)90077-6 [Google Scholar] [CrossRef]
[5]. Fitzpatrick TH, Downs BW, Anatomy, Head and Neck, Nasopalatine NerveStatPearls [Internet] 2020-2019 Feb 6 Treasure Island (FL)Stat Pearls Publishing [Google Scholar]
[6]. Sharma NA, Garud RS, Greater palatine foramen – key to successful hemimaxillary anaesthesia: A morphometric study and report of a rare aberrationSingapore Med J 2013 54(3):152-59.10.11622/smedj.201305223546029 [Google Scholar] [CrossRef] [PubMed]
[7]. Pashley EL, Nelson R, Pashley DH, Pressures created by dental injectionsJ Dent Res 1981 60(10):1742-48.10.1177/002203458106001003016944338 [Google Scholar] [CrossRef] [PubMed]
[8]. Katz J, Melzack R, Measurement of painSurg Clin North Am 1999 79(2):231-52.10.1016/S0039-6109(05)70381-9 [Google Scholar] [CrossRef]
[9]. Blanton PL, Jeske AH, Dental local anaesthetics: Alternative delivery methodsJADA 2003 134(2):228-34.10.14219/jada.archive.2003.014012636129 [Google Scholar] [CrossRef] [PubMed]
[10]. Malamed SF, Handbook of local anaesthesia5th editionELSEVIER [Google Scholar]
[11]. Monheim LM, Local anaesthesia and pain control in dental practice 1969 ed 4St LouisMosby [Google Scholar]